Globally, populations are rapidly aging. The worldwide population of individuals aged 65 and older reached 761 million in 2021, and this number is expected to double and surpass 1.6 billion in 2050 [
1]. In the European Union, over 94 million people are aged 65 and older, whereas in the United States, this number exceeds approximately 55 million. Japan has over 37 million people aged 65 and older, which accounts for 28.4% of the total population, and in China, this number exceeds 185 million [
2]. The number of people aged 65 and older is projected to grow the fastest in Northern Africa, Western Asia and sub-Saharan Africa in 2050 [
1]. The population of individuals over the age of 80 is also predicted to grow worldwide. The WHO defines a super-aged society as the proportion of the population aged 65 and over exceeding 21%. Preparations for an expected super-aged society is crucial not only from the perspectives in medical system and healthcare, but also from socio-economic perspectives.
Elderly individuals often have multiple underlying diseases or comorbidities. The coexistence of diabetes mellitus (DM) [
3,
4], heart failure [
5,
6], and chronic kidney disease (CKD) [
7,
8,
9] is frequently observed in the elderly. These diseases and stroke are interrelated [
10]. Stroke is a leading cause of adult disability [
11,
12], and multidisciplinary rehabilitation are needed for severe stroke patients [
13]. Comorbidities are observed in approximately 60% of elderly individuals and are related to a worsened prognosis and decreased quality of life (QOL) [
14].
As aging population has progressed, the number of individuals with dementia is also increasing [
31]. Dementia is a complex of diseases, including Alzheimer’s disease [
32] and vascular dementia [
33]. Typical symptom of dementia is loss of memory, language, problem-solving and other thinking abilities. Concomitant heart failure [
34], CKD [
35], and diabetes mellitus with poor glycemic control [
36] are at risk of developing dementia. Dementia causes severe disability [
12], and has significant impacts on patients, families, communities, and medical system and healthcare [
37,
38].
2. Can Nutrition Contribute to a Reduction in Sarcopenia, Frailty, and Comorbidities in a Super-Aged Society?
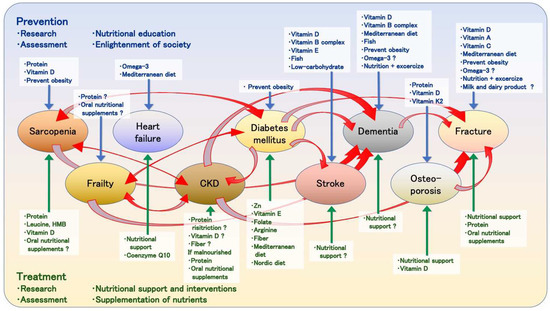
Researchers provide an overview of the literatures to determine whether nutrient deficiencies relate to the risk of diseases and whether nutrient intake can prevent the onset of diseases or enhance treatment outcomes (
Figure 1). Malnutrition and nutrient deficiencies have been associated with an increased risk of CKD [
90,
91,
92,
93], stroke [
157,
158,
159], osteoporosis [
193,
194], fractures [
229,
230,
231], and dementia [
183,
184,
185,
186]. Nutritional interventions can reduce the risk and improve the prognosis of these diseases [
97,
98,
99,
193,
232,
233,
234,
235,
236,
237].
Figure 1. Relationship between diseases and nutrients. The upper part of the figure indicates the involvement of nutrients in prevention, and the lower part indicates their involvement in treatment. Nutrients written in blue letters with blue arrows indicate that the nutrients are involved in prevention of diseases. Nutrients written in green letters with green arrows indicate that the nutrients are involved in the treatment of the diseases. The red arrows indicate the relationship between diseases.
Although a consensus on nutritional management for sarcopenia and frailty has not been established, numerous studies have been conducted on this topic [
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76,
77,
78,
94,
95,
96,
121,
124,
126,
127,
128,
129,
164,
165,
222,
223,
226]. The need for oral nutritional supplements to reduce sarcopenia [
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72] and frailty [
53,
73,
74,
75,
76,
77,
78] is still controversial. According to The European Society for Clinical Nutrition and Metabolism guidelines on clinical nutrition and hydration in geriatrics [
238], “Older persons with malnutrition or at risk of malnutrition with chronic conditions shall be offered oral nutritional supplements when dietary counseling and food fortification are not sufficient to increase dietary intake and reach nutritional goals”. This indicates the importance of the appropriate usage of oral nutritional supplements.
Protein supplementation may have potential benefits when it comes to malnutrition in CKD patients [
97,
98,
99], in preventing osteoporosis [
193], and treating hip fractures in the elderly [
232,
233,
234,
235,
236,
237]. Although a consensus has still not been reached, it is important to note that protein intake may need to be restricted in CKD patients to preserve renal function [
100,
101,
102,
103]. Considering that CKD is not uncommon in the elderly individuals, the protein intake of elderly individuals needs to be carefully evaluated. Leucine and HMB are effective in reducing sarcopenia [
42,
43,
44,
45,
46,
47,
48,
57]. HMB can be used without increasing the nitrogen load in CKD patients.
Preventing a vitamin D deficiency and supplementing it may have potential benefits with regard to reducing sarcopenia [
65,
66] and stroke risk [
146,
147], preventing decreased bone density [
195,
198,
199], and lowering fracture risks [
215,
216,
217,
218,
219,
220]. Although the effectiveness of vitamin D supplementation at managing mineral bone disorders in CKD patients has not been demonstrated [
110,
111,
112], they are relatively safe, and may be practically considered for their potential to improve glycemic control, lipid profiles, and inflammation [
113]. Vitamin D is also being investigated for its potential association with lowering risk of developing dementia [
168,
169,
170].
Evidence of malnutrition in patients with diabetes mellitus is limited [
116,
117,
118,
119,
120,
121,
122,
123], although scholars have suggested associations between diabetes mellitus and sarcopenia [
121,
123,
124,
125,
126,
127,
128,
129] and frailty [
120]. Appropriate management procedure for malnutrition in diabetes mellitus patients has not still been established. Zn [
130,
131], vitamin E [
132], folate [
133], and L-arginine [
134,
135] supplementation and fiber-rich diets [
136] have been suggested to potentially improve blood glucose control and insulin resistance. The reason why L-arginine improved glycemic control and insulin resistance is not clear in detail. L-arginine is a precursor for nitric oxide (NO) production by NO synthetase (NOS), and asymmetric dimethylarginine (ADMA) is a competitive inhibitor of NOS [
239]. Elevated asymmetric dimethylarginine levels in diabetes mellitus patients correlate with the development of microangiopathies, including retinopathy and nephropathy [
240]. L-arginine also stimulates insulin secretion from β-cells [
241]. These properties may lead to improved glycemic control in diabetes mellitus patients. However, the evidence for this topic remains insufficient.
The Mediterranean diet has the potential in preventing heart failure [
87,
89], the impairment of glycemic control in diabetes mellitus patients [
137,
138,
141], dementia [
174,
175], and fractures [
206,
207]. Omega-3 fatty acids, which is abundant in fish oil, may be beneficial in reducing heart failure [
88] and dementia [
177,
178] risk. Additionally, the supplementation of vitamins may contribute to the prevention of various diseases, including vitamin E [
132] and folate [
133] for glycemic control and insulin resistance in diabetes mellitus patients; vitamin B complex [
148] and vitamin E [
150] for stroke risk; vitamin B complex, vitamin C, vitamin E and folate [
172] for cognitive impairment; vitamin C [
214] and vitamin K2 [
200] for osteoporosis; and vitamin A [
212] and vitamin C [
213] for fractures. Obesity is a risk factor for all-cause mortality [
242], diabetes mellitus [
124,
141], cardiovascular disease [
243], ischemic stroke [
144], cognitive impairment [
166,
167], fractures [
224,
225], and many other diseases [
72]. Preventing obesity is fundamental to a healthy life. However, low BMI and decreasing lean body mass are also risks of mortality in elderly patients [
145,
244]. Thus, proper body weight management for elderly people and providing nutritional education for individuals and enlightening society as a whole is important.
The prevalence of malnutrition alone without any diseases is high in the elderly [
245,
246], and the presence of sarcopenia, frailty, and comorbidities may further increase their malnutrition risk. Therefore, screening and assessment for malnutrition is crucial. In the context of malnutrition and sarcopenia, nutritional assessment or diagnosis, represented by the Mini Nutritional Assessment [
247,
248] and GLIM [
249], recommends the measurement of the skeletal muscle mass or the calf circumference [
248,
250,
251].
Dietary fiber is an important material for short-chain fatty acids (SCFAs) production in the gut. SCFAs play an important role in gut barrier and microbiota maintenance, and they are associated with decreased inflammatory reactions [
252]. Prebiotics and probiotics enhance the effect of dietary fiber. Dysbiosis, which is defined as the impairment of microbiota composition and gut barrier integrity, is associated with many chronic diseases, including diabetes mellitus [
253] and CKD [
254]. Researchers expected to find evidence of the potential benefits that dietary fiber, prebiotics, and probiotics have for various health conditions, particularly by improving dysbiosis in CKD patients. However, although the effect has been shown in animal experimental models [
255], evidence of this topic is still insufficient [
114,
115].