Systemic lupus erythematosus (SLE), the prototype of systemic autoimmune diseases is characterized by extreme heterogeneity with a variable clinical course. Renal involvement may be observed and affects the outcome. Hydroxychloroquine should be administered to every lupus patient irrespective of organ involvement. Conventional immunosuppressive therapy includes corticosteroids, methotrexate, cyclophosphamide, mycophenolate mofetil, azathioprine, cyclosporine and tacrolimus. However, despite conventional immunosuppressive treatment, flares occur and broad immunosuppression is accompanied by multiple side effects. Flare occurrence, target organ involvement, side effects of broad immunosuppression and increased knowledge of the pathogenetic mechanisms involved in SLE pathogenesis as well as the availability of biologic agents has led to the application of biologic agents in SLE management. Biologic agents targeting various pathogenetic paths have been applied. B cell targeting agents have been used successfully. Belimumab, a B cell targeting agent, has been approved for the treatment of SLE. Rituximab, an anti-CD20 targeting agent is also used in SLE. Anifrolumab, an interferon I receptor-targeting agent has beneficial effects on SLE. In conclusion, biologic treatment is applied in SLE and should be further evaluated with the aim of a good treatment response and a significant improvement in quality of life.
1. Introduction
Systemic lupus erythematosus (SLE), the prototype of autoimmune diseases, is a highly heterogenous disease that affects all organ systems and has an unpredictable course [
1]. Its course ranges from mild to severe or fatal disease [
2]. Women within the reproductive period are mainly affected [
3]. Females originating from Africa or Asia are frequently affected and may exhibit severe disease manifestations [
3]. SLE treatment is the focus of scientific research, as biologic agents and small molecules enter management of the disease [
4].
SLE follows a variable and unpredictable course [
5]. It can be chronic or follow a relapsing and remitting course. Individuals with the disease may present with serious musculoskeletal, cardiovascular and ocular manifestations [
6]. Many of these symptoms are disease manifestations or may be caused by the application of corticosteroids for disease management [
7]. In 2014, the principle “treat to target” was introduced into the treatment strategy of SLE [
8]. Flares, target organ involvement, refractory disease, adverse effects of conventional immunosuppressive agents and a better understanding of molecular pathogenesis of SLE as well as the availability of biologic agents led to the application of biologic agents and small molecules in SLE treatment [
9,
10]. New biologic agents are in development for the management of SLE with various molecular therapeutic targets. Hydroxychloroquine is the standard mainstay treatment for SLE, and it is recommended by EULAR for patients with symptoms but without major organ lesions [
11]. Corticosteroids are administered for the treatment of SLE, but they induce broad immunosuppression, and their use is accompanied by side effects. Hence, it has been proposed that glucocorticoid use should be limited to the shortest possible time and the lowest dose possible.
3. Systemic Lupus Erythematosus Treatment
3.1. Hydroxychloroquine
Hydroxychloroquine, an antimalarial, when taken by soldiers during the Second World War for the prevention of malaria, was shown to improve musculoskeletal complaints. Thus, it was utilized in the treatment of rheumatic conditions. Hydroxychloroquine is now considered the standard-of-care treatment of SLE, as it was shown to significantly reduce mortality in all ethnic groups [
13,
14,
15], unless there are contraindications to it [
16,
17]. It is utilized in the treatment of discoid lupus and SLE [
18]. Hydroxychloroquine modulates the immune response by modulating macrophage and other antigen presenting cell function [
19,
20] and by blocking Toll-like receptors on dendritic cells [
21].
3.2. Glucocorticoids
Glucocorticoids are used in SLE at every dose level, including large, medium and small doses. Large bolus doses may be used as needed in cases of disease flare or target organ involvement and small doses as maintenance treatment [
28] to reduce disease activity and disease burden accumulation. They act via a genomic pathway, involving transrepressive and transactivating modes of action on the cell nucleus, and via a non-genomic pathway [
29]. However, they induce broad immunosuppression, and their use is accompanied by side effects.
3.3. Azathioprine
Azathioprine is administered in SLE as a conventional immunosuppressive agent that aids in steroid sparing. It may be administered as maintenance treatment in renal disease in lupus [
32] and in lupus flares. Its administration is safe during pregnancy but unsafe during lactation [
33].
3.4. Methotrexate
If low dose glucocorticoids do not control the disease, methotrexate may be applied as an immunosuppressive agent, which contributes to steroid sparing [
34,
35]. Methotrexate has an antifolate mechanism of action [
36]. It is indicated in lupus patients who display an inadequate response to hydroxychloroquine and in patients with cutaneous and articular involvement [
37] without renal disease. Methotrexate enters cells through a folate transporter [
35]. Once within the cell, methotrexate as monoglutamate forms polyglutamates, a more potent drug form which inhibits various enzymes, leading to increased adenosine levels [
38], the decreased production of ammonium and H
2O
2 and decreased synthesis of purines, methionine and DNA. Adenosine is a molecule with anti-inflammatory effects [
39].
3.5. Mycophenolate Mofetil
Mycophenolate mofetil (MMF) inhibits inosine 5-monophosphate dehydrogenase, thereby inhibiting the synthesis of guanine. Thus, B cells, T cells and fibroblasts are decreased. MMF also reduces transforming growth factor β and fibronectin synthesis, thereby exhibiting antifibrotic effects [
43]. MMF inhibits the expression of cell adhesion molecules, thereby interfering with the recruitment of lymphocytes and monocytes in the sites of inflammation. It may also induce T cell apoptosis [
44]. The first trial in lupus with MMF was performed in 2000. Thereafter, MMF became a standard drug for the treatment of lupus nephritis [
45].
3.6. Cyclophosphamide
Cyclophosphamide is an alkylating drug which acts on DNA and leads to the death of activated lymphocytes while simultaneously having a protective effect on glomeruli [
55,
56]. Cyclophosphamide displays side effects such as leukopenia, an increased infection risk, bladder toxicity and an increased cancer risk [
57]. Cyclophosphamide may be applied as induction therapy for flares or target organ involvement [
53,
58].
3.7. Calcineurin Inhibitors
Calcineurin inhibitors tacrolimus and cyclosporine have been applied as immunosuppressives in organ transplantation. They modulate the immune response mainly by inhibiting T cell activation. Additionally, they reduce albuminuria and preserve renal function [
59]. In SLE without renal involvement, cyclosporine contributes to lowering steroid dosage, reduced disease activity and flare prevention [
60] by modulating T cell function [
61,
62].
3.8. Intravenous Immunoglobulin
Therapeutic intravenous immunoglobulin (IVIg) is a product which contains human multi-specific immunoglobulin G. IVIg has been used successfully in lupus patients leading to a reduction in disease activity [
70]. IVIg was shown to be effective for various manifestations in SLE. It was shown to be effective for renal disease in SLE, as well as target organ manifestations, such as thrombocytopenia, refractory neuropsychiatric lupus [
71] and lupus myocarditis [
72]. IVIg may act via various mechanisms, including the inhibition of autoreactive B lymphocytes [
73].
4. Biologic Treatment in Systemic Lupus Erythematosus
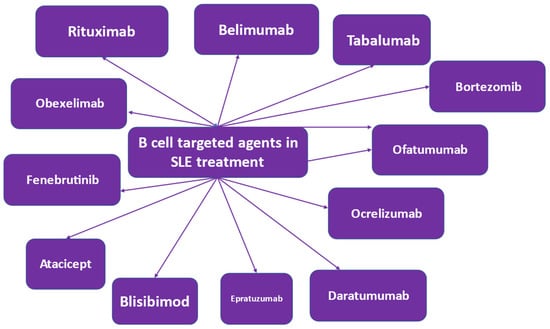
4.1. B Cell Targeted Treatment
SLE pathophysiology is characterized by B cell involvement [
89,
90]. Therefore, various therapeutic strategies targeting the B cell have been applied [
91,
92]. B lymphocytes are involved in antibody-dependent and antibody-independent mechanisms in SLE pathogenesis. Autoantibodies are produced by B cells, which are self-reacting, thereby triggering an inflammatory response. In terms of health benefits, B cells produce protective antibodies [
93]. In SLE, autoantibodies are produced, which are involved in triggering an inflammatory response via multiple mechanisms, including the induction of cytokine and interferon production by innate immune cells [
94]. This immune mechanism is disturbed in SLE patients and is further disrupted by the abnormal functioning of other immune cells [
95]. Novel treatment methods that target the B cell have been developed or are in development [
91,
92] (
Figure 3).
Figure 3. B cell-targeted biologic agents in the treatment of systemic lupus erythematosus (SLE).
4.1.1. Rituximab
Rituximab is a B cell-depleting anti-CD20 monoclonal antibody, applied as a B cell-targeted treatment. Rituximab depletes CD20-positive B cells; however, it spares stem cells and plasma cells, as they do not express the CD20 molecule [
103,
104]. Rituximab depletes B cells via antibody-dependent and complement-mediated cytotoxicity [
105]. It induces B cell apoptosis and reduces proliferation. Rituximab may be used to treat refractory SLE with renal and neuropsychiatric manifestations [
106,
107,
108].
4.1.2. Belimumab
Belimumab is a fully humanized monoclonal antibody against BlyS. It has been administered in clinical trials intravenously and subcutaneously. Belimumab was approved by the FDA for the treatment of seropositive, moderate SLE. Two international clinical trials [
79,
120] in autoantibody-positive adult patients with active SLE evaluated belimumab. SLE patients were randomized to receive either belimumab or placebo in addition to standard-of-care treatment.
4.1.3. Tabalumab
Tabalumab, is a monoclonal antibody against soluble and membrane-bound BlyS [
135]. Tabalumab was tested in two phase III trials, namely ILLUMINATE-1 and ILLUMINATE-2, in adult patients with moderate to severe SLE without kidney involvement [
97,
135]. ILLUMINATE-1 did not meet the primary efficacy endpoint in the tabalumab arm—as opposed to ILLUMINATE-2, in which the SRI_5 response was met—in the cohort receiving tabalumab 120 mg twice monthly. Depression was observed in some patients on tabalumab, and some patients attempted suicide.
4.1.4. Atacicept
Atacicept is an antagonist of BlyS- and APRIL-mediated B cell activation. It is a fused protein of the TACI (transmembrane activator calcium moderator and cyclophilin ligand interactor) and IgG, which binds to both Blys and APRIL. As both BlyS and APRIL have been found to be increased in SLE patients, it was suggested that the dual blockade by atacicept might be more effective than BlyS blocking [
98]. Atacicept was tested in a phase II b study in SLE patients [
136].
4.1.5. Blisibimod
Blisibimod is a moiety that inhibits BlyS and displays the characteristics of a peptide and an antibody. It was tested in a phase II trial in SLE and did not reach the primary efficacy endpoint of SRI-5 response [
137]. A beneficial treatment effect was observed in SLE patients with high disease activity, where it appeared to be effective in lowering the steroid dosage [
138]. The drug appeared to be well tolerated with no serious reported adverse events and no deaths in the treatment arms.
4.1.6. Epratuzumab
Epratuzumab is a monoclonal antibody against CD22. It binds to CD22, thereby inhibiting B cell activation [
139,
140]. CD22 is a molecule, which is expressed on mature B cells, not on plasma cells or memory B cells, and acts as an inhibitory co-receptor of the B cell receptor and modulates B cell activation and migration.
4.1.7. Daratumumab
Daratumumab is a monoclonal antibody against CD38, a molecule expressed on plasmablasts [
142]. CD38 is expressed on plasmablasts, CD19+ mature B cells and plasmacytoid dendritic cells in lupus patients. Daratumumab was administered to two female patients with lupus nephritis and autoimmune hemolytic anemia not responding to immunosuppression [
143]. Patients were administered belimumab after the unsuccessful administration of daratumumab.
4.1.8. Ocrelizumab
Ocrelizumab is a fully humanized monoclonal antibody against CD20 with higher antibody-dependent complement and lower complement-dependent cytotoxicity effects as compared to rituximab in SLE patients [
144]. Ocrelizumab was successfully used in relapsing, remitting and primary progressive multiple sclerosis [
145]. Ocrelizumab was tested in patients with lupus nephritis with beneficial effects, but it displayed a high rate of serious infections [
146].
4.1.9. Obinutuzumab
Obinutuzumab, a novel humanized type II glycoengineered anti-CD20 antibody, is a B-cell targeting treatment, which may be administered in SLE patients [
142,
147]. Studies performed in vitro indicated that obinutuzumab may induce higher B cell cytotoxicity as compared to rituximab in SLE [
147,
148].
4.1.10. Ofatumumab
Ofatumumab is a fully humanized anti-CD20 monoclonal antibody. It has been applied as a B cell-depleting agent, which may be used in patients with SLE intolerant to rituximab, i.e., in patients who develop infusion reactions to rituximab [
150,
151]. It induces antibody- and complement-dependent cytotoxicity in B lymphocytes expressing CD20. Ofatumumab exhibits potency in B cells lysis, which stems from its ability to bind with high affinity to the short extracellular part of the CD20 molecule and its slow release from the target molecule.
4.1.11. Obexelimab
Obexelimab is a humanized anti-CD19 monoclonal antibody targeting FcgRIIb, which is a reversible B-cell inhibitor [
142]. CD-19 is a cell surface molecule found on B cells, plasmablasts and plasma cells [
153]. It was hypothesized that targeting CD19 could lead to significant B cell and plasma cell depletion in lupus patients. Obexelimab was tested in a phase II randomized trial in moderately active lupus patients.
4.1.12. Bruton’s Tyrosine Kinase-Targeted Treatment
Currently, B-cell signaling is a target for B-cell treatment in SLE. Tyrosine kinases, Bruton’s tyrosine kinase in particular, acts as an intracellular molecule essential for the development, survival and activation of B cells. Bruton’s tyrosine kinase is involved in antigen presentation, B-cell differentiation and the production of autoantibodies in SLE [
154]. In experimental animal models, Bruton’s tyrosine kinase inhibition was shown to have beneficial effects in SLE [
155].
4.1.13. Proteasome Inhibitors
CD-20 negative cells may be source of treatment failures with CD-20-targeting agents. CD-20 negative cells may be targeted by inhibiting the proteasome. Proteasome inhibition leads to the accumulation of defective immunoglobulin chains and induces stress in the endoplasmic reticulum, leading to plasma cell apoptosis [
157]. Bortezomib is a proteasome inhibitor, which has been tested in animal models of lupus [
158]. Bortezomib was also tested in SLE patients.
4.1.14. Rigerimod
Rigerimod is a peptide which blocks antigen presentation to T cells by reducing the stability of MHC molecules, thereby inhibiting B cell function. Rigerimod has been utilized in lupus patients with encouraging results [
161].
4.2. Interferon Inhibitors
4.2.1. Sifalimumab
Interferons (IFNs) are immunostimulatory cytokines divided in three categories: types I, II and III [
162]. IFNα is a type I IFN that is abundant and has been studied in depth. The role of interferons in the pathogenesis of SLE has been extensively studied and has been proven [
163].
4.2.2. Anifrolumab
Type I IFN may be implicated in the pathogenesis of SLE. A gain-of-function genetic mutation in the type I IFN pathway may be associated with a higher risk of SLE [
165]. In the period before the clinical presentation of SLE, high type I IFN and SLE autoantibodies have been observed. Patients with established SLE and evidence of high type I IFN may have more active disease and lupus nephritis or other severe manifestations.
4.3. Interleukin Inhibitors
4.3.1. Tocilizumab
Tocilizumab is a humanized monoclonal antibody against interleukin-6 receptor [
168] and has been mainly used in the treatment of rheumatoid arthritis [
169] and is also utilized in the treatment of giant cell arteritis [
170]. Tocilizumab has been also used in patients with severe SARS-CoV-2 virus infection [
171]. Tocilizumab was used to treat refractory hemolytic anemia in an SLE patient [
172].
4.3.2. Secukinumab
Secukinumab is a monoclonal antibody which binds to interleukin 17A. It is used in ankylosing spondylitis, psoriasis and psoriatic arthritis [
176,
177,
178]. T-helper 17 cells are thought to be involved in the pathogenesis of SLE [
179]. Secukinumab was administered to a female patient with psoriasis and refractory lupus nephritis with beneficial effects [
180].
4.4. Low Dose Interleukin-2
The loss of immune tolerance characterizes SLE. This loss of tolerance may be due to the impaired function of T regulatory cells (Tregs) [
182,
183] as well as an imbalance between T follicular helper cells and T follicular regulatory cells. Low dose interleukin-2 in patients with SLE was shown to restore the balance between T follicular regulatory cells and T follicular helper cells in favor of T follicular regulatory cells and display clinical efficacy in SLE [
184,
185].
4.5. JAK Inhibitors
Baricitinib
Baricitinib, a selective oral inhibitor of Janus kinase, has been approved for the treatment of rheumatoid arthritis [
186]. Baricitinib has been evaluated in active SLE patients not responding to standard-of-care treatment. The resolution of arthritis and rash was observed [
187].
5. Therapeutic Strategies for the Management of SLE
In 2014, the treat-to-target principle was introduced in the strategy for the therapeutic management of SLE [
8]. In 2019, the EULAR recommendations based on evidence and expert opinion for the management of SLE were updated [
188]. It was concluded that hydroxychloroquine should be administered to all lupus patients. During lupus flares, bolus doses of glucocorticoids should be administered. During maintenance treatment, glucocorticoids should be minimized and, if possible, withdrawn entirely. The initiation of immunomodulatory agents can aid in the reduction or withdrawal of glucocorticoids. However, despite conventional immunosuppressive treatment, flares of the disease occur and some patients may not respond to it. Treatment of flares in unresponsive patients targets organ involvement, and the observation of side effects, the deeper knowledge of pathogenetic paths in SLE and the availability of biologic agents has enabled the introduction of biologic agents and small molecules in the treatment of SLE. B cell-targeting agents have been introduced with success. Rituximab may be used in renal and non-renal SLE. Belimumab has been approved for the treatment of SLE. The sequential use of rituximab followed by belimumab has also been tested in refractory cases. In 2023, the Study Group of Autoimmune Diseases of the Portuguese Society of Internal Medicine issued recommendations for the off-label use of biologic agents and small molecules in SLE [
9]. They suggested that in SLE patients with very active disease, i.e., SLEDAI > 20 or BILAG 3A, severe hemolytic anemia, severe thrombocytopenia, severe kidney disease (stage IV) or severe CNS disease, the use of rituximab is recommended as first-line therapy. In patients with very active disease, such as severe kidney disease or severe CNS disease, the sequential use of rituximab followed by belimumab may be applied. In patients with persistently active disease with flares for at least one year or very active disease, rituximab is recommended in rituximab-naïve cases as second-line therapy, and baricitinib or tocilizumab may be used if arthritis predominates as second-line treatment. In lupus patients with severe kidney disease, rituximab is recommended in rituximab-naïve patients as second-line therapy, and the sequential use of rituximab and belimumab may be used in refractory cases as second-line treatment. In patients with very active disease, the sequential use of rituximab followed by belimumab may be applied in rituximab-naïve patients as second-line treatment. In these patients with very active disease, bortezomib may be considered in multi-refractory cases as second-line treatment. In patients with hemolytic anemia or thrombocytopenia, rituximab is recommended and bortezomib may be considered in multi-refractoriness. For moderate or severe CNS disease, rituximab is recommended in rituximab-naïve cases as second-line treatment and the sequential use of rituximab followed by belimumab may be considered in refractory cases as second-line treatment.
This entry is adapted from the peer-reviewed paper 10.3390/life13071496