The use of advanced preclinical models has become increasingly important in drug development. This is particularly relevant in bladder cancer, where the global burden of disease is quite high based on prevalence and a relatively high rate of lethality. Predictive tools to select patients who will be responsive to invasive or morbid therapies (chemotherapy, radiotherapy, immunotherapy, and/or surgery) are largely absent. Patient-derived and clinically relevant models including patient-derived xenografts (PDX), organoids, and conditional reprogramming (CR) of cell cultures efficiently generate numerous models and are being used in both basic and translational cancer biology. These CR cells (CRCs) can be reprogrammed to maintain a highly proliferative state and reproduce the genomic and histological characteristics of the parental tissue. Therefore, CR technology may be a clinically relevant model to test and predict drug sensitivity, conduct gene profile analysis and xenograft research, and undertake personalized medicine.
1. Circulating Tumor Cells (CTCs): Importance and Technical Challenges
Liquid biopsies are noninvasive methods that may be harnessed for cancer precision medicine. Circulating factors, including circulating tumor cells (CTCs), cell-free DNA (cfDNA), RNAs (miRNAs, long noncoding RNAs [lncRNAs], mRNAs), cell-free proteins, peptides, and exosomes are derived from cells in human body liquids. CTCs from BC can be detected in the urine and serum of patients with metastatic BC, with higher levels of CTCs correlating with cancer aggressiveness [
69,
70]. CTCs derived from BC can be measured by using CTC-specific proteins, such as c-MET and PD-L1 [
71,
72,
73]. Increased CTC levels were also able to predict clinical outcomes, such as recurrence and survival [
74]. CellSearch
TM, an FDA-approved CTC assay kit, is currently being used in clinical settings for prognostic purposes in breast cancer but has low sensitivity and specificity [
75]. Being able to culture cancer cells from blood and other liquid biopsies would be extremely valuable, but there are many technical issues that limit the study of CTC biology and their applications. It is technically difficult to capture and characterize viable CTCs [
67,
76,
77].
2. Noncirculating Cell Biomarkers
In addition to CTCs, DNA, RNA, and exosome candidate biomarkers in serum and/or urine have been identified in BC. Mutation of the human telomerase reverse transcriptase gene (hTERT) promoter occurs in 70% of human BC and is also associated with recurrence and poor prognosis of BC [
78,
79,
80,
81]. In the urine specimens of BC patients, the telomerase reverse transcriptase (TERT) promoter mutations correlated with recurrence [
82], while KRAS2 mutations were found in the plasma even before BC diagnosis [
83]. Urinary UBE2C and hTERT mRNA were found to be potential markers for early diagnosis and prognosis of BC [
84]. Urinary levels of miR-126 and miR-146a-5p were also found to be elevated in BC and are associated with tumor grade and invasiveness [
85]. Exosomes transfer biologically active molecules and can be secreted into the urine, blood, and other body fluids [
86]. Hence, exosomes are essential mediators of cell–cell communication [
87]. Interestingly, there is a strong association between heightened exosome levels and BC [
88]. In urinary exosomes, significantly increased levels of active molecules (e.g., TACSTD2, lncRNAs–HOTAIR, HOX- AS-2, ANRIL, and linc-ROR) were found in high-grade MIBC patients [
89]. However, none of the above markers are found in a majority of BC and urine samples of patients and thus have not been suggested for clinic use. Further, they cannot be used for functional analyses to predict clinical outcome.
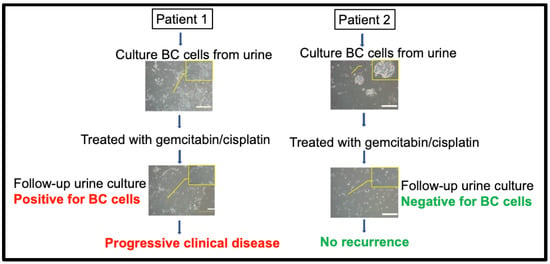
3. Urine CRCs as a Living and Functional Biomarker for Clinical Relevance and Response
Our previous work evaluated drug responses via CR culture of bladder cancer cells, which was taken from urine samples. The success rate of urine CRC cultures was high, 83.3% (50 of 60 cases); specifically, low-grade bladder cancer was 75.0% (9 of 12 cases), and high-grade bladder cancer was 85.4% (41 of 48 cases). Interestingly, researchers obtained a 100% success rate of BC cell cultures after researchers optimized collection conditions. Additionally, researchers did not observe bias for the success rates of CRC urine cultures with respect to pathology group, disease status, age, or gender from all bladder cancer cases. Researchers also reported that CR cells had 79.7–82.6% of genetic variation similar to the original tumors. Thirteen patients underwent drug-sensitivity tests, which revealed varied responses to conventional drugs such as gemcitabine, cisplatin, pirarubicin, and epirubicin [
62]. In order to study whether urine BC cells can predict clinical response, researchers collected urine samples before and after treatment. Thus, researchers were able to establish urine CR BC cells from Patients 1 and 2 before treatment (surgery and/or intravenous chemotherapy, gemcitabine + cisplatin;
Figure 1) and from urine samples after treatment; however, researchers only established UCCC from Patient 1, not Patient 2, after two cycles of chemotherapy. This outcome was consistent with clinical follow-up showing that Patient 1′s tumor soon relapsed after treatment. However, the tumor in Patient 2 showed no recurrence after the first and second cycles of chemotherapy, correlating with our urine BC cell culture results.
Figure 1. Clinical relevance of urine CR BC cells from Patients 1 and 2. Patient 1 accepted tumor resection following chemotherapy but soon relapsed (red). Patient 2’s tumor was sensitive to chemotherapy. Phase contract images of urine CR cell conditions before and after chemotherapy treatment in Patients 1 and 2. Researchers failed to establish urine CR BC cells after the first and second cycles of chemotherapy in Patient 2 since this patient was disease-free (green). Red color indicated positive CR BC culture and active disease (non-responder, or BC recurrence). Green color indicated negative CR BC culture and disease free (responder, or no recurrence). The figure was drawn using BioRender.
Our data also showed that response of CR BC cells generated from patients’ urine samples prior to treatment correlated with response of the BC patients. The CR BC cells of one patient showed relatively low sensitivity to pirarubicin, which was consistent with clinical follow-up. This patient’s tumor soon relapsed 3 months later after intravesical treatment with pirarubicin (40 mg) followed by undergoing transurethral resection. Another patient showed relative sensitivity to gemcitabine and cisplatin. In the absence of surgery, his CT obtained 6 months later showed stable disease (SD) after treatment with gemcitabine (1000 mg/m2/intravenous) and cisplatin (70 mg/m2/intravenous). These clinical results correlated well with the drug-sensitivity profiles of the corresponding CR cells in response to gemcitabine and cisplatin. Thus, urine BC cells can be used to test drug sensitivity, and their response seemed to correlate with the patients’ response.
4. Urine CRCs with IFN-Induced PD-L1 Levels as a Novel Biomarker for BC Immunotherapies
Checkpoint blockade immunotherapy has been widely used in bladder cancer treatment, but its effectiveness cannot be determined by traditional preclinical models. For example, increased evidence from both preclinical and clinical studies mostly indicates that the immunochemistry (IHC) of programmed-death ligand 1 (PD-L1) levels in tumor tissues currently used clinically is not a satisfactory predictor of anti-PD-1/PD-L1 treatment outcomes [
90]. Glycosylation of PD-L1 may render its polypeptide antigens inaccessible to PD-L1 antibodies, leading to inaccurate IHC readouts in some patient samples [
86,
91]. Recently researchers found that different BC cells have different PD-L1 expression and sensitivity to IFN-γ, and these diversities can be found not only between tumor cells from different patients but also among subclones in tumor cells from the same patient. Researchers investigated PD-L1 as a means to predict the immune checkpoint inhibitors response in bladder cancer by CR technology. Researchers collected 43 tumor/urine (tumor = 17, urine = 26) samples of primary bladder cancer patients and generated bladder cancer cells. The expression levels of PD-L1 on bladder cancer cells were measured by flow cytometry before and after interferon gamma treatment. Researchers found that IFN-γ-stimulated PD-L1 (sPD-L1) expression on BC cells may predict the prognosis of BC patients. The better prognostic value was in urine BC-PD-L1. Transcriptome analysis showed that BC cells with high sPD-L1 tended to enrich genes associated with the collagen-containing extracellular matrix, cell–cell adhesion, and positive regulation of the immune system. Urine BC-PD-L1 also exhibited predictive value for ICI response in BC patients. The results showed great potential of urine CR bladder cancer cell PD-L1 for prognostic and predictive value in clinical practice [
92]. This would be the first functional predictive biomarker for BC immunotherapy.
Currently, cystoscopy is the gold standard method for diagnosis and surveillance in bladder cancer. It is an invasive, painful, and expensive procedure. Most invasive procedure have complications and possible negative consequences for patients [
93]. Therefore, discovering a noninvasive method will be beneficial for diagnosis, drug-sensitivity assessment, and follow-up. Liquid biopsies recently came into use in the clinical setting, and studies have confirmed their ability to reveal various genetic alterations of metastatic and primary tumors and provide precise clinical information [
94]. The most easily reachable liquid biopsy type for bladder cancer is urine. Urine is easy to access, and liquid biopsies are noninvasive and appropriate for patient follow-up. Liquid biopsies have been broadly explored for diagnosis and surveillance of bladder cancer by detecting biomarkers such as microRNA, circular RNA, and cell-free DNA [
95]. Further studies need to be conducted to determine other possible applications of this noninvasive urine-derived model in bladder cancer.
This entry is adapted from the peer-reviewed paper 10.3390/cells12131714