Biobanks provide a platform for innovative biomedical research. Recent scientific advances in cryopreservation have enabled the prospect of establishing “living biobanks” that store viable, functional tissue or replicable cell types for years to decades.
1. Introduction
Traditional cancer models including cell lines and animal models have limited applications in both basic and clinical cancer research. Genomics-based precision oncology only help 2–20% patients with solid cancer. Functional diagnostics and patient-derived cancer models are needed for precision cancer biology. In this review, we will summarize applications of conditional cell reprogramming (CR) in cancer research and next generation living biobanks (NGLB). Together with organoids, CR has been cited in two NCI (National Cancer Institute, USA) programs (PDMR: patient-derived cancer model repository; HCMI: human cancer model initiatives. HCMI will be distributed through ATCC). Briefly, the CR method is a simple co-culture technology with a Rho kinase inhibitor, Y-27632, in combination with fibroblast feeder cells, which allows us to rapidly expand both normal and malignant epithelial cells from diverse anatomic sites and mammalian species and does not require transfection with exogenous viral or cellular genes. Establishment of CR cells from both normal and tumor tissue is highly efficient. The robust nature of the technique is exemplified by the ability to produce 2 × 106 cells in five days from a core biopsy of tumor tissue. Normal CR cell cultures retain a normal karyotype and differentiation potential and CR cells derived from tumors retain their tumorigenic phenotype. CR also allows us to enrich cancer cells from urine (for bladder cancer), blood (for prostate cancer), and pleural effusion (for non-small cell lung carcinoma). The ability to produce inexhaustible cell populations using CR technology from small biopsies and cryopreserved specimens has the potential to transform biobanking repositories (NGLB: next-generation living biobank) and current pathology practice by enabling genetic, biochemical, metabolomic, proteomic, and biological assays, including chemosensitivity testing as a functional diagnostics tool for precision cancer medicine.
2. Patient-Derived Cancer Models and CRC are Needed for Precision Oncology
2.1. iPS (Induce Pluripotent Stem) Cells
Both embryonic and adult stem cells can be propagated in vitro and these cells retain a normal karyotype and can differentiate into several germ layers, providing great potential for applications in regenerative medicine [
25,
26]. Several recent review articles summarized applications if iPS in cancer modeling [
27,
28,
29,
30,
31].
2.2. Organoid Cultures
The laboratories of Clevers, Kuo and others successfully established organoid cultures initially from mouse tissues [
32,
33,
34,
35,
36,
37]. These studies have now been extended to human specimens, both normal and tumor. Organoid cultures provide a platform to investigate basic biology for early stage cancers, to identify drug targets, and to study drug resistance [
36,
38,
39,
40,
41,
42,
43,
44,
45]. Unlike monolayer cell lines that are grown on plastic, organoid cultures are established using three-dimensional growth of epithelial cells in Matrigel™. These cultures are fairly stable genetically, can be grown for a long period of time and are not clonal in selection, but rather capture partial heterogeneity of the original tumor. Paired normal and cancer organoids can be established from the same patient samples, thereby providing an opportunity for its application to personalized medicine and regenerative medicine. Precise tumor tissue sampling is very crucial for organoid cultures as this culture system propagates both normal and cancer cells. Additionally, these cultures are more suitable for low-throughput rather than high throughput drug screening [
44,
45]. Overall it takes 4-6 weeks to provide enough cells for drug screening [
46].
2.3. Patient-Derived Xenografts (PDX)
In recent years patient-derived xenografts have emerged as a viable system for modeling human tumors in vitro [
47,
48]. Unlike cell lines, such as lack of stromal components, clonal selection, and genetic drift due to long-term culturing conditions, PDX models cross-talk between stromal components and epithelial tumor cells, appear to have high genetic stability, especially during early passages, and can preserve the molecular and cellular heterogeneity of the primary tumor. In addition, PDX models appear to predict metastatic potential and response too [
49]. Currently, PDXs are still widely recognized as a more physiologically relevant preclinical model to standard cell line xenografts. PDX models faithfully recapitulate the original patient genetic profile, gene expression patterns and tissue histology. Despite their benefits, PDX models are limited by their inherent variability, lower throughput and lack of growth in vitro. The ability to generate cell lines from PDX models would enable high throughput chemosensitivity screens, ex vivo genetic manipulation and the development of novel orthotopic models. Development of stable PDX cell lines remains a challenge due to murine stromal outgrowth, lineage commitment and limited differentiation potential. Overall, it takes 2–5 month for PDX expansion at a relatively high cost of mice and their care.
2.4. Conditionally Reprogrammed Cells (CRCs)
It remains a challenge to establish a single model system that is rapid, simple to perform, and has a high rate of success. The CRC method we developed at Georgetown meets these needs. The culture method can rapidly convert normal and tumor cells to a state of “reprogrammed stem-like” in which the cells are highly proliferative and maintain their original karyotypes; moreover, the removal of these conditions restores the capacity for cell differentiation [
12,
50,
51]. Thus, we named this method “conditional reprogramming”. As we have described below in the detailed protocols. Briefly, the tissue samples are first evaluated histologically by a pathologist to determine the composition of the sample (i.e., what percentage of the cells are tumor cells). The samples are then dispersed into single cells by enzymatic digestion and plated in a medium containing irradiated Swiss-3T3-J2 mouse fibroblasts (feeder cells) and 10 µM Y-27632. Epithelial colonies are readily observed at two days and usually proliferate rapidly to reach confluence in approximately five days. The conditional reprogramming method is applicable to many epithelial tissues including skin, prostate, lung, breast, kidney, salivary gland and liver cell types and it has recently been extended to neuroendocrine and endocrine tissues. Interestingly, the method seems generally applicable to many mammalian species such as mouse, rat, dog, ferret, horse, and cow [
52,
53,
54,
55,
56,
57]. An important feature is that these cultures can be used for establishing xenografts [
12,
50] and patient-derived xenograft cell lines [
58] and can also be used to generate cell cultures from PDX and organoid cultures. Finally, conditionally reprogrammed cells retain cell lineage commitment and maintain the heterogeneity of cells present in a biopsy [
12,
50,
59,
60,
61,
62].
3. Next-Generation Living Biobanks (NGLB)
Living Biobanks will have a significant impact across basic biological research, medicine and the biopharma industry; however, the effects of such applications are underexplored. Recent approaches, for example, patient-derived xenograft models, organoids, conditionally reprogrammed cells, induced pluripotent cells, and other cancer precision medicine applications, represent an unexhausted resource of living biobanks. However, these concepts are applied in very many different ways by the academic and private sectors, representing an actively growing field that has yet to reach clinical consensus or maturity. Here we summarize application of CR technology in living biobanks.
28–29 March 2011, we first presented “bring biobank to life” at BRN 2011 Symposium “Advancing Cancer Research Through Biospecimen Science” of NCI when we started CR technology [
12,
84]. Editor in Chief of American Journal of Pathology proposed applications of CR technology in living biobanks [
84]. Eventually, more and more articles came out for tumor living biobanks as the applications of CRC and organoid cultures [
37,
43,
46,
51,
59,
85,
86,
87,
88,
89,
90,
91,
92,
93,
94,
95,
96,
97,
98,
99,
100,
101,
102]. However, that will be impossible task in terms of efforts, work load and cost if one would like to establish living biobanks from every patient in the hospital for the immediate use of personalized medicine. In order to balance of distribution of disease types for research and industry, it’s extremely important to cryopreserved tissue specimens and will generate cell cultures using CR and/or organoids technologies. Thus, we brought forth a new concept: next generation living biobank (NGLB) (
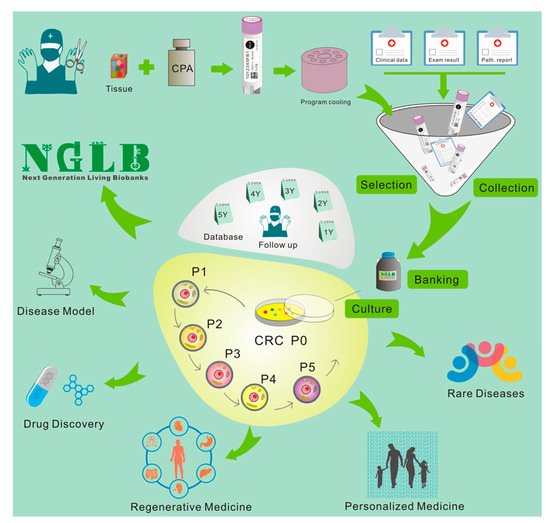
Figure 6). Except for immediate use of personalized diagnostics and treatment, we suggest to collect and cryopreserve specimens including surgical specimens, core biopsies, needle biopsies, brushed cells, or cells from liquid biopsies (blood, urine, etc.). These specimens should be collected and stored together with their corresponding -omics (genomic, transcriptomic, proteomic, metabolomic, etc.) and clinical information. Then, CR technology will be used to generate an unexhausted cell cultures for living cell banks for future demands in drug discovery, disease modeling, regenerative medicine. These cryopreserved specimens, their corresponding CR cells and CRC- derivatives together compose of NGLB (
Figure 1). Compared to regular living biobanks, this NGLB strategy would be a highly efficient platform with the minimal time, money, and other support, this may also avoid redundant cell lines from common diseases, for example, lung cancers. Most importantly, this NBLG includes cryopreserved specimens with broader coverage of disease types, which allow us to generate cell cultures from rare disease using CR or organoids cultures, since there are no available cell models or very few cell lines for many rare diseases, for example, adenoid cystic carcinoma (ACC), neuroendocrine cancer, etc. We also list properties of conventional cell lines, CRC, organoids and PDX in basic and translational cancer research (
Table 1).
Figure 1. Workflow of next generation living biobanks (NGLB). Specimens including surgical specimens, core biopsies, needle biopsies, brushed cells, or cells from liquid biopsies (blood, urine, etc.) from patients with disease and/or different stages of disease (for example, before and after treatment, primary or metastatic, etc.) will be collected, cryopreserved, and stored together with their corresponding -omics (genomic, transcriptomic, proteomic, metabolomic, etc.) and clinical information. CR technology will be used to generate an unexhausted cell cultures for living cell banks for future demands in drug discovery, disease modeling, regenerative medicine. CR cells can be used to generate other types of living biobanks such organoids or patient-derived xenografts (PDX) (for tumor).
Table 1. Comparison of a patient-derived cancer models.
| |
Conventional Cell Lines |
Organoids |
PDX |
CRC |
| Sample size |
| FNA |
− |
+/− |
− |
+++ |
| Core Biopsy |
− |
+ |
− |
+++ |
| Surgical Specimens |
+ |
+++ |
++ |
+++ |
| Timing |
dozen days |
1-5 weeks |
1-5mont |
1-10 days |
| Success rate of initiation |
+ 0–10% |
++ (5–80%) |
++ (2–30%) |
+++50–100% |
| Tumor type specific |
| Rapid Expansion |
+++ |
++ |
+ |
+++ |
| Matched Normal con |
− |
+ |
- |
+ |
| Karyotypic stability |
− |
++ |
N/A |
++ |
| 3D growth |
− |
+ |
+++ |
− |
| Representation of tumor |
+ |
++ |
++ |
++ |
| Genetic manipulation |
+++ |
++ |
− |
++ |
| Maintenance (passage) |
+++ |
++ |
+ |
+++ |
| LT drug screens |
+++ |
– |
+ |
+++ |
| HT drug screens |
+++ |
++ |
− |
+++ |
| Heterogeneity |
− |
++ |
+++ |
++ |
| Tumor–stroma interaction |
− |
− |
++ |
− |
This entry is adapted from the peer-reviewed paper 10.3390/cells8111327