Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Additive manufacturing (AM), which is also called rapid prototyping/3D printing/layered manufacturing, can be considered as a rapid conversion between digital and physical models. One of the most used materials in AM is polylactic acid (PLA), which has advantageous material properties such as biocompatibility, biodegradability, and nontoxicity. For many medical applications, it is considered as a leading biomaterial. In dentistry, in addition to its uses in dental models (education, teaching, simulation needs), it can be used for therapeutic objectives and tissue engineering.
- additive manufacturing
- fused filament fabrication
- polylactic acid
- dentistry
1. Introduction
Traditional methods of transplantation of organs have several risks such as limited sources, complications, and secondary injuries. Additive manufacturing (AM) technology potentially helps to solve these issues since it can rapidly fabricate personalized tissue structures such as scaffolds, repair certain tissue defects, and even directly manufacture tissues and organs [1]. It is true that these types of additively manufactured structures cannot perfectly match the patient’s damaged tissue, but they may possess suitable microstructures and cell arrangements for the promotion of cell growth and differentiation. Figure 1 presents the roadmap of the three main axes. The first axis is represented by the most common AM applications that can be found in the following areas: aerospace, spare parts, arts and design, prototyping, and medicine. The medical applications can be divided into orthopedics and orthodontics. Using AM technology, it is possible to build complicated models for surgery preparation. AM models of a patient’s anatomy can be very helpful to better understand the patient’s anatomy prior to surgery instead of using CT scans and MRI. In addition, these models can be used for surgical simulation and training purposes [2,3,4]. Dentistry involves the diagnosis, treatment, and condition counteraction, turmoil, and sicknesses of the teeth, gums, jaws, and mouth. It is frequently viewed as fundamental for complete oral well-being. The human mouth’s oral cavity includes the upper and lower jaws, which are respectively called maxilla and mandible. Each jaw (upper/lower) contains 16 teeth, nerves, blood vessels and muscles [5]. Dentistry was selected to be treated since it can affect the whole human body’s health. The second axis is represented by the most common AM materials: plastics, metals, ceramics, and composites [6]. Plastic materials have two types: thermosets and thermoplastics. Thermoplastic materials are utilized in two kinds of AM techniques: powder bed fusion and material extrusion. Among these kinds, amorphous thermoplastic materials are utilized for material extrusion processes due to their melt properties (high viscous melt). The typical size of the nozzle used for extrusion of these materials is 0.2–0.5 mm [7]. Polylactic acid (PLA) [8,9] and acrylonitrile butadiene styrene (ABS) [10,11] are the two most common examples. Polycarbonate (PC) [12], PC/ABS blend [13], and polyetherimide (PEI) [14] are other examples of amorphous materials that are used in material extrusion. The thirst axis is represented by the most common material-based AM processes. The classifications of these processes are based on the material states: solid, liquid, and powder. They can be respectively labeled as follows: solid-based AM methods, liquid-based AM methods, and powder-based AM methods [15]. Material extrusion, powder bed fusion directed energy deposition material jetting, binder jetting, vat photopolymerization, and sheet lamination are among the seven additive manufacturing techniques classified by ASTM/F2921 [4]. Extrusion-based techniques, being cost-effective, are widely used for solid materials. Several materials such as multi-colored plastics and living cells are manufactured following a material extrusion-based technology [16]. Additionally, this process can be completely based on the functional aspects of the products [17,18]. Among these techniques, fused filament fabrication (FFF), also called fused deposition modeling (FDM), is a desirable AM technique in order to fabricate PLA due to its geometrical flexibility and relatively low cost. An illustration and details of the FFF technique can be found in our previous work [19]. Using the FFF technique, several dental applications can be performed in a simple way. For example, with this technique, it is possible to produce polymer dentures with hollow, semi-hollow, and solid structures [20].
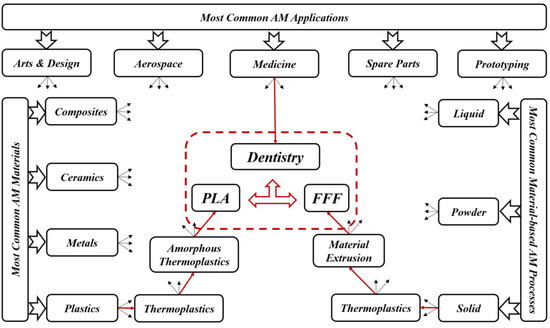
Figure 1. Roadmap of current review topics.
2. AM Techniques Used in Dentistry
Day by day, additive manufacturing technology is expanding, and, because of its frequently used layer-by-layer construction, it has a remarkable perspective for biomedical applications. This technology may directly fabricate specific functional components with the help of scanned data in CT images that give superior visualization of a particular framework. In typical presurgical preparation, it helps medical experts to practically replan surgical events. In addition, it can be considered as a communication tool between medical experts and patients [15,21].
Fields such as dentistry, where the anisotropy is needed as per the requirement, pose as best clients for AM technology. Implant section is one of the most important medical applications for AM. The implants are customized as per the needs and patient’s requirements; AM can then help in fabricating those implants as required [22]. For dental applications, models, splints, and drill guides are developed by AM technology. In addition, the development of artificial tissues and organs has been carried out by using AM techniques [23]. AM techniques are currently widely used for 3D organ models, which are useful to understand complex human anatomy. In a recent review by Rouf et al. [6], several AM techniques for various aspects of medical needs (orthopedics and orthodontics) were presented. Some AM works in dentistry are presented since AM for dentistry has been applied for almost 20 years. As shown in Figure 2, for metallic dental crowns, researchers used several AM techniques such as fused filament fabrication (FFF) [24], selective laser sintering (SLS) [25], stereolithography (SLA) [26], and laminated object manufacturing (LOM) [27]. Dental pieces, bridges and crowns were the dental applications for these AM techniques [28,29]. For non-metallic oral implants, crowns and bridges, models for dental study, and surgical equipment (specifically surgical guides for dental surgery), SLA and FFF are generally used [30]. For maxillofacial implants, the metallic powder using the selective laser melting method (SLM) [31] replaces the patient’s entire jaw. Furthermore, AM technologies have been used for creating complete or partial dentures, where direct laser metal sintering (DLMS) processes have been utilized to create metallic dentures [32,33,34]. The FFF technique has been used to create polymer dentures with solid, hollow, or semi-hollow structures [20]. Research is currently being conducted using AM techniques to develop dentures that possess anti-microbial properties [35]. FFF and SLA have been used to generate bioresorbable polymer dental implants that display odontogenic properties [36,37]. Recently, powder bed fusion technologies became leading AM techniques in dental applications [6]. However, the roughness associated with printed components can represent a real issue. So, there is a need to remedy the roughness in dental implants. On the other hand, FFF technique can be utilized in order to create complex and functional geometries, starting directly from CAD models [38]. This technique can then be employed in order to produce cellular structures with controllable pore shape, pore size, and porosity. These kinds of structures are fundamental in orthopedic scaffolds due to their high compressive strength, low elastic modulus, and adequate cell accommodation spaces. Several developments are needed to extend the application of these advantageous structures to dentistry, especially when a patient suffers from bone loss due to injuries or accidents. Furthermore, other AM applications can be found in maxillofacial surgery. For example, it is possible to develop surgical equipment to correct facial defects. This kind of equipment can reduce the surgery risks and provide aesthetic results [39]. By developing 3D inkjet-printed bones in the jaw area, a group of researchers found a solution for mandibular deformities [40]. These fabricated bones had dimensional compatibility in patients, and there was a link between artificial bones and host ones. That can allow reducing operational time and risk and simplify adjusting the size for bone fixation during treatment. In addition to these applications, splints can be performed by using AM techniques. Sun et al. [41] provided AM splints for maxillofacial surgery that helped to identify the positions of mandible and maxilla as parts of facial bone treatment. These splints showed high accuracy levels and improved mechanical strength. For mandible fractures or defects, AM technology also helped to provide bone implants. As part of surgical treatment for square-shaped or asymmetric faces, titanium implants based on the anatomy of the patient’s mandible have been developed, and part of the mandible has been replaced with that. With this implant invention, it is much easier for surgeons to treat mandible defects and fractures that were very difficult to solve in the early stages [42]. When dealing with neurosurgery, additively manufactured skull models are also useful for skull defects. In the next sections, FFF is selected to be treated among the different AM techniques due to its various advantages.
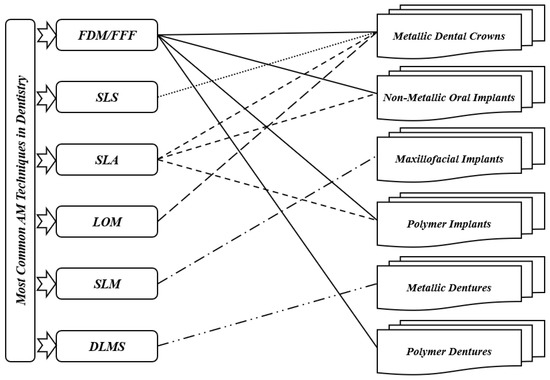
Figure 2. Most common AM techniques in dentistry.
3. AM Materials Used in Dentistry
Ceramics, metals, and polymers are the most common materials utilized for dental applications such as crowns, bridges, implants, splints, etc. It is true that ceramics and metals are generally preferred for many dental applications; however, polymers are used for biodegradable applications [5]. In literature, many materials have been used in dentistry. However, we present only some recent studies of AM materials applied to dentistry. Bae et al. [43] used SLM and cold isostatic pressing (CIP) techniques for 3Y-TZP ceramics for fabrication of dental crowns and prostheses and for dental restoration. According to their study, the maximum flexural strength and maximum densification were achieved through sintering at 1500 °C. Their method led to the establishment of SLS/CIP technology for 3Y-TZP ceramics. Next, Muta et al. [44] used the FFF technique for polyvinyl alcohol (PVA) material to fabricate provisional dental crowns. They found that with good accuracy, additively manufactured PVA models can be utilized to fabricate crowns. In the same period, a research paper on the use of alumina ceramics with the FFF technique to fabricate dental crowns was published by Arnesano et al. [45]. At 1150 °C, it was found that the used samples were pre-sintered, and the mechanical properties were like those of pure alumina. Their method was cost-effective and energy-efficient. Revilla-León et al. [46] used SLM and conventional milling (CM) techniques with cobalt chromium alloy (Co-Cr) to fabricate dental prostheses. When fabricating the samples by the two processes, it was found that the shear bond strength had no significant impact, while the roughness was enhanced with the SLM process. In the same period, Baciu et al. [47] published a research paper on using Co–Cr–W alloy with the SLM technique to fabricate dental bridges and inlays. A modification in roughness was found after fabricating specimens using different blasting media. For more information about the different materials used in dentistry, such as titanium and other alloys, the interested reader can refer to [5,6]. Table 1 presents a summary of the different results of recent material studies in dentistry. According to this table, there is no recent work studying AM-PLA for dental applications, while one can find many recent works that aimed to improve the mechanical properties of AM-PLA parts in different areas [19]. The researchers focused on studying the mechanical properties of AM-PLA parts, considering simple specimens (simple geometrical models); however, when dealing with dental applications, complex geometrical models that can largely affect the mechanical properties of the final printed parts should be considered.
Table 1. Recent works in additively manufactured materials for dental applications.
| Authors | Material | AM Technique | Dental Application | Results |
|---|---|---|---|---|
| Bae et al. [43] | 3Y-TZP ceramics | SLM + CIP | Dental crown, prostheses, restoration. | Foundation of SLS/CIP technology for 3Y-TZP dental ceramics |
| Muta et al. [44] | PVA | FDM | Provisional dental crown | Good accuracy |
| Arnesano et al. [45] | Alumina-Ceramic | FDM | Dental crown | Energy efficiency |
| Revilla-León et al. [46] | Co-Cr alloy | SLM + CM | Dental prostheses | Improved roughness with SLM process |
| Baciu et al. [47] | Co–Cr–W alloy | SLM | Dental inlays and bridges | Increased hardness |
In general, and according to our best knowledge, there have been no significant developments that use PLA materials in dental applications during the last three decades despite this material possessing many advantageous properties. In the next sections, we only focus on PLA material for dentistry in order to extend its applications considering several criteria such as sustainability, biodegradability, and biocompatibility. To meet this objective, some suggestions will be added, especially when dealing with composite PLA materials to improve their mechanical properties.
4. AM-PLA Material and Its Application to Dentistry
It is known that one of the most utilized AM materials is PLA since it is considered as a biocompatible, biodegradable, and nontoxic material [48,49,50,51]. Several works have been carried out to identify the design and process parameter effects on the quality of the final product [52]. PLA material is considered as a leading biomaterial for many medical applications and may replace conventional petrochemical-based polymers [53,54]. Due to its high potential for applicability in several areas such as medicine, chemistry, and biotechnology, it has been considered as a promising product under the concept of “green plastic”, since most of the polymers currently produced, are petroleum-based and non-renewable raw materials. The availability of pure lactic acid isomers is considered as an essential aspect for producing PLA with more interesting thermal and mechanical properties. In addition to its low environmental effects, it can be recycled in a traditional way [55]. This enhances its use as a promising polymer in medical applications, especially dental ones. Ramot et al. [56] reviewed the inflammatory reaction process that can be expected following PLA implantation, and they highlighted specific cases in which the inflammatory reaction could lead to some safety issues. In addition, some cases from different medical fields have been reported with the objective of demonstrating possible clinical side effects due to its use. Two kinds of biomaterials can be primarily utilized to prepare biodegradable scaffolds and medical models: natural and synthetic biomaterials. Usually, chitosan, fibrin, and collagen are utilized as natural medical polymeric materials that have excellent compatibility levels, stimulate cell adhesion and proliferation, and also maintain cell phenotypes; however, they can lead to poor mechanical strength (can be easily deformed). The degradation time, shape, and relative molecular mass of synthetic polymers such as PLA, PVA, and polycaprolactone (PCL) [57] can be precisely controlled. However, the polymer surfaces lack recognition sites for cell adhesion, which leads to heterogeneous cell distribution and then cell loss. Therefore, the mechanical performance of the polymer, such as fluidity and surface roughness, must be enhanced for it to be used in medical implants. Yue et al. [58] integrated more complex functions into polymers. After preparing antimicrobial composite resins, they found that antibacterial printed implants killed bacteria on contact without damaging human cells and may be eventually used to replace conventional dental fillings. Furthermore, their approach utilized for fabricating antimicrobial polymers can easily be transferred to other, nonmedical applications such as food packaging, water purification, or even toys for children. Despite PLA material having many advantages, it is difficult for the moment to use it in permanent replacements such as inlays and onlays since it may lead to total or partial loss of these replacements. So, for inlays and onlays, it is recommended to continue using ceramic/porcelain, gold, resin, zirconia materials (alloys), and metals (alloys) such as gold, palladium, chromium, nickel, etc., for permanent crowns and bridges. According to our best knowledge, dental PLA models such as replacement teeth are largely used for simulation needs (teaching, training, etc. This material can also be used in plates and tissues [1] for treating maxilla and mandible fractures. In certain periodical (provisional) parts (crowns, bridges, plates, etc.) this material can be used during the treatment period because of its biodegradability properties.
This entry is adapted from the peer-reviewed paper 10.3390/jfb14070334
This entry is offline, you can click here to edit this entry!
