Cerebrotendinous xanthomatosis (CTX) is an autosomal recessive disorder caused by pathogenic variants in CYP27A1, leading to a deficiency in sterol 27-hydroxylase. This defect results in the accumulation of cholestanol and bile alcohols in various tissues, including the brain, tendons, and peripheral nerves. Elevated levels of cholestanol are consistently observed. Most patients present normal or low serum cholesterol levels. The decrease in chenodeoxycholic acid (CDCA) leads to increased synthesis of cholesterol metabolites such as bile alcohols 23S-pentol and 25-tetrol 3-glucuronide, which may serve as surrogate follow-up markers in patients with CTX. Lipid abnormalities in CTX have clinical implications. Cholestanol deposition in tissues contributes to the clinical manifestations, including neurological symptoms and tendon xanthomas. Dyslipidemia and abnormal cholesterol metabolism may also contribute to the increased risk of atherosclerosis and cardiovascular complications observed in some CTX patients.
- cerebrotendinous xanthomatosis
- cholestanol
- cholesterol
- lipid
- chenodeoxycholic acid
1. Introduction
2. Cholesterol Metabolism in CTX
3. Metabolic Abnormalities and Laboratory Diagnosis of CTX
4. CTX Treatment and Its Effect on Metabolism
5. Diet Effects in CTX
This entry is adapted from the peer-reviewed paper 10.3390/brainsci13070979
References
- Höflinger, P.; Hauser, S.; Yutuc, E.; Hengel, H.; Griffiths, L.; Radelfahr, F.; Howell, O.W.; Wang, Y.; Connor, S.L.; Duell, P.B.; et al. Metabolic profiling in serum, cerebrospinal fluid, and brain of patients with cerebrotendinous xanthomatosis. J. Lipid Res. 2021, 62, 100078.
- Koyama, S.; Sekijima, Y.; Ogura, M.; Hori, M.; Matsuki, K.; Miida, T.; Harada-Shiba, M. Cerebrotendinous Xanthomatosis: Molecular Pathogenesis, Clinical Spectrum, Diagnosis, and Disease-Modifying Treatments. J. Atheroscler. Thromb. 2021, 28, 905–925.
- Nóbrega, P.R.; Bernardes, A.M.; Ribeiro, R.M.; Vasconcelos, S.C.; Araújo, D.A.B.S.; Gama, V.C.d.V. Cerebrotendinous Xanthomatosis: A practice review of pathophysiology, diagnosis, and treatment. Front. Neurol. 2022, 13, 1049850.
- Salen, G.; Steiner, R.D. Epidemiology, diagnosis, and treatment of cerebrotendinous xanthomatosis (CTX). J. Inherit. Metab. Dis. 2017, 40, 771–781.
- Nie, S.; Chen, G.; Cao, X.; Zhang, Y. Cerebrotendinous xanthomatosis: A comprehensive review of pathogenesis, clinical manifestations, diagnosis, and management. Orphanet J. Rare Dis. 2014, 9, 179.
- Gong, J.Y.; Setchell, K.D.R.; Zhao, J.; Zhang, W.; Wolfe, B.; Lu, Y.; Lackner, K.; Knisely, A.S.; Wang, N.L.; Hao, C.Z.; et al. Severe Neonatal Cholestasis in Cerebrotendinous Xanthomatosis: Genetics, Immunostaining, Mass Spectrometry. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 561–568.
- Verrips, A.; Dotti, M.T.; Mignarri, A.; Stelten, B.M.L.; Verma, S.; Federico, A. The safety and effectiveness of chenodeoxycholic acid treatment in patients with cerebrotendinous xanthomatosis: Two retrospective cohort studies. Neurol. Sci. 2020, 41, 943–949.
- Russell, D.W. The enzymes, regulation, and genetics of bile acid synthesis. Annu. Rev. Biochem. 2003, 72, 137–174.
- Clayton, P.T.; Verrips, A.; Sistermans, E.; Mann, A.; Mieli-Vergani, G.; Wevers, R. Mutations in the sterol 27-hydroxylase gene (CYP27A) cause hepatitis of infancy as well as cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2002, 25, 501–513.
- Atallah, I.; San Millán, D.; Benoît, W.; Campos-Xavier, B.; Superti-Furga, A.; Tran, C. Spinal Cerebrotendinous Xanthomatosis: A case report and literature review. Mol. Genet. Metab. Rep. 2021, 26, 100719.
- Mignarri, A.; Gallus, G.N.; Dotti, M.T.; Federico, A. A suspicion index for early diagnosis and treatment of cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2014, 37, 421–429.
- Berginer, V.M.; Abeliovich, D. Genetics of cerebrotendinous xanthomatosis (CTX): An autosomal recessive trait with high gene frequency in Sephardim of Moroccan origin. Am. J. Med. Genet. 1981, 10, 151–157.
- Stelten, B.M.L.; Dotti, M.T.; Verrips, A.; Elibol, B.; Falik-Zaccai, T.C.; Hanman, K.; Mignarri, A.; Sithole, B.; Steiner, R.D.; Verma, S.; et al. Expert opinion on diagnosing, treating and managing patients with cerebrotendinous xanthomatosis (CTX): A modified Delphi study. Orphanet J. Rare Dis. 2021, 16, 353.
- Amador, M.D.M.; Masingue, M.; Debs, R.; Lamari, F.; Perlbarg, V.; Roze, E. Treatment with chenodeoxycholic acid in Cerebrotendinous Xanthomatosis: Clinical, neurophysiological, and quantitative brain structural outcomes. J. Inherit. Metab. Dis. 2018, 41, 799–807.
- Duell, P.B.; Salen, G.; Eichler, F.S.; DeBarber, A.E.; Connor, S.L.; Casaday, L. Diagnosis, treatment, and clinical outcomes in 43 cases with Cerebrotendinous Xanthomatosis. J. Clin. Lipidol. 2018, 12, 1169–1178.
- Salen, G.; Grundy, S.M. The metabolism of cholestanol, cholesterol, and bile acids in cerebrotendinous xanthomatosis. J. Clin. Investig. 1973, 52, 2822–2835.
- Salen, G.; Shefer, S.; Berginer, V. Biochemical abnormalities in cerebrotendinous xanthomatosis. Dev. Neurosci. 1991, 13, 363–370.
- Petar Brlek, P.; Bulić, L.; Weinberger, D.G.; Bošnjak, J.; Pavlović, T.; Tomić, S.; Dupan, Z.K.; Borić, I.; Primorac, D. Successful Treatment of a Rare Cholesterol Homeostasis Disorder Due to CYP27A1 Gene Mutation with Chenodeoxycholic Acid Therapy. Biomedicines 2023, 11, 1430.
- Liang, Z.; Chen, Y.; Wang, L.; Li, D.; Yang, X.; Ma, G.; Wang, Y.; Li, Y.; Zhao, H.; Liang, Y.; et al. CYP27A1 inhibits bladder cancer cells proliferation by regulating cholesterol homeostasis. Cell Cycle 2019, 18, 34–45.
- Menkes, J.H.; Schimschock, J.R.; Swanson, P.D. Cerebrotendinous Xanthomatosis: The Storage of Cholestanol Within the Nervous System. Arch. Neurol. 1968, 19, 47–53.
- Inoue, K.; Kubota, S.; Seyama, Y. Cholestanol induces apoptosis of cerebellar neuronal cells. Biochem. Biophys. Res. Commun. 1999, 256, 198–203.
- Van Bogaert, L.; Philippart, M.; De Barsy, T. Nouvelles recherches sur la xanthomatose cérébro-tendineuse . Rev. Neurol. 1969, 121, 98–100.
- Martini, G.; Mignarri, A.; Ruvio, M.; Valenti, R.; Franci, B.; Del Puppo, M.; Federico, A.; Nuti, R.; Dotti, M.T. Long-term bone density evaluation in cerebrotendinous xanthomatosis: Evidence of improvement after chenodeoxycholic acid treatment. Calcif. Tissue Int. 2013, 92, 282–286.
- Bonney, H.; de Silva, R.; Giunti, P.; Greenfeld, J.; Hunt, B.; Ataxia, U.K. Management of the Ataxias towards Best Clinical Practice. 2016. Available online: https://www.ataxia.org.uk/wp-content/uploads/2020/11/Ataxia_UK_Medical_Guidelines_Third_Edition._v3m_Dec_2016_-_updated_Sep_2019.pdf (accessed on 30 June 2021).
- Salen, G.; Berginer, V.; Shore, V.; Horak, I.; Horak, E.; Tint, G.S.; Shefer, S. Increased concentrations of cholestanol and apolipoprotein B in the cerebrospinal fluid of patients with cerebrotendinous xanthomatosis. Effect of chenodeoxycholic acid. N. Engl. J. Med. 1987, 316, 1233–1238.
- Samenuk, P.; Koffman, B.M. Chenodeoxycholic treatment of cerebrotendinous xanthomatosis. Neurology 2001, 56, 695–696.
- Mignarri, A.; Rossi, S.; Ballerini, M.; Gallus, G.N.; Del Puppo, M.; Galluzzi, P.; Federico, A.; Dotti, M.T. Clinical relevance and neurophysiological correlates of spasticity in cerebrotendinous xanthomatosis. J. Neurol. 2011, 258, 783–790.
- Ginanneschi, F.; Mignarri, A.; Mondelli, M.; Gallus, G.N.; Del Puppo, M.; Giorgi, S.; Federico, A.; Rossi, A.; Dotti, M.T. Polyneuropathy in cerebrotendinous xanthomatosis and response to treatment with chenodeoxycholic acid. J. Neurol. 2013, 260, 268–274.
- Burnett, J.R.; Moses, E.A.; Croft, K.D.; Brown, A.J.; Grainger, K.; Vasikaran, S.D.; Leitersdorf, E.; Watts, G.F. Clinical and biochemical features, molecular diagnosis and long-term management of a case of cerebrotendinous xanthomatosis. Clin. Chim. Acta 2001, 306, 63–69.
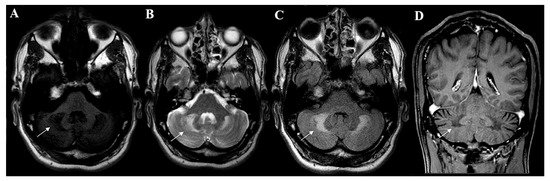
- Stelten, B.M.L.; Nijeholt, G.J.L.A.; Hendriks, E.; Kluijtmans, L.A.J.; Wevers, R.A.; Verrips, A. Long-term MRI findings in patients with Cerebrotendinous Xanthomatosis treated with chenodeoxycholic acid. Neurology 2022, 99, 559–566.
- Mignarri, A.; Magni, A.; Del Puppo, M.; Gallus, G.N.; Björkhem, I.; Federico, A.; Dotti, M.T. Evaluation of cholesterol metabolism in cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2016, 39, 75–83.
- De Sain-van der Velden, M.G.; Verrips, A.; Prinsen, B.H.; de Barse, M.; Berger, R.; Visser, G. Elevated cholesterol precursors other than cholestanol can also be a hallmark for CTX. J. Inherit. Metab. Dis. 2008, 31 (Suppl. S2), S387–S393.
- Panzenboeck, U.; Andersson, U.; Hansson, M.; Sattler, W.; Meaney, S.; Björkhem, I. On the mechanism of cerebral accumulation of cholestanol in patients with cerebrotendinous xanthomatosis. J. Lipid Res. 2007, 48, 1167–1174.
- DeBarber, A.E.; Connor, W.E.; Pappu, A.S.; Merkens, L.S.; Steiner, R.D. ESI-MS/MS quantification of 7α-hydroxy-4-cholesten-3-one facilitates rapid, convenient diagnostic testing for cerebrotendinous xanthomatosis. Clin. Chim. Acta. 2010, 411, 43–48.
- Di Taranto, M.D.; Gelzo, M.; Giacobbe, C.; Gentile, M.; Marotta, G.; Savastano, S.; Dello Russo, A.; Fortunato, G.; Corso, G. Cerebrotendinous xanthomatosis, a metabolic disease with different neurological signs: Two case reports. Metab. Brain Dis. 2016, 31, 1185–1188.
- Björkhem, I. Cerebrotendinous xanthomatosis. Curr. Opin. Lipidol. 2013, 24, 283–287.
- Haas, D.; Gan-Schreier, H.; Langhans, C.D.; Rohrer, T.; Engelmann, G.; Heverin, M.; Russell, D.W.; Clayton, P.T.; Hoffmann, G.F.; Okun, J.G. Differential diagnosis in patients with suspected bile acid synthesis defects. World J. Gastroenterol. 2012, 18, 1067–1076.
- Verrips, A.; Wevers, R.A.; Van Engelen, B.G.; Keyser, A.; Wolthers, B.G.; Barkhof, F.; Stalenhoef, A.; De Graaf, R.; Janssen-Zijlstra, F.; Van Spreeken, A.; et al. Effect of simvastatin in addition to chenodeoxycholic acid in patients with cerebrotendinous xanthomatosis. Metabolism 1999, 48, 233–238.
- Bel, S.; Garcia-Patos, V.; Rodriguez, L.; Selvan, A.; Diaz, P.; Wolthers, B.G.; Castells, A. Cerebrotendinous xanthomatosis. J. Am. Acad. Dermatol. 2001, 45, 292–295.
- Stelten, B.M.L.; Huidekoper, H.H.; van de Warrenburg, B.P.C.; Brilstra, E.H.; Hollak, C.E.M.; Haak, H.R.; Kluijtmans, L.A.J.; Wevers, R.A.; Verrips, A. Long-term treatment effect in cerebrotendinous xanthomatosis depends on age at treatment start. Neurology 2019, 92, e83–e95.
- Van Heijst, A.F.; Verrips, A.; Wevers, R.A.; Cruysberg, J.R.; Renier, W.O.; Tolboom, J.J. Treatment and follow-up of children with cerebrotendinous xanthomatosis. Eur. J. Pediatr. 1998, 157, 313–316.
- Salen, G.; Tint, G.S.; Eliav, B.; Deering, N.; Mosbach, E.H. Increased formation of ursodeoxycholic acid in patients treated with chenodeoxycholic acid. J. Clin. Investig. 1974, 53, 612.
- Kuriyama, M.; Tokimura, Y.; Fujiyama, J.; Utatsu, Y.; Osame, M. Treatment of cerebrotendinous xanthomatosis: Effects of chenodeoxycholic acid, pravastatin, and combined use. J. Neurol. Sci. 1994, 125, 22–28.
- Björkhem, I.; Skrede, S.; Buchmann, M.S.; East, C.; Grundy, S. Accumulation of 7α-hydroxy-4-cholesten-3-one and cholesta-4, 6-dien-3-one in patients with cerebrotendinous xanthomatosis: Effect of treatment with chenodeoxycholic acid. Hepatology 1987, 7, 266–271.
- Björkhem, K.; Muri-Boberg, E.; Leitersdorf. Inborn errors in bile acid biosynthesis and storage of sterols other than cholesterol. In The Metabolic Bases of Inherited Diseases; Scriver, C.R., Beaudet, A.L., Sly, W.S., Valle, D., Eds.; McGraw Hill Publishing Co.: New York, NY, USA, 2001; pp. 2961–2988.
- Salen, G.; Shefer, S.; Berginer, V.M. Familial diseases with storage of sterols other than cholesterol: Cerebrotendinous xanthomatosis and sitosterolemia with xanthomatosis. In The Metabolic Basis of Inherited Disease, 5th ed.; Stanbury, J.B., Wyngaarden, J., Fredrickson, D.S., Eds.; McGraw-Hill Book: New York, NY, USA, 1983; pp. 713–730.
- Oftebro, H.; Bjorkhem, I.; Skrede, S.; Schreiner, A.; Pederson, J.I. Cerebrotendinous xanthomatosis: A defect in mitochondrial 26-hydroxylation required for normal biosynthesis of cholic acid. J. Clin. Investig. 1980, 65, 1418–1430.
- Salen, G.; Batta, A.K.; Tint, G.S.; Shefer, S. Comparative effects of lovastatin and chenodeoxycholic acid on plasma cholestanol levels and abnormal bile acid metabolism in cerebrotendinous xanthomatosis. Metabolism. 1994, 43, 1018–1022.
- Wolthers, B.G.; Volmer, M.; van der Molen, J.; Koopman, B.J.; de Jager, A.E.; Waterreus, R.J. Diagnosis of cerebrotendinous xanthomatosis (CTX) and effect of chenodeoxycholic acid therapy by analysis of urine using capillary gas chromatography. Clin. Chim. Acta. 1983, 131, 53–65.
- Batta, A.K.; Shefer, S.; Batta, M.; Salen, G. Effect of chenodeoxycholic acid on biliary and urinary bile acids and bile alcohols in cercbrotendinous xanthomatosis: Monitoring by high performance liquid chromatography. J. Lipid Res. 1985, 26, 690–698.
- Batta, A.K.; Salen, G.; Shefer, S.; Tint, G.S.; Batta, M. Increased plasma bile alcohol glucuronides in patients with cerebrotendinous xanthomatosis: Effect of chenodeoxycholic acid. J. Lipid Res. 1987, 28, 1006–1012.
- Batta, A.K.; Salen, G.; Tint, G.S. Hydrophilic 7β-hydroxy bile acids, lovastatin, and cholestyramine are ineffective in the treatment of Cerebrotendinous Xanthomatosis. Metabolism 2004, 53, 556–562.
- Setoguchi, T.; Salen, G.; Tint, G.S.; Mosbach, E.H. A biochemical abnormality in cerebrotendinous xanthomatosis. Impairment of bile acid biosynthesis associated with incomplete degradation of the cholesterol side chain. J. Clin. Investig. 1974, 53, 1393–1401.
- Tint, G.S.; Ginsberg, H.; Salen, G.; Le, N.; Shefer, S. Chenodeoxycholic acid normalizes elevated lipoprotein secretion and catabolism in cerebrotendinous xanthomatosis. J. Lipid Res. 1989, 30, 633–640.
- Blaabjerg, M.; Marjanovic, D. Cerebrotendinøs xantomatose er en sjælden neurologisk sygdom med en specifik behandling . Ugeskr Laeger 2013, 175, 285–286. (In Danish)
- Salen, G.; Meriwether, T.W.; Nicolau, G. Chenodeoxycholic acid inhibits increased cholesterol and cholestanol synthesis in patients with cerebrotendinous xanthomatosis. Biochem. Med. 1975, 14, 57–74.
- Kinoshita, M.; Kawamura, M.; Fujita, M.; Hirota, D.; Suda, T.; Taki, M.; Kusano, J.; Takao, K.; Takenaka, H.; Kubota, S.; et al. Enhanced susceptibility of LDL to oxidative modification in a CTX patient:—role of chenodeoxycholic acid in xanthoma formation. J. Atheroscler. Thromb. 2004, 11, 167–172.
- Bjorkhem, I.; Skrede, S. Familial disease with storage of sterols other than cholesterol: Cerebrotendinous xanthomatosis and phytosterolemia. In The Metabolic Basis of Inherited Disease, 6th ed.; Scriver, C.R., Beaudet, A.L., Sly, W.S., Valle, D., Eds.; McGraw-Hill: New York, NY, USA, 1989; pp. 1283–1302.
- Goldstein, J.L.; Ho, Y.K.; Basu, S.K.; Brown, M.S. Binding site of macrophages that mediate uptake and degradation of acetylated low density lipoprotein, producing massive cholesterol deposition. Proc. Natl. Acad. Sci. USA 1979, 76, 333–337.
- Sparrow, C.P.; Parthasarathy, S.; Steinberg, D. A macrophage receptor that recognizes oxidized LDL but not acetylated LDL. J. Biol. Chem. 1989, 264, 2599–2604.
- Witztum, J.L.; Steinberg, D. Role of oxidized low density-lipoprotein in atherogenesis. J. Clin. Investig. 1991, 88, 1785–1792.
- Koopman, B.J.; Wolthers, B.G.; van der Molen, J.C.; Waterreus, R.J. Bile acid therapies applied to patients suffering from cerebrotendinous xanthomatosis. Clin. Chim. Acta 1985, 152, 115–122.
- Ellis, E.; Axelson, M.; Abrahamsson, A.; Eggertsen, G.; Thörne, A.; Nowak, G.; Ericzon, B.-G.; Björkhem, I.; Einarsson, C. Feedback regulation of bile acid synthesis in primary human hepatocytes: Evidence that CDCA is the strongest inhibitor. Hepatology 2003, 38, 930–938.
- Sekijima, Y.; Koyama, S.; Yoshinaga, T.; Koinuma, M.; Inaba, Y. Nationwide survey on cerebrotendinous xanthomatosis in Japan. J. Hum Genet. 2018, 63, 271–280.
- Berginer, V.M.; Berginer, J.; Korczyn, A.D.; Tadmor, R. Magnetic resonance imaging in cerebrotendinous xanthomatosis: A prospective clinical and neuroradiological study. J. Neurol. Sci. 1994, 122, 102–108.
- Mandia, D.; Besson, G.; Lamari, F.; Castelnovo, G.; Curot, J.; Duval, F.; Giral, P.; Lecerf, J.M.; Roland, D.; Pierdet, H.; et al. Cholic acid as a treatment for cerebrotendinous xanthomatosis in adults. J. Neurol. 2019, 266, 2043–2050.
- Pierre, G.; Setchell, K.; Blyth, J.; Preece, M.A.; Chakrapani, A.; McKiernan, P. Prospective treatment of cerebrotendinous xanthomatosis with cholic acid therapy. J. Inherit. Metab. Dis. 2008, 31, S241–S245.
- Makishima, M.; Okamoto, A.Y.; Repa, J.J.; Tu, H.; Learned, R.M.; Luk, A.; Hull, M.V.; Lustig, K.D.; Mangelsdorf, D.J.; Shan, B. Identification of a nuclear receptor for bile acids. Science 1999, 284, 1362–1365.
- Parks, D.J.; Blanchard, S.G.; Bledsoe, R.K.; Chandra, G.; Consler, T.G.; Kliewer, S.A.; Stimmel, J.B.; Willson, T.M.; Zavacki, A.M.; Moore, D.D.; et al. Bile acids: Natural ligands for an orphan nuclear receptor. Science 1999, 284, 1365–1368.
- Wang, H.B.; Chen, J.; Hollister, K.; Sowers, L.C.; Forman, B.M. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol. Cell 1999, 3, 543–553.
- Einarsson, C.; Hillebrant, C.G.; Axelson, M. Effects of treatment with deoxycholic acid and chenodeoxycholic acid on the hepatic synthesis of cholesterol and bile acids in healthy subjects. Hepatology 2001, 33, 1189–1193.
- Huidekoper, H.H.; Vaz, F.M.; Verrips, A.; Bosch, A.M. Hepatotoxicity due to chenodeoxycholic acid supplementation in an infant with cerebrotendinous xanthomatosis: Implications for treatment. Eur. J. Pediatr. 2016, 175, 143–146.
- Medscape. Available online: https://emedicine.medscape.com/article/1418820-overview (accessed on 30 June 2021).
- Bartholdi, D.; Zumsteg, D.; Verrips, A.; Wevers, R.A.; Sistermans, E.; Hess, K.; Jung, H.H. Spinal phenotype of Cerebrotendinous Xanthomatosis—A pitfall in the diagnosis of multiple sclerosis. J. Neurol. 2004, 251, 105–107.
- Lewis, B.; Mitchell, W.D.; Marenah, C.B.; Cortese, C.; Reynolds, E.H.; Shakir, R. Cerebrotendinous xanthomatosis: Biochemical response to inhibition of cholesterol synthesis. Br. Med. J. 1983, 287, 21–22.
- Nakamura, T.; Matsuzawa, Y.; Takemura, K.; Kubo, M.; Miki, H.; Tarui, S. Combined treatment with chenodeoxycholic acid and pravastatin improves plasma cholestanol levels associated with marked regression of tendon xanthomas in cerebrotendinous xanthomatosis. Metabolism 1991, 40, 741–746.
- Black, M.M.; Gawkrodger, D.J.; Seymour, C.A.; Weismann, K. Metabolic and nutritional disorders. In Rook/Wilkinson/Ebling: Textbook of Dermatology, 6th ed.; Champion, R.H., Burton, J.L., Burns, T., Breathnach, S., Eds.; Blackwell Science: London, UK, 1998; pp. 2577–2677.
- Peynet, J.; Laurent, A.; De Liege, P.; Lecoz, P.; Gambert, P.; Legrand, A.; Mikol, J.; Warnet, A. Cerebrotendinous xanthomatosis: Treatments with simvastatin, lovastatin, and chenodeoxycholic acid in 3 siblings. Neurology 1991, 41, 434–436.
- Koopman, B.J.; Wolthers, B.G.; van der Moten, J.C.; Nagel, G.T.; Waterreus, R.J.; Oosterhuis, H.J.G.H. Capillary gas chromatographic determinations of urinary bile acids and bile alcohols in CTX-patients proving the ineffectivity of ursodeoxycholic acid treatment. Clin. Chim. Acta 1984, 142, 103–111.
- Koopman, B.J.; Wolthers, B.G.; van der Molen, J.C.; Nagel, G.T.; Kruizinga, W. Abnormal urinary bile acids in a patient suffering from cerebrotendinous xanthomatosis during oral administration of ursodeoxycholic acid. Biochim. Biophys. Acta 1987, 917, 238–246.
- Dotti, M.T.; Lütjohann, D.; von Bergmann, K.; Federico, A. Normalisation of serum cholestanol concentration in a patient with Cerebrotendinous Xanthomatosis by combined treatment with chenodeoxycholic acid, simvastatin and LDL apheresis. Neurol. Sci. 2004, 25, 185–191.
- Ito, S.; Kuwabara, S.; Sakakibara, R.; Oki, T.; Arai, H.; Oda, S.; Hattori, T. Combined treatment with LDL-apheresis, chenodeoxycholic acid and HMG-CoA. J. Neurol. Sci. 2003, 216, 179–182.
- Byun, D.S.; Kasama, T.; Shimizu, T.; Yorifuji, H.; Seyama, Y. Effect of cholestanol feeding on sterol concentrations in the serum, liver, and cerebellum of mice. J. Biochem. 1988, 103, 375–379.
- Shefer, S.; Hauser, S.; Salen, G.; Zaki, F.G.; Bullock, J.; Salgado, E.; Shevitz, J. Comparative effects of cholestanol and cholesterol on hepatic sterol and bile acid metabolism in the rat. J. Clin. Investig. 1984, 74, 1773–1781.
- Yousuke, S. Cholestanol metabolism, molecular pathology, and nutritional implications. J. Med. Food 2003, 6, 217–224.
- Valdivielso, P.; Calandra, S.; Duran, J.C.; Garuti, R.; Herrera, E.; Gonzalez, P. Coronary heart disease in a patient with cerebrotendinous xanthomatosis. J. Intern Med. 2004, 255, 680–683.
- Malco, R.; Nestor, W.; Marcelo, M. Cardiac involvement in movement disorders. Mov. Disord. Clin. Pract. 2021, 8, 651–668.
- Zhang, S.; Li, W.; Zheng, R.; Zhao, B.; Zhang, Y.; Zhao, D.; Zhao, C.; Yan, C.; Zhao, Y. Cerebrotendinous xanthomatosis with peripheral neuropathy: A clinical and neurophysiological study in Chinese population. Ann. Transl. Med. 2020, 8, 1372.
