Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Neurosciences
Multiple sclerosis (MS) is a disabling immune-mediated demyelinating neurodegenerative disease with an estimated prevalence of 1 in 1000 in populations of European descent. It primarily affects females (F:M = 2–3:1) mainly between the ages of 15 and 55 years.
- multiple sclerosis
- pediatric-onset multiple sclerosis
- nutrition
- diet
- gut microbiota
- gut-brain axis
- blood-brain barrier
- vitamin D
1. The Gut-Brain Axis in MS
The MS GBA contemplates a dysbiosis-induced pro-inflammatory gut environment responsible for a leaky gut [14] allowing the emergence of activated myelin-specific bystander T cells which regulate the cytokine milieu in the central nervous system (CNS) and the function of neurons and glial cells [13]. Clinical [relapsing-remitting (RR) course with subsequent progressive disability] and pathological similarities between MS and the murine model of experimental autoimmune encephalomyelitis (EAE) allow the latter to be considered as a suitable model for the study of MS. Through this model, studies have confirmed that high-fat diets, especially if high in saturated fats, are relevant MS triggers [15,16]. Obesity itself, due to the adipose tissue‘s inflammatory properties mediated by adipokines production (e.g., adiponectin), has been suggested to contribute to the pro-inflammatory status of MS, which also has impacts on the quiescence of CNS-resident microglia [17,18].
1.1. The Intestinal Barrier
The intestinal barrier is a complex functional unit composed of mucosal and luminal elements (i.e., epithelial cells layer; mucosal barrier; innate and acquired immune components); neuroenteric, vascular, and endocrine systems; digestive enzymes; and gut microbiota (GM). This barrier plays a key role in protecting against enteric organisms, their toxins, and bio-products associated with the health and disease susceptibility of organs/systems [19,20]. The recently discovered gut-vascular barrier controls the translocation of gut bacteria and antigens into the bloodstream [21,22].
The gut-(liver)-brain axis connects the GM, neuroendocrine and neuroimmune systems, autonomic nervous system, and enteric nervous system with the CNS [13,23]. The GM consists of trillions of commensal microorganisms that maintain the integrity of the mucosal barrier and contribute to normal host physiology [19]. Factors such as an unbalanced diet, infections, antibiotics, stress, and environmental factors can lead to dysbiosis and increased intestinal permeability [24,25,26]. Dysbiosis is associated with various diseases, including gastrointestinal and systemic inflammatory diseases [27].
GM dysbiosis can also impact the onset and progression of neurological disorders such as MS by affecting metabolic pathways and interacting with host immunity [28,29,30,31,32].
Identifying a characteristic/diagnostic composition of microbial communities associated with the gut microbiota of MS patients is challenging due to variations between studies and individual profiles [31,32]. However, reduced microbial diversity is commonly observed, which is characterized by an increased Firmicutes/Bacteroides ratio and prevalence of species producing endogenous ethanol, lipopolysaccharide, and reactive oxygen species [33,34].
These biochemical factors, along with pro-inflammatory T-helper types and cytokine patterns, contribute to intestinal inflammation and impairment of the barrier function (leaky gut) [29,35].
In an MS mouse model, Streptococcus thermophilus ST285 has been observed to switch cytokine responses to myelin peptides from pro-inflammatory to anti-inflammatory patterns [36]. The significance of increased abundance of Akkermansia species in MS patients and the EAE mouse model is still debated, with suggestions of a compensatory effect rather than a direct association with EAE progression and MS pathogenesis [37,38].
Considering differences in patient selection methods, environmental factors, and dietary habits, certain species (e.g., Faecalibacterium, Eubacterium rectale, Corynebacterium, Fusobacteria, Bacteroides stercoris, and Bacteroides coprocola) [29,39] are generally reduced in MS patients compared to healthy controls in some studies. These species are responsible for decreased production of metabolites such as bacterial lipid 654, a Toll-like receptor 2 ligand derived from gastrointestinal and oral bacteria [40,41,42], and short-chain fatty acids (SCFAs) such as butyrate and propionic acid [14,43,44].
SCFAs, produced by the colonic fermentation of dietary fibers and resistant starch, are speculated to play a key role in neuro-immunoendocrine regulation [45]. A secondary increase in species related to oxidative levels is observed in progressive MS or more severe disease forms [46,47,48], and it is sufficient to induce EAE sensitivity [49,50]. Saturated fatty acids (FAs) have a close relationship with autoimmunity phenomena in MS, as their concentration and composition regulate immune cell polarization, differentiation, and function, with a protective role in blood-brain barrier function. They are critical players in CNS chronic inflammation, progressive degeneration, and remyelination [34,51].
Additionally, a negative association with polysaccharide-digesting bacteria such as B. thetaiotaomicron is often observed [52].
1.2. The Blood-Brain Barrier
The BBB plays a crucial role in maintaining the homeostasis of the brain microenvironment, and its dysfunction is implicated in the pathogenesis of various neurological diseases, including MS. The BBB consists of multiple biological barriers including the proper blood-brain barrier, the blood-cerebrospinal fluid barrier, and the arachnoid barrier [22,53] (Figure 1).
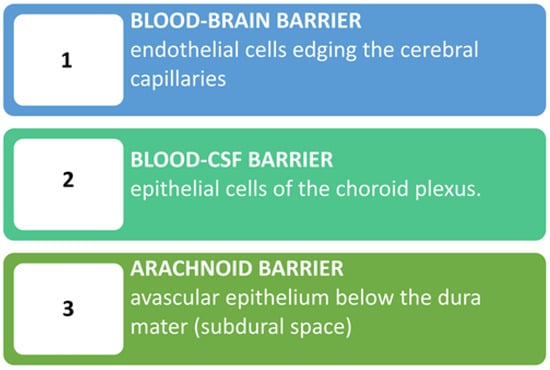
Figure 1. The blood-brain barrier consists of biological barriers formed by different cells at three key interfaces. The 1st layer is made up of microvascular endothelial cells that line the cerebral capillaries and permeate the brain and spinal cord. The 2nd barrier is made up of the epithelial cells of the choroid plexus. This layer, being more permeable to proteins thanks to the presence of a fenestrated endothelium below a cuboidal epithelium, may regulate brain permeability under conditions of gut inflammation. The 3rd barrier is situated below the dura mater and contributes little to blood-brain exchange due to its avascular nature and relatively small surface area compared to other barriers. CSF: Cerebrospinal fluid.
The integrity of the BBB can be influenced by the GM, as bacterial antigens such as lipopolysaccharide (LPS) and SCFAs can travel from the leaky gut to the brain endothelial cells’ Toll-like receptors 2 through the bloodstream. In the EAE murine model, high-fat-diet-induced obesity resulted in severe disease accompanied by gut dysbiosis, increased gut permeability, and systemic inflammation, suggesting a role for gut barrier modulation in obesity-induced MS severity [39]. In a similar EAE model, obesity induced by a high-fat diet also led to BBB disruption, which allows the infiltration of monocytes/macrophages and activation of resident microglia, ultimately exacerbating CNS inflammation in EAE [54], likely mediated by IL-6 and CCL-2 [55].
The activation of pro-inflammatory pathways disrupts the delicate balance between protective and harmful reactions. It can induce the release of Vascular Endothelial Growth Factor B/VEGF-B and Tumor Growth Factor/TGF-alpha from microglia, which activates astrocytes and exerts detrimental effects on neurons. The Th17 cytokines IL-17A and IL-17F appear to be pivotal in triggering BBB disturbance [56,57]. As mentioned earlier, SCFAs not only have effects on the colon and peripheral tissues but also play a crucial role in the communication between the GM, gut, and brain. They can cross the BBB through endothelial cell monocarboxylate transporters and a) upregulate the expression of tight junction proteins essential for BBB integrity, b) affect neuroinflammation by influencing glial cell morphology and function, and modulating levels of neurotrophic factors [45]. Moreover, due to its bidirectional nature, GBA neuroinflammation could result in further intestinal inflammation as the disease progresses by affecting efferent cholinergic transmission [13,58,59].
2. Diets and Dietary Supplementations
2.1. Dietary Influence on MS
Studies in adults with MS suggest that diet-related inflammation increases the odds of developing the disease [60,61]. The prevalence of Westernized diets, characterized by ultra-processed foods that are high in salt, saturated and trans fatty acids [62] and low in fibers and flavonoids, may contribute to the upregulation of pro-inflammatory compounds, gut dysbiosis, neuroinflammation, and neurodegeneration [63,64,65]. The high salt content in processed foods has been associated with disease exacerbation and the development of new lesions, although the evidence is debated [66,67,68]. Saturated fats activate pro-inflammatory Toll-like receptors (TLRs) and increase NF-κB, which affects the innate immune system [7]. They also play a role in GM-mediated inflammation in MS development and relapse risk, as seen in the EAE model [39,54,55] or in MS patients. [63,65,69].
Conversely, higher fish consumption, particularly oily fish rich in vitamin D and omega-3 fatty acids, is associated with a lower risk of CNS demyelination [70]. Flavonoids, polyphenolic compounds that are abundant in fruits and vegetables, have shown a protective role in MS development in experimental models [71,72]. Non-fermentable cellulose fiber may prevent changes in GM composition and T cell responses associated with CNS autoimmunity in MS [50]. The proper functioning of all players in the gut-brain axis is crucial for managing the impact of MS [Table 1].
Several diets have been proposed for MS based on assumptions such as existing food allergies, gluten sensitivity, hypovitaminosis, or the concept of a healthy diet (e.g., Mediterranean diets, Paleolithic diet) [73]. Although a diet rich in fruits and vegetables seems logically protective against relapses and disease progression [74], larger and better-conducted studies are needed to confirm this correlation due to conflicting evidence [75].
Table 1. Synopsis of the main specific diets proposed over time in patients with multiple sclerosis.
| Diet Name | Main Characteristics |
|---|---|
| Allergen free/milk free | Hypoallergenic diet based on the unproven hypothesis of the association between MS and external allergens [76]. The milk protein butyrophilin has been implicated through antigenic mimicry with myelin oligodendrocyte glycoprotein in EAE [77] as well as in MS patients [78]. Some studies with questionnaires suggest an inverse relationship between total dairy intake and MS disability severity [79,80] with an inverse relationship between whole grain intake and MS-related disability [80]. |
| Gluten free | Among studies, only one clinical trial gave meaningful results, but there are methodological limitations [81,82,83]. All in all, the current level of evidence is inadequate to state whether gluten plays a role in MS [82]. |
| Mega Ascorbic | High in vitamin C diet. No well-defined link between MS and vitamin C [84]. |
| Multi Vitaminic | Multi vitaminic supplementation (e.g., A and D): quite convincing data show that higher vitamin intake/serum levels correlate with lower risk of MS development but not convincing on the contrary [85]. Possible detrimental effects of overdosing require vitamin-level monitoring [86,87]. |
| Hebener’s | Self-reported disease stability/amelioration in one study with fish oil and antioxidant drugs supplementation + Ω-6 restriction [88]. |
| Kousmine | High in polyunsaturated fats/low in animal fats diet to counteract a possibly increased membrane permeability [89,90,91]. |
| Swank (low saturated fats) | Low-saturated fats (<20 g fat/day or <20% total calories): reported lower death rates and better outcome in the more adherent patients and those with lower disability at entry [92,93]. |
| Mediterranean diets (MD) | Common features include emphasis on vegetables, fruits, beans, nuts, seeds, breads, unrefined grains, and olive oil; inclusion of fish and wine; minimal intake of full-fat dairy products and possibly lean meats [94,95]. Conflicting results on whether lean and unprocessed red meat is detrimental [96,97,98]. It is considered beneficial for its antioxidant properties. Negatively associated with neurological and fatigue symptoms. Adherence should be monitored through validated tests [e.g., Predimed for adults [94] and KidMed for children [99] |
| Mediterranean/DASH | It derives from the Mediterranean Dietary Approaches to Stop Hypertension (DASH) [100,101]. |
| MIND | The Mediterranean/Intervention for Neurodegenerative Delay (MIND) is a combination of MD and DASH [100,101,102]. |
| Paleolithic1 | Consists of high-quality foods full of nutrients and fiber and with less artificial sugar and salt compared to present-day diets [103]. Nutrients included in this diet are essential to myelin growth and repair. Typically, it does not permit consumption of dairy or grain products. |
| Modified Paleolithic (MD-PI intervention) |
This diet is rich in α-lipoic acid and polyphenols. It has commonalities with MD including avoidance of high-fat meats/ultra-processed foods with added sugar, sodium, and hydrogenated fats [104,105,106]. |
| Wahls™ Paleo diet | Differences from a traditional Paleo diet: exclusion of eggs; limited animal and fish protein. It allows legumes (e.g., soy milk), two servings of gluten-free grains (e.g., rice) per week; it specifies nine cups of fruits and vegetables (F/V)/day with 1/3 each from dark-green leafy vegetables, sulfur-rich vegetables, and deeply colored F/V; seaweed, algae and nutritional yeast are encouraged [107,108]. |
| Wahls/Elim Paleo | This is a paleo version modified by adding a restriction of lectins to reduce intestinal permeability and CNS inflammation [107,108]. |
| Overcoming MS (OMS) | Minimized saturated fats and plant-based, whole-food diet plus seafood [79,109]. |
| Ketogenic diet (KD) | Eliminating all/almost all carbohydrates and increasing the intake of proteins. KD combined with a modified MD have been suggested to improve neuroinflammation in MS [110,111]. |
| Energy restriction (ER) | Chronic ER/Intermittent energy restriction (IER) determines a switch from glucose to fatty acids and ketones as the major fuel source for cells [112,113,114,115]. Mice fed a “fasting mimicking” diet (very low-calorie diet lasting for 3 days every 7 days) exhibited delayed onset, reduced incidence, and decreased severity of EAE. Histological findings show reduced immune cell infiltration and demyelination in the spinal cord [116]. |
| McDougall Diet | A low-fat (10–15% of calories from fat), starch-based, vegan diet with no oils permitted. For 7 days, produced significant favorable changes in commonly tested biomarkers used to predict future risks for cardiovascular disease and metabolic diseases [75,117]. It appeared safe and effective in preventing clinical attacks/new MRI lesions. Drawback = long-term adherence [118]. |
Abbreviations: DASH, Dietary Approaches to Stop Hypertension; ER, Energy restriction; F/V, fruit and vegetables; KD, Ketogenic diet; MD, Mediterranean diet; MIND, Mediterranean/Intervention for Neurodegenerative Delay; MS, multiple sclerosis; OMS Overcoming MS; PI, Paleolithic intervention.
A recent meta-analysis [119,120] examined 11 studies (involving 608 participants) that investigated whole dietary approaches without concomitant interventions with appropriate control groups and outcome measurements. The modified Paleolithic and modified Mediterranean diets improved fatigue and quality of life compared to the control diets. Low-fat diets improved fatigue but not quality of life. Fasting, calorie-restricted, and anti-inflammatory diets did not significantly affect fatigue or quality of life, and ketogenic diets fell somewhere in between. GM appeared to be a pivotal element influenced not only by the type of diet but also by therapies. In fact, vitamin D supplementation, commonly prescribed for MS [121], may also influence gut bacterial populations by increasing the frequency of certain genera [122]. In vitro studies have shown that some MS drugs (e.g., fingolimod and teriflunomide) also have anti-inflammatory and antioxidant effects and can shape GM and inhibit the growth of neurotoxin-secreting gut bacteria. [123] Regular exercise has been shown to have positive effects on sleep, depression, paresthesia, fatigue, and cognitive performance [124,125]. However, the impact of physical activity on GM composition and microbial metabolites in the gastrointestinal tract in MS patients remains to be studied [126].
Other factors, such as socioeconomic status, quality of life, and personal motivation, may contribute to the uncertainty surrounding diet-related results. Adherence to an MS-specific diet is associated with higher socioeconomic status, better quality of life, and higher nutritional quality [127]. Enhancing personal motivation and ensuring positive support from study staff and family members are opportunities for future dietary intervention studies in MS, as they can improve adherence and reduce attrition [118,128]. Additionally, strategies should be developed to tailor study diets to the preferences of both individuals with MS and their household members to reduce feelings of burden and improve diet observance [118,128].
Progressive MS disabilities can impact grocery shopping, cooking, and eating, leading to weight loss, isolation, and dysphagia in advanced stages [129,130]. Proper nutritional support and guidance are necessary to ensure a correct diet at any age, starting from the early stages of the disease [120,131,132,133]. On the other hand, an unbalanced diet coupled with reduced physical activity can result in overweight/obesity, which triggers EAE and MS onset and progression [17,54,55,134,135,136,137,138]. Overweight and obesity are also associated with cardiovascular disease, which contributes to more rapid disability progression in MS [139,140,141].
Considering the role of GM in MS onset and progression, probiotics are of great interest [142]. Probiotic supplementation can modify GM composition and intestinal barrier function, potentially modulating GBA pathways, immune cells, and inflammatory cytokines. Studies in MS patients and animal models have shown promising but inconclusive results, including slower disability progression, reduced depressive symptoms, and improvements in general health [143,144]. Further research is needed to explore different strains and their effects on GM composition, as they may depend on ongoing diets and therapies [145,146,147,148].
2.2. Dietary Supplementations
Apart from probiotics, dietary supplementation of several compounds proposed to increase anti-inflammatory and antioxidant activities have been reviewed by a recent Cochrane metanalysis including 30 randomized controlled trials (RCT) or controlled clinical trials (CCT) among participants with MS on MS-related outcomes, i.e., relapses, disability progression, and magnetic resonance imaging (MRI) measures [149]. After reviewing dietary programs including supplementation to increase PUFAs [comparing PUFAs vs. MUFA or PUFA Omega 6 vs. Omega 3] and other dietary supplements (e.g., antioxidants, acetyl L-carnitine, biotin, creatine, riboflavin), the metanalysis concluded that, at present, there is insufficient evidence to determine whether supplementation with antioxidants or other dietary interventions has any real impact, whether beneficial or harmful, on MS-related outcomes [149,150]. These data confirmed others’ conclusions that the body of present evidence is primarily focused around the isolation of individual nutrients, many of which demonstrate no clear effect on major outcomes of MS progression [151]. Of note, although some uncertainties can depend on the dosages used and/or the duration of the treatments (e.g., PUFA), supplementations with other compounds (e.g., vitamin D) may depend on patients’ pre-existing nutritional adequacy as opposed to a need for high-dose supplementation [151]. Recent data confirm that although there are no statistically significant correlations between clinical outcomes and vitamin D serum levels or supplementations, patients receiving vitamin D had fewer new T2-weighted lesions, especially when optimal or higher levels of vitamin D (>30 ng/mL) were maintained throughout the entire 4-month observation period [152]. All in all, stronger studies focused on food and nutritional supplementation are required to strengthen the evidence.
This entry is adapted from the peer-reviewed paper 10.3390/children10061022
This entry is offline, you can click here to edit this entry!
