Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cardiac & Cardiovascular Systems
Non-invasive imaging methods can assess coronary anatomy through coronary computed tomography angiography (CCTA) and/or inducible myocardial ischemia through functional stress testing (stress echocardiography, cardiac magnetic resonance imaging, single photon emission computed tomography—SPECT, or positron emission tomography—PET).
- chronic coronary syndrome
- echocardiography
- cardiac magnetic resonance
- coronary computed tomography angiography
- nuclear medicine
- ischemia
- CAD
1. A Multimodal Imaging Approach in Chronic Coronary Syndrome
Coronary artery disease (CAD) is a major cause of morbidity and mortality worldwide, and an accurate diagnostic assessment is pivotal for identifying patients that could potentially benefit from revascularization [1].
A multimodal non-invasive diagnostic approach for CAD detection includes anatomical (Coronary Computed Tomography Angiography, CCTA) and non-invasive functional imaging (stress echocardiography—SE, Cardiac Magnetic Resonance—CMR, nuclear imaging, stress CCTA, or CCTA derived Fractional Flow Reserve-FFR) [2,3].
While CCTA accurately depicts coronary anatomy, detects potential stenosis, and evaluates plaque features, other non-invasive functional imaging can demonstrate myocardial ischemia and the corresponding coronary territory. Integrating this complementary information is essential for the global risk assessment and the subsequential management of patients with suspected CAD [2].
The current European Society of Cardiology (ESC) guidelines recommend the use of either anatomical or non-invasive functional imaging as the initial test for diagnosing CAD after a global clinical risk assessment [4].
Which test to prescribe can be sometimes difficult to decide; typically CCTA is the preferred test in patients with a lower range of clinical likelihood of CAD, whereas the non-invasive functional tests for ischemia have better rule-in power and should be therefore preferred in those with higher clinical risk of coronary atherosclerosis [4].
2. The Role of Echocardiography
Functional tests designed to identify suspected CAD, with or without cardiac imaging, traditionally serve three important clinical purposes in the field of cardiology:
-
Diagnosing CAD
-
Guiding appropriate therapy (revascularization and/or medical intervention) in cases where CAD is confirmed
-
Assessing the long-term outcomes and stratifying the risk for patients with CAD.
Stress echocardiography is commonly utilized as a non-invasive functional test during the diagnostic evaluation of CAD. It possesses the following characteristics:
-
Cost-effectiveness and wide accessibility
-
Absence of ionizing radiation (environmentally friendly)
-
Ease of performance, potentially at the bedside
-
High diagnostic accuracy, particularly in terms of specificity for severe/obstructive CAD [1].
3. The Role of Cardiac Magnetic Resonance
Among noninvasive imaging modalities, CMR has been increasingly used in recent years due to its unique qualities in providing a complete assessment in patients with known or suspected CAD [30]. Indeed, CMR is able not only to evaluate the morphology, volume, and wall motion of the left ventricle (LV) but also allows precise tissue characterization. Furthermore, after gadolinium-based contrast medium (GBCM) injection, it enables the evaluation of stress-perfusion defects and the acquisition of late gadolinium enhancement (LGE) sequences for the detection of the extent of infarct scar [31,32,33].
In some cases, nuclear imaging may show false negative (balanced ischemia) or false positive results; in these circumstances, stress-CMR offers better sensibility and specificity in detecting functionally significant CAD [2].
In a few large randomized clinical trials, stress-CMR has been shown to be even superior in detecting ischemia compared to single photon emission computed tomography (SPECT) [34,35,36], and it resulted in a lower probability of unnecessary subsequent angiography [37,38]. The importance of stress-CMR is not only related to its high diagnostic accuracy but also to its ability to predict the patient’s prognosis.
In fact, numerous studies have demonstrated that pathological stress-CMR is associated with a higher risk of cardiac death and adverse events during long-term follow-up [39,40,41,42].
In patients with prior revascularization, a stress-CMR reduces the need for further diagnostic imaging techniques, subsequent coronary angiography, and revascularizations without impairing patients’ prognosis [30].
4. The Role of Nuclear Medicine (SPECT/PET)
The use of single photon emission computed tomography (SPECT) is currently an established approach in the initial evaluation of patients with suspected CAD thanks to wide availability, standardized protocols, and the extensive data established for diagnostic accuracy. Ischemia can be provoked by exercise or pharmacological stressors (dobutamine) that increase myocardial work and oxygen demand, as in other stress imaging protocols [2]. In case of left bundle branch block or ventricular paced rhythms, vasodilators (i.e., adenosine, regadenoson, or dipyridamole) should be preferred to identify heterogeneity in myocardial perfusion as well as in patients who are not able to achieve ≥85% of maximal age-predicted heart rate during exercise [59]. The mechanisms of action of the vasodilator substances and dobutamine are the same as already described in the CMR section.
Single-photon emission computed tomography implicates the intravenous administration of gamma-emitting radiotracers, which are accumulated by cardiomyocytes in proportion to myocardial blood flow. This uptake occurs during periods of rest as well as during physical or pharmacological stress. The radionuclide agent is typically injected at the peak of exercise or during maximum vasodilation. During stress, a decrease in regional tracer uptake indicates relative myocardial hypoperfusion, whereas reduced uptake both during stress and at rest suggests the presence of a myocardial scar [60]. Two radiopharmaceuticals labeled with technetium-99m (99mTc) (sestamibi and tetrofosmin) and thallium-201 (201Tl) chloride are currently commercially available [59,61].
The particular pharmacokinetic characteristic of 201Tl is the prolonged retention within the cardiomyocytes allowing the evaluation of the coronary reserve in a single administration immediately after the provocation test. On the contrary, the perfusion study should be performed in two sessions (stress and rest test, usually 24 h apart) using the technetium-based tracers, with more favorable dosimetry and improved quality of gated images thanks to their shorter half-life [59].
5. The Role of Coronary Computed Tomography Angiography
Coronary CT Angiography (CCTA) is the preferred imaging technique in symptomatic patients with a low-intermediate pre-test probability of CAD [4,69]. The current new-generation CT scanners enable high image quality with reduced contrast volume and radiation dosage, providing high diagnostic accuracy in the detection of CAD, even in the case of patients with high and/or irregular heart rates [20,70]. Integrating CCTA in the diagnostic algorithm of patients with stable chest pain was shown to be associated with a significant reduction in cardiovascular death and non-fatal myocardial infarction, due to proper diagnosis and tailoring of the treatment strategy [71,72].
Coronary CT Angiography allows risk stratification of patients with CAD based on the severity of coronary stenoses but also evaluation of the plaque characteristics (Figure 1). Importantly, baseline plaque burden is associated with the risk of major cardiovascular events independently of the presence of obstructive lesions [73,74,75] and predicts the progression to obstructive CAD [76]. High-risk plaque features (i.e., positive remodeling, low attenuated plaques, napkin-ring sign, spotty calcification) are strong predictors of future MI and focused the physician on secondary medical treatments [77,78,79].
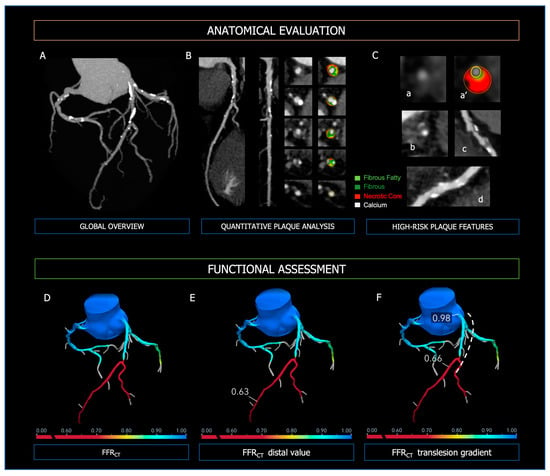
Figure 1. Anatomical evaluation and functional assessment of coronary plaques derived from CCTA. Panel (A)—3-vessel overview of the coronary tree for evaluation of calcium extent and distribution; Panel (B)—curved MPR, straight MPR, and cross-sections for quantitative plaque analysis; Panel (C)—high-risk plaque features; (a,a’): low attenuated plaque; (b): napkin-ring sign; (c): positive remodeling; (d): spotty calcifications. In the upper Panels, the figure legend refers to the colors used for quantitative plaque analysis; light green: fibrous fatty volume; dark green: fibrous volume; red: necrotic core volume; white: calcific volume. Panel (D): FFR-CT 3D model of the coronary tree, with distal FFR-CT (Panel (E)) and trans-lesion gradient (Panel (F), dashed line). At the bottom of Panels (D–F), the colorimetric scale of FFR-CT used in the 3D models is shown.
The specificity of CCTA in CAD is boosted with the integration of anatomical information with functional hemodynamic assessment (Figure 4), which includes (i) CT-derived fractional flow reserve (FFRCT) and (ii) CT perfusion (CTP) [80]. The use of FFRCT, which is based on computational fluid dynamics, showed the highest diagnostic performance for vessel-specific ischemia compared with SPECT and PET [81]. Moreover, in the case of FFRCT < 0.80, stable symptomatic patients diagnosed with CAD at CCTA have been shown to experience significantly lower cardiovascular death or myocardial infarction [82]. Thus, the diagnostic strategy based on CCTA integrated with FFRCT proves to be accurate and cost-effective, reducing the number of unnecessary invasive coronary angiography [28]. In the PERFECTION Trial, the addition of both FFRCT or stress-CTP to CCTA improved its diagnostic accuracy and positive predictive value in the evaluation of the functional relevance of CAD [83]. Compared with computational fluid dynamics (CFD) analytics, CTP has limited application in clinical practice and data regarding prognostic implications are lacking. However, the combined approach CCTA plus CTP is characterized by excellent specificity for the detection of hemodynamically significant CAD [84,85]. Moreover, it is comparable to invasive coronary angiography plus SPECT in predicting major cardiovascular events [86].
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics13122083
This entry is offline, you can click here to edit this entry!
