The glycocalyx generally covers almost all cellular surfaces, where it participates in mediating cell-surface interactions with the extracellular matrix as well as with intracellular signaling molecules. The endothelial glycocalyx that covers the luminal surface mediates the interactions of endothelial cells with materials flowing in the circulating blood, including blood cells. Cardiovascular diseases (CVD) remain a major cause of morbidity and mortality around the world. The cardiovascular risk factors start by causing endothelial cell dysfunction associated with destruction or irregular maintenance of the glycocalyx, which may culminate into a full-blown cardiovascular disease. The endothelial glycocalyx plays a crucial role in shielding the cell from excessive exposure and absorption of excessive salt, which can potentially cause damage to the endothelial cells and underlying tissues of the blood vessels.
1. Background
The blood vascular system consists of a network of vessels ranging from as large as the aorta, arteries, and veins to the smaller units including arterioles, venules, and capillaries [
1]. With the exception of the capillaries whose wall is made up of a single layer of endothelial cells, the other vessels have a wall with several tissue layers called tunics: tunica interna, tunica media, and tunica adventitia/externa [
2]. The innermost tissue layer in the wall of the blood vessels is the luminal surface layer, consisting of continuously arranged endothelial cells [
3]. The single layer of endothelial cells making up the capillaries is interrupted with some fenestrations or pores in some tissues such as in the gastrointestinal tract to enable the transportation of molecules across the capillary wall [
3,
4,
5]. The luminal surface of endothelial cells is lined with a meshwork consisting of glycoproteins, proteoglycans, and hyaluronic acid/hyaluronan (HA), forming a gel-like material known as the endothelial glycocalyx [
6,
7]. The main components of the endothelial glycocalyx therefore include cell surface heparan sulfate proteoglycans (HSPGs) with associated chondroitin sulfate (CS) polysaccharide chains in certain syndecans (SDCs) and hyaluronic acid/hyaluronan (HA) [
8]. The HA in the glycocalyx helps to reinforce its thickness and provides it with a gel-like appearance on the surface of the endothelial cells [
9]. The endothelial-associated HSPGs consist of syndecans (SDCs) and glypicans (GPCs) that are located on the cell membranes [
10] and perlecan secreted into the extracellular matrix with a pericellular localization near the basement membrane [
10,
11].
The glycocalyx plays an important protective role on the tissues that it covers, especially the epithelial and endothelial surfaces [
12]. For instance, the endothelial glycocalyx has been reported to act as a salt-buffer on the endothelial surfaces, preventing the rapid absorption of sodium chloride (NaCl) from plasma and, thus, protecting the endothelium and the underlying tissues from the damaging effects of direct exposure to excessive amounts of salt [
13]. An intact glycocalyx is also essential for the normal structure or function of endothelial cells, and endothelial dysfunction is mainly associated with old age, as well as pathological conditions including inflammatory conditions, atherosclerosis, hypertension, and heart failure [
14]. The extensive sulfation of the glycosaminoglycan (GAG) chains among the proteoglycans within the endothelial glycocalyx increases its negativity that allows it to bind plasma proteins such as albumin [
15]. The major components of the endothelial glycocalyx that project into the vascular lumen are also involved in flow-mediated “mechanosensation-mechanotranduction” that affects nitric oxide synthesis and vasodilation [
16].
Glycocalyx homeostasis is very important in a sense that there is constant biosynthesis and degradation of its components to maintain a balanced cell surface layer [
9]. Deviations from this balance either through excessive degradation or biosynthesis of the glycocalyx has been associated with various disease states [
19,
20]. The excessive degradation of the glycocalyx has been linked to disease conditions including cardiovascular diseases, hypertension, diabetes, and some cancers [
21]. On the other hand, increased biosynthesis of the glycocalyx components has been observed and associated with various types of cancers [
21,
22,
23,
24]. There are certain enzymes that are generally implicated in the degradation of components of the glycocalyx including: matrix metalloproteinases (MMPs), ADAM-17 (a disintegrin and metalloproteinase), and ‘sheddases’ such as secretases, heparanases, and hyaluronidases (HYAL 1to 3) [
25,
26,
27]. Circulating levels of the glycocalyx degradation enzymes and/or levels of these components of the glycocalyx such as syndecans or HA in plasma may be used to gauge the status of the endothelial glycocalyx in various disease states [
28]. Thus, prolonged cardio-pulmonary bipass in individuals undergoing cardiac surgery has been associated with increased glycocalyx degradation based on the increased levels of syndecan-1 in circulation [
29].
2. Major Components of the Glycocalyx in CVD Pathophysiology
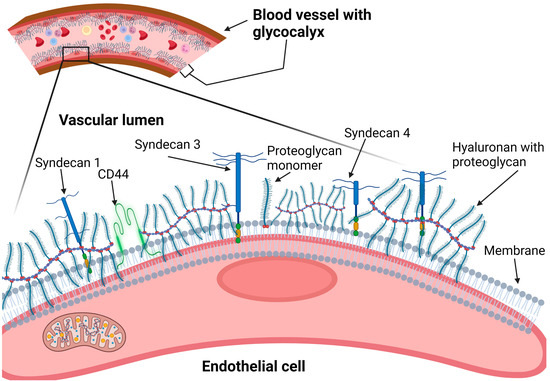
The components of the glycocalyx involved in CVD pathophysiology include membrane-bound heparan sulfate proteoglycans (such as syndecans and glypicans), CD44, and a membrane-associated polysaccharide called hyaluronic acid (or hyaluronan) (Figure 1).
Figure 1. Components of the vascular endothelial cell surface glycocalyx. CD-44: cluster of differentiation-44.
2.1. Heparan Sulfate Proteoglycans (Syndecans and Glypicans)
2.1.1. Syndecans
Syndecans belong to a family of single-pass transmembrane proteoglycans with three major domains: an ectodomain on the outside, a transmembrane domain, and a cytoplasmic domain on the inner side of the plasma membrane [
31]. The ectodomain is modified with conjugated glycosaminoglycan (GAG) chains in form of either heparan sulfate (HS) or chondroitin sulfate (CS) chains or both, which enable syndecans to act as cell surface co-receptors [
32]. Heparan sulfate chains are the major GAG in syndencans, but CS chains are also found on syndecans 1 and 3 [
33]. The GAG chains are conjugated to the ectodomain of a core protein, expressed by any of the four mammalian genes that encode for syndecans 1 to 4 (SDCs 1 to 4) [
34]. The GAG-attachment site on the ectodomain is at both ends in the case of SDC-1 and SDC-3, but it is near the terminal end for SDC-2 and SDC-4 [
35]. The presence of cleavage sites on the ectodomains of syndecans renders them liable to being ‘slashed’ from the plasma membrane by ‘sheddases’ (proteolytic enzymes such as matrix metalloproteinases) and released into plasma (becoming ‘solubilized’ as soluble syndecans), which may be potentially utilized as biomarkers for various diseases [
35,
36,
37]. The HS and CS chains are modified with unique sulfation patterns along their lengths, making them highly negatively charged and enabling them to bind with a wide range of positively charged particles including positively charged peptides (e.g., growth factors) and electrolytes including sodium ions.
2.1.2. Glypicans
Glypicans are membrane-bound or cell surface heparan sulfate proteoglycans with one or two heparan sulfate chains and a glycosylphosphatidylinositol anchor that attaches the entire molecule to the plasma membrane [
50]. This group of molecules consists of six members, from glypican-1 to -6, which are expressed predominantly during embryonic development [
51]. They are involved in facilitating Wnt, hedgehog, fibroblast growth factor, and bone-morphogenic proteins/peptide signaling [
51,
52,
53]. Their GPI anchor is cleaved by the expression of an enzyme known as Notum that releases not only glypicans but also other GPI-anchored proteins from the cell surface [
54]. Glypicans are a major component of the glycocalyx alongside syndecans, which undergo significant remodeling by sheer stress on the endothelial surface during atherosclerosis [
55].
2.2. Hyaluronan
Hyaluronan is a long polysaccharide of alternating glucuronic acid (GlcA) and N-acetylglucosamine (GlcNAc) sugar residues, which are un-sulfated but result in a highly negatively charged molecule [
57]. It is pericellularly synthesized by a family of three pericellular enzymes known as hyaluronan synthases: from HAS-1 to -3 [
58,
59]. It is then degraded by a family of six hyaluronidase (HYALs) members, of which HYAL-1 and HYAL-2 are the most potent enzymes [
60,
61]. HYAL-2 is believed to have a role in promoting pulmonary vascular remolding and pulmonary hypertension [
61]. The deficiency of HYAL-3 increases collagen deposition, promoting post-myocardial infarction fibrosis [
61]. Hyaluronan is most known as an extracellular matrix molecule, but, due to its close association with various cell surface structures including its cognate receptor CD44, integrins, and proteoglycans, it contributes to the surface gel-like glycocalyx of the synthesizing cell [
62]. The hyaluronan receptor-CD44 can also be cleaved from the cell surface by proteases such as ADAM-10, ADAM-17, and MMP-14 [
63,
64]. A delicate balance is maintained normally between hyaluronan bio-synthesis and degradation depending on the activity of HASs and HYL enzymes, which varies in different physiological and pathological conditions [
62]. The hyaluronan synthesis and degradation processes are indeed crucial during cardiovascular development or angiogenesis [
65,
66]. Native hyaluronan is believed to inhibit angiogenesis, whereas oligosaccharides formed following hyaluronan degradation seem to promote angiogenesis by increasing endothelial cell proliferation and migration [
67,
68]. The interactions of hyaluronan with reactive oxygen or nitrogen species (ROS/RNS) and their consequences on tissue homeostasis are well summarized by Berdiaki et al., whereby the innate high molecular weight hyaluronan is anti-angiogenic, anti-inflammatory, and anti-oncogenic [
69]. However, following degradation by the ROS/RNS, the low molecular weight oligosaccharides produced become pro-angiogenic, pro-inflammatory, and oncogenic [
69]. Changes in hyaluronan synthesis and degradation have mainly been associated with cancer and inflammatory conditions [
70,
71,
72,
73].
3. Glycocalyx and Salt Interactions
Since the endothelial glycocalyx covers the luminal surface of the cells, where it forms a gel-like structure, it is believed to protect the endothelial cells from direct exposure to excessive NaCl salt (above 160 mEq/L) dissolved in plasma [
86]. The normal sodium levels in plasma are kept within a narrow range of 135–145 mEq/L by a combination of ‘thirst’/water intake and hormonal (aldosterone-anti-diuretic/vasopressin) systems [
87,
88]. The GAG chains (including heparan sulfate, chondroitin sulfate, and hyaluronan) are major components of the glycocalyx and are highly negatively charged, making them attractive to the positively charged sodium ions flowing in circulation [
89],
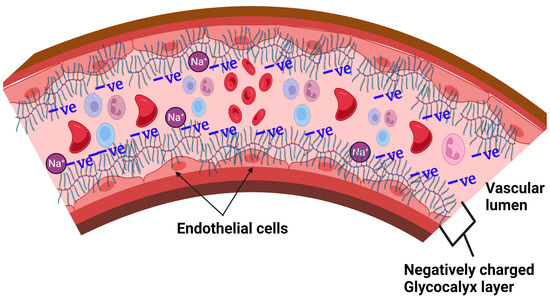
Figure 2. Thus, the glycocalyx is able to play a positive role in the sodium buffering by transiently binding sodium on the luminal side of the blood vessels [
90]. The glycocalyx, therefore, is a major player in buffering the intravascular sodium and stores a great amount sodium creating a hypertonic environment [
91,
92].
Figure 2. Vascular endothelial glycocalyx buffering sodium.
3.1. Proposed Glycocalyx-Salt Interaction Mechanisms Contributing to Hypertension and Cardiovascular Disease
The mechanism underlying the rapid degradation of the endothelial glycocalyx is that excess sodium diminishes the buffering capacity of the glycocalyx leading to increased sodium reaching endothelial cells as well as reducing the repelling effect between the vascular and erythrocyte glycocalyces; this leads to corrosion of both the erythrocyte and endothelial glycocalyces, which result in endothelial activation and dysfunction [
93,
96,
97]. Damage to the vascular glycocalyx also leads to extravasation of the excess sodium ions into the interstitial glycosaminoglycan networks where sodium disrupts the function of the glycosaminoglycans and also activates immune cells [
91,
98,
99]. The augmented interaction between the erythrocytes and endothelial glycocalyces increases the thrombotic events [
100] and the interaction between the endothelial cell and innate cells in the lumen via the adhesion molecules [
101]. The entry of excess sodium through the epithelial sodium channel (ENaC) on the endothelial cells and innate immune cells (such as dendritic cells [
102,
103,
104,
105] and macrophages) activates nicotinamide adenine dinucleotide phosphate (NADPH) oxidase resulting in the generation of super oxides, peroxynitrite, and other reactive oxygen species (ROS) [
106].
The endothelial cells with excessively degraded glycocalyx from excess sodium overload are unable to produce sufficient nitric oxide due to the reduced activation of endothelial nitric oxide synthase [
117,
118]. Recent evidence has shown that the endothelial glycocalyx plays a role in initiating the signal transduction pathways that contribute to NO production. Specifically, Bartosch et al. demonstrated that the proteoglycan glypican-1, not syndecan-1, plays a dominant role in propagating extracellular forces into the endothelial cells to activate signal transduction for the production of NO [
119].
3.2. Possible Strategies for Reducing the Damaging Effects of NaCl-Salt Overload on Vascular Endothelium
High dietary salt intake remains a big challenge as many people in various populations around the world are still unable to stop consuming high amounts of salt due to the diverse sources of dietary salt available in common foods [126,127,128]. It is therefore understandable that efforts are being made to find alternative ways of overcoming the deleterious effects of high salt overload on human health, other than simply advising people to reduce salt intake. For example, a recent clinical trial conducted among black women aged between 20 and 60 years in the USA provided evidence showing that ‘hot yoga’ can reduce the harmful effects of salt overload on endothelial function [129]. The exact mechanism is unknown. Similarly, regular aerobic exercise has also been reported to reduce endothelin-1-mediated vasoconstriction and endothelial dysfunction in postmenopausal women, as well as in obese or overweight adults [130,131]. Replacement or substitution of NaCl salt with other forms of salt with similar ‘saltness’ taste, such as potassium chloride (KCl) and monosodium glutamate (MSG), have also been piloted by the Department of Food Science at Cornell University (New York) and been found to have relatively high acceptability among the study subjects, although with a caveat of not disclosing the specific names of the salt substitute [132].
4. Current Diagnostic Tools to Determine Glycocalyx and Endothelial Health Status
Since the glycocalyx consists of both protein and carbohydrate components, its breakdown products include monomers or shorter/smaller molecules of each of the two large macromolecules, as well as shed syndecans and glypicans [
27,
148]. These include small peptides or amino acids and the breakdown products of proteins: glypicans, syndecan-1, shorter disaccharides, or individual GlcA and GlcNAc—these are sugar residues, which are the major breakdown products of the polysaccharide component of the glycocalyx [
148]. The much longer HA polysaccharides are usually reduced to shorter sugar chains that are released into various body fluids including saliva, cerebrospinal fluid (CSF), urine, and blood plasma and can easily be isolated from such body fluids [
149,
150]. The smaller peptides or amino acids can be re-used in the synthesis of new proteins by body cells [
151]. Most of the breakdown products of the polysaccharide component of the glycocalyx end up being deposited in body tissues and body fluids from which they can be measured or determined to assess the level of glycocalyx degradation as biomarkers of health or disease [
148,
150].
5. Conclusions
Endothelial glycocalyx is important in protecting endothelial cells from direct exposure to excessive amounts of salt and helps in maintaining normal endothelial function, which is necessary in the prevention of cardiovascular diseases. The degradation of the glycocalyx is increased in certain cardiovascular diseases due to enhanced sheer force of the rapid blood flow in hypertension, inflammatory changes, and oxidative stress in atherosclerosis and, alternatively, because of the increased expression of degradative enzymes. Excessive salt due to salt overload may also lead to rapid degradation of the endothelial glycocalyx, resulting in an endothelial dysfunction and consequent cardiovascular disease. This makes dietary modification, particularly reducing sodium-salt intake or using substitutes for dietary salt, a key strategy for preserving glycocalyx integrity. The increased presence of breakdown components of the glycocalyx, such as syndecans and hyaluronan in the plasma or urine of cardiovascular disease patients can be measured and utilized as a potential prognostic biomarker for specific cardiovascular disorders.
This entry is adapted from the peer-reviewed paper 10.3390/nu15132873