Human skin pigmentation and melanin synthesis are incredibly variable, and are impacted by genetics, UV exposure, and some drugs. Patients’ physical appearance, psychological health, and social functioning are all impacted by a sizable number of skin conditions that cause pigmentary abnormalities. Hyperpigmentation, where pigment appears to overflow, and hypopigmentation, where pigment is reduced, are the two major classifications of skin pigmentation. Albinism, melasma, vitiligo, Addison’s disease, and post-inflammatory hyperpigmentation, which can be brought on by eczema, acne vulgaris, and drug interactions, are the most common skin pigmentation disorders in clinical practice. Anti-inflammatory medications, antioxidants, and medications that inhibit tyrosinase, which prevents the production of melanin, are all possible treatments for pigmentation problems. Skin pigmentation can be treated orally and topically with medications, herbal remedies, and cosmetic products, but a doctor should always be consulted before beginning any new medicine or treatment plan.
- skin pigmentation
- melanin
- tyrosinase inhibitors
- hypopigmentation
1. Introduction

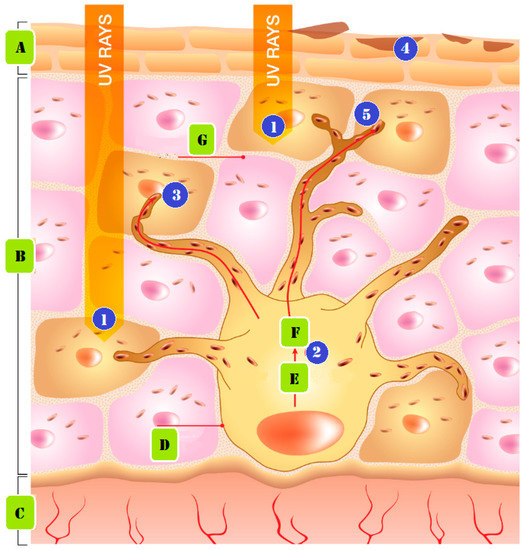
2. Causes of Skin Pigmentation
2.1. Genetics
2.2. Sun Exposure
2.3. Medications
3. Types of Pigmentation Disorders
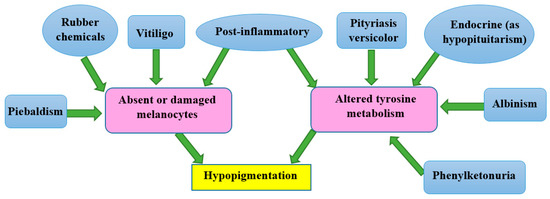
3.1. Causes of Hypopigmentation
3.2. Causes of Hyperpigmentation
4. Drugs for Treatment of Skin Pigmentation
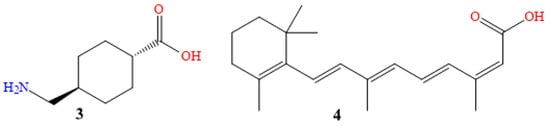
4.1. Oral Medications
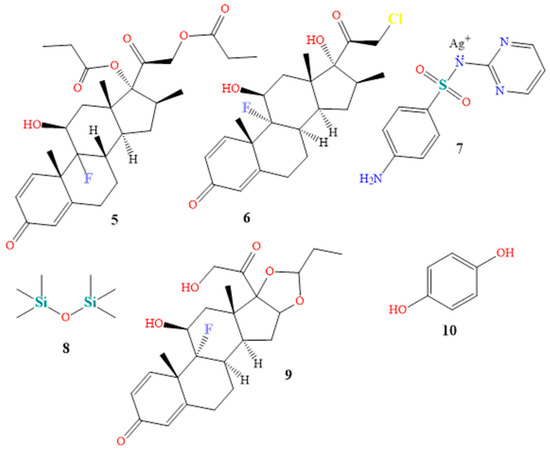
4.2. Topical Creams

5. Natural Hyperpigmentation Treatment
6. Modern Skin Pigmentation Treatments and Promising New Technologies
This entry is adapted from the peer-reviewed paper 10.3390/molecules28124839
References
- Del Bino, S.; Duval, C.; Bernerd, F. Clinical and biological characterization of skin pigmentation diversity and its consequences on UV impact. Int. J. Mol. Sci. 2018, 19, 2668.
- Martin, A.R.; Lin, M.; Granka, J.M.; Myrick, J.W.; Liu, X.; Sockell, A.; Atkinson, E.G.; Werely, C.J.; Möller, M.; Sandhu, M.S.; et al. An unexpectedly complex architecture for skin pigmentation in Africans. Cell 2017, 171, 1340–1353.
- Nasti, T.H.; Timares, L. MC 1R, Eumelanin and Pheomelanin: Their role in determining the susceptibility to skin cancer. Photochem. Photobiol. 2015, 91, 188–200.
- Solano, F. Photoprotection and skin pigmentation: Melanin-related molecules and some other new agents obtained from natural sources. Molecules 2020, 25, 1537.
- Polidori, C.; Jorge, A.; Ornosa, C. Eumelanin and pheomelanin are predominant pigments in bumblebee (Apidae: Bombus) pubescence. PeerJ 2017, 5, e3300–e3321.
- Hu, S.; Zhai, P.; Chen, Y.; Zhao, B.; Yang, N.; Wang, M.; Xiao, Y.; Bao, G.; Wu, X. Morphological characterization and gene expression patterns for melanin pigmentation in Rex rabbit. Biochem. Genet. 2019, 57, 734–744.
- Baek, S.H.; Lee, S.H. Sesamol decreases melanin biosynthesis in melanocyte cells and zebrafish: Possible involvement of MITF via the intracellular cAMP and p38/JNK signalling pathways. Exp. Dermatol. 2015, 24, 761–766.
- Madelaine, R.; Ngo, K.J.; Skariah, G.; Mourrain, P. Genetic deciphering of the antagonistic activities of the melanin-concentrating hormone and melanocortin pathways in skin pigmentation. PLoS Genet. 2020, 16, e1009244-65.
- Ozdeslik, R.N.; Olinski, L.E.; Trieu, M.M.; Oprian, D.D.; Oancea, E. Human nonvisual opsin 3 regulates pigmentation of epidermal melanocytes through functional interaction with melanocortin 1 receptor. Proc. Natl. Acad. Sci. USA 2019, 116, 11508–11517.
- Wolf Horrell, E.M.; Boulanger, M.C.; D’Orazio, J.A. Melanocortin 1 receptor: Structure, function, and regulation. Front. Genet. 2016, 7, 95–111.
- Suherlan, S.; Fakih, T.M.; Effendi, D.H. Uji In-Silico Aktivitas Melanogenesis Senyawa Ternatin Bunga Kembang Telang (Clitoria ternatea) terhadap Reseptor Tirosinase. Pros. Farm. 2021, 7, 849–856.
- Jablonski, N.G. The evolution of human skin pigmentation involved the interactions of genetic, environmental, and cultural variables. Pigment Cell Melanoma Res. 2021, 34, 707–729.
- Ainger, S.A.; Jagirdar, K.; Lee, K.J.; Soyer, H.P.; Sturm, R.A. Skin pigmentation genetics for the clinic. Dermatology 2017, 233, 1–15.
- Feng, Y.; McQuillan, M.A.; Tishkoff, S.A. Evolutionary genetics of skin pigmentation in African populations. Human Mol. Genet. 2021, 30, 88–97.
- Kita, R.; Fraser, H.B. Local adaptation of sun-exposure-dependent gene expression regulation in human skin. PLoS Genet. 2016, 12, e1006382.
- Armenta, A.M.; Henkel, E.D.; Ahmed, A.M. Pigmentation disorders in the elderly. Drugs Aging 2019, 36, 235–245.
- Adigun, C.G. Adverse drug reactions of the lower extremities. Clin. Podiatr. Med. Surg. 2016, 33, 397–408.
- Nicolaidou, E.; Katsambas, A.D. Pigmentation disorders: Hyperpigmentation and hypopigmentation. Clin. Dermatol. 2014, 32, 66–72.
- Böhm, M. Disorders of Melanin Pigmentation. In Braun-Falco’s Dermatology; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1–35.
- Ma, E.Z.; Zhou, A.E.; Hoegler, K.M.; Khachemoune, A. Oculocutaneous albinism: Epidemiology, genetics, skin manifestation, and psychosocial issues. Arch. Dermatol. Res. 2023, 315, 107–116.
- Federico, J.R.; Krishnamurthy, K. Albinism. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Lee, D.Y.; Kim, C.R.; Lee, J.H. Trichrome vitiligo in segmental type. Photodermatol. Photoimmunol. Photomed. 2011, 27, 111–112.
- Hill, J.P.; Batchelor, J.M. An approach to hypopigmentation. BMJ 2017, 356, 356–362.
- Kallini, J.R.; Riaz, F.; Khachemoune, A. Tinea versicolor in dark-skinned individuals. Int. J. Dermatol. 2014, 53, 137–141.
- Miazek, N.; Michalek, I.; Pawlowska-Kisiel, M.; Olszewska, M.; Rudnicka, L. Pityriasis Alba—Common Disease, Enigmatic Entity: Up-to-Date Review of the Literature. Pediatr. Dermatol. 2015, 32, 786–791.
- Jing, J.; Man, X.Y. Vitiligo-like depigmentation in a patient treated with PD-1 antibody. BMJ 2021, 374, n1982.
- McMichael, L. Skin camouflage. BMJ 2012, 344, d7921.
- Silpa-Archa, N.; Kohli, I.; Chaowattanapanit, S.; Lim, H.W.; Hamzavi, I. Postinflammatory hyperpigmentation: A comprehensive overview: Epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. J. Am. Acad. Dermatol. 2017, 77, 591–605.
- Sheth, P.B.; Shah, H.A.; Dave, J.N. Periorbital hyperpigmentation: A study of its prevalence, common causative factors and its association with personal habits and other disorders. Indian J. Dermatol. 2014, 59, 151–157.
- Choi, W.; Yin, L.; Smuda, C.; Batzer, J.; Hearing, V.J.; Kolbe, L. Molecular and histological characterization of age spots. Exp. Dermatol. 2017, 26, 242–248.
- Baxter, L.L.; Pavan, W.J. The etiology and molecular genetics of human pigmentation disorders. Wiley Interdiscip. Rev. Dev. Biol. 2013, 2, 379–392.
- Yadalla, H.K.K.; Aradhya, S. Post acne hyperpigmentation: A brief review. Our Dermatol. Online 2011, 2, 230–231.
- Plensdorf, S.; Livieratos, M.; Dada, N. Pigmentation disorders: Diagnosis and management. Am. Fam. Physician 2017, 96, 797–804.
- Woolery-Lloyd, H.; Kammer, J.N. Treatment of Hyperpigmentation. In Seminars in Cutaneous Medicine and Surgery; WB Saunders: Philadelphia, PA, USA, 2011; Volume 30, pp. 171–175.
- Bala, H.R.; Lee, S.; Wong, C.; Pandya, A.G.; Rodrigues, M. Oral tranexamic acid for the treatment of melasma: A review. Dermatol. Surg. 2018, 44, 814–825.
- Ali, A.A.; Al-Obaidi, Z.M.J.; Raauf, A.M.; Mahmood, H.S. A Comparative, Randomized, Double-Blinded, and Vehicle-Controlled Study for the Reduction in Facial Pigmentation after Treatment with both Tranexamic Acid and Tranexamic Acid Ethyl Ester. Syst. Rev. Pharm. 2020, 11, 563–567.
- Kaur, A.; Bhalla, M.; Sarkar, R. Tranexamic acid in melasma: A review. Pigment Int. 2020, 7, 12–25.
- Maeda, K. Mechanism of Action of Topical Tranexamic Acid in the Treatment of Melasma and Sun-Induced Skin Hyperpigmentation. Cosmetics 2022, 9, 108.
- McKesey, J.; Tovar-Garza, A.; Pandya, A.G. Melasma treatment: An evidence-based review. Am. J. Clin. Dermatol. 2020, 21, 173–225.
- Grimes, P.E.; Ijaz, S.; Nashawati, R.; Kwak, D. New oral and topical approaches for the treatment of melasma. Int. J. Women’s Dermatol. 2019, 5, 30–36.
- Artzi, O.; Horovitz, T.; Bar-Ilan, E.; Shehadeh, W.; Koren, A.; Zusmanovitch, L.; Mehrabi, J.; Salameh, F.; Nelkenbaum, G.I.; Zur, E.; et al. The pathogenesis of melasma and implications for treatment. J. Cosmet. Dermatol. 2021, 20, 3432–3445.
- Taraz, M.; Niknam, S.; Ehsani, A.H. Tranexamic acid in treatment of melasma: A comprehensive review of clinical studies. Dermatol. Ther. 2017, 30, e12465.
- Tse, T.W.; Hui, E. Tranexamic acid: An important adjuvant in the treatment of melasma. J. Cosmet. Dermatol. 2013, 12, 57–66.
- Sharma, R.; Mahajan, V.K.; Mehta, K.S.; Chauhan, P.S.; Rawat, R.; Shiny, T.N. Therapeutic efficacy and safety of oral tranexamic acid and that of tranexamic acid local infiltration with microinjections in patients with melasma: A comparative study. Clin. Exp. Dermatol. 2017, 42, 728–734.
- Kim, S.J.; Park, J.Y.; Shibata, T.; Fujiwara, R.; Kang, H.Y. Efficacy and possible mechanisms of topical tranexamic acid in melasma. Clin. Exp. Dermatol. 2016, 41, 480–485.
- Sofen, B.; Prado, G.; Emer, J. Melasma and post inflammatory hyperpigmentation: Management update and expert opinion. Skin. Ther. Lett. 2016, 21, 1–7.
- Demir, B.; Çiçek, D.; Bilik, L.; Aydoğdu, E.G.; Artaş, H.; Demirpolat, N.; Ergin, C. Oral isotretinoin induced pigmentation disorder: A case report. Firat Tip Derg 2017, 22, 143–145.
- Mysore, V.; Mahadevappa, O.H.; Barua, S.; Majid, I.; Viswanath, V.; Bhat, R.M.; Talwar, S.; Thurakkal, S.; Aurangabadkar, S.J.; Chatterjee, M.; et al. Standard guidelines of care: Performing procedures in patients on or recently administered with isotretinoin. J. Cutan. Aesthetic Surg. 2017, 10, 186–194.
- Bagatin, E.; Costa, C.S. The use of isotretinoin for acne–an update on optimal dosing, surveillance, and adverse effects. Expert Rev. Clin. Pharmacol. 2020, 13, 885–897.
- Fallah, H.; Rademaker, M. Isotretinoin in the management of acne vulgaris: Practical prescribing. Int. J. Dermatol. 2021, 60, 451–460.
- Villani, A.; Nastro, F.; Di Vico, F.; Fabbrocini, G.; Annunziata, M.C.; Genco, L. Oral isotretinoin for acne: A complete overview. Expert Opin. Drug Saf. 2022, 21, 1027–1037.
- Spring, L.K.; Krakowski, A.C.; Alam, M.; Bhatia, A.; Brauer, J.; Cohen, J.; Rosso, J.Q.; Diaz, L.; Dover, J.; Eichenfield, L.F.; et al. Isotretinoin and timing of procedural interventions: A systematic review with consensus recommendations. JAMA Dermatol. 2017, 153, 802–809.
- Chu, S.; Michelle, L.; Ekelem, C.; Sung, C.T.; Rojek, N.; Mesinkovska, N.A. Oral isotretinoin for the treatment of dermatologic conditions other than acne: A systematic review and discussion of future directions. Arch. Dermatol. Res. 2021, 313, 391–430.
- Shao, X.; Chen, Y.; Zhang, L.; Zhang, Y.; Ariyawati, A.; Chen, T.; Chen, J.; Liu, L.; Pu, Y.; Li, Y.; et al. Effect of 30% supramolecular salicylic acid peel on skin microbiota and inflammation in patients with moderate-to-severe acne vulgaris. Dermatol. Ther. 2023, 13, 155–168.
- Dréno, B.; Araviiskaia, E.; Kerob, D.; Andriessen, A.; Anfilova, M.; Arenbergerova, M.; Barrios, L.O.; Mokos, Z.B.; Haedersdal, M.; Hofmann, M.A. Nonprescription acne vulgaris treatments: Their role in our treatment armamentarium—An international panel discussion. J. Cosmet. Dermatol. 2020, 19, 2201–2211.
- Rachmin, I.; Ostrowski, S.M.; Weng, Q.Y.; Fisher, D.E. Topical treatment strategies to manipulate human skin pigmentation. Adv. Drug Deliv. Rev. 2020, 153, 65–71.
- Bose, S.K.; Ortonne, J.P. Pigmentation: Dyschromia. In Textbook of Cosmetic Dermatology; Martin-Dunitz Ltd.: London, UK, 1998; pp. 391–415.
- Yasir, M.; Goyal, A.; Sonthalia, S. Corticosteroid adverse effects. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Yélamos, O.; Alejo, B.; Ertekin SSVilla-Crespo, L.; Zamora-Barquero, S.; Martinez, N.; Domínguez, M.; Iglesias, P.; Herrero, A.; Malvehy, J.; Puig, S. Non-invasive clinical and microscopic evaluation of the response to treatment with clobetasol cream vs. calcipotriol/betamethasone dipropionate foam in mild to moderate plaque psoriasis: An investigator-initiated, phase IV, unicentric, open, randomized clinical trial. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 143–149.
- Cho, J.H.; Bhutani, S.; Kim, C.H.; Irwin, M.R. Anti-inflammatory effects of melatonin: A systematic review and meta-analysis of clinical trials. Brain Behav. Immun. 2021, 93, 245–253.
- Karekar, S.R.; Marathe, P.A.; Nagarajan, V.B.; Khopkar, U.S.; Chikhalkar, S.B.; Desai, P.K.; Dongre, M.S. Use of topical steroids in dermatology: A questionnaire based study. Indian Dermatol. Online J. 2020, 11, 725–730.
- Chadderdon, C.; Gaston, R.G.; Loeffler, B.J.; Lewis, D. Betamethasone Versus Ketorolac Injection for the Treatment of De Quervain’s Tenosynovitis: A Double-Blind Randomized Clinical Trial: Level 1 Evidence. J. Hand Surg. 2017, 42, S45–S46.
- Patel, H.K.; Barot, B.S.; Parejiya, P.B.; Shelat, P.K.; Shukla, A. Topical delivery of clobetasol propionate loaded microemulsion based gel for effective treatment of vitiligo: Ex vivo permeation and skin irritation studies. Colloids Surf. B Biointerfaces 2013, 102, 86–94.
- Khaitan, B.K.; Sindhuja, T. Autoimmunity in vitiligo: Therapeutic implications and opportunities. Autoimmun. Rev. 2022, 21, 102932.
- Eleftheriadou, V.; Atkar, R.; Batchelor, J.; McDonald, B.; Novakovic, L.; Patel, J.V.; Ravenscroft, J.; Rush, E.; Shah, D.; Shah, R.; et al. British Association of Dermatologists’ Clinical Standards Unit. British Association of Dermatologists guidelines for the management of people with vitiligo 2021. Br. J. Dermatol. 2022, 186, 18–29.
- Habet, K.A.; Kolli, S.S.; Pona, A.; Feldman, S.R. A review of topical corticosteroid sprays for the treatment of inflammatory dermatoses. Dermatol. Online J. 2019, 25, 3–12.
- Gajinov, Z. Corticosteroid topical therapy range: Fluocinolone-acetonide gel. Galen. Med. J. 2022, 1, 17–22.
- Medici, S.; Peana, M.; Nurchi, V.M.; Zoroddu, M.A. Medical uses of silver: History, myths, and scientific evidence. J. Med. Chem. 2019, 62, 5923–5943.
- Bandyopadhyay, D. Topical antibacterials in dermatology. Indian J. Dermatol. 2021, 66, 117–125.
- Adhya, A.; Bain, J.; Ray, O.; Hazra, A.; Adhikari, S.; Dutta, G.; Ray, S.; Majumdar, B.K. Healing of burn wounds by topical treatment: A randomized controlled comparison between silver sulfadiazine and nano-crystalline silver. J. Basic Clin. Pharm. 2014, 6, 29–34.
- Nethi, S.K.; Das, S.; Patra, C.R.; Mukherjee, S. Recent advances in inorganic nanomaterials for wound-healing applications. Biomater. Sci. 2019, 7, 2652–2674.
- Srivastava, S.; Patil, A.; Prakash, C.; Kumari, H. Comparison of intralesional triamcinolone acetonide, 5-fluorouracil, and their combination in treatment of keloids. World J. Plast. Surg. 2018, 7, 212–219.
- Khan, H.A.; Sahibzada, M.N.; Paracha, M.M. Comparison of the efficacy of intralesional bleomycin versus intralesional triamcinolone acetonide in the treatment of keloids. Dermatol. Ther. 2019, 32, e13036-40.
- Raman, P.; Pitty, R.; Krithika, C.L.; Anand, S.N.; Subramani, G.P. Topical curcumin and triamcinolone acetonide in recurrent minor aphthous ulcers: A pilot trial. J. Contemp. Dent. Pract. 2020, 21, 884–890.
- Kwiatkowska, D.; Wicka, M.; Bulska, E.; Kaliszewski, P. Investigation of the Excretion of Triamcinolone Acetonide and Its Metabolite. Separations 2023, 10, 164.
- Mangion, S.E.; Mackenzie, L.; Roberts, M.S.; Holmes, A.M. Seborrheic dermatitis: Topical therapeutics and formulation design. Eur. J. Pharm. Biopharm. 2023, 185, 148–164.
- Pinto, L.M.; Chiricozzi, A.; Calabrese, L.; Mannino, M.; Peris, K. Novel Therapeutic Strategies in the Topical Treatment of Atopic Dermatitis. Pharmaceutics 2022, 14, 2767.
- Sandhu, S.; Klein, B.A.; Al-Hadlaq, M.; Chirravur, P.; Bajonaid, A.; Xu, Y.; Intini, R.; Hussein, M.; Vacharotayangul, P.; Sroussi, H.; et al. Oral lichen planus: Comparative efficacy and treatment costs—A systematic review. BMC Oral Health 2022, 22, 161.
- Pakravan, F.; Ghalayani, P.; Emami, H.; Isfahani, M.N.; Noorshargh, P. A novel formulation for radiotherapy-induced oral mucositis: Triamcinolone acetonide mucoadhesive film. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2019, 24, 63.
- Mangold, A.R.; Pittelkow, M.R. Lichen planus. Clin. Basic Immunodermatology 2017, 551–576.
- Ahmad Nasrollahi, S.; Sabet Nematzadeh, M.; Samadi, A.; Ayatollahi, A.; Yadangi, S.; Abels, C.; Firooz, A. Evaluation of the safety and efficacy of a triple combination cream (hydroquinone, tretinoin, and fluocinolone) for treatment of melasma in Middle Eastern skin. Clin. Cosmet. Investig. Dermatol. 2019, 12, 437–444.
- Dreher, F.; Draelos, Z.D.; Gold, M.H.; Goldman, M.P.; Fabi, S.G.; Puissegur Lupo, M.L. Efficacy of hydroquinone-free skin-lightening cream for photoaging. J. Cosmet. Dermatol. 2013, 12, 12–17.
- Banihashemi, M.; Zabolinejad, N.; Jaafari, M.R.; Salehi, M.; Jabari, A. Comparison of therapeutic effects of liposomal tranexamic acid and conventional hydroquinone on melasma. J. Cosmet. Dermatol. 2015, 14, 174–177.
- Pradhan, M.; Singh, D.; Murthy, S.N.; Singh, M.R. Design, characterization and skin permeating potential of Fluocinolone acetonide loaded nanostructured lipid carriers for topical treatment of psoriasis. Steroids 2015, 101, 56–63.
- Treesirichod, A.; Chaithirayanon, S.; Chaikul, T.; Chansakulporn, S. The randomized trials of 10% urea cream and 0.025% tretinoin cream in the treatment of acanthosis nigricans. J. Dermatol. Treat. 2021, 32, 837–842.
- Bagatin, E.; Gonçalves, H.D.S.; Sato, M.; Almeida, L.M.C.; Miot, H.A. Comparable efficacy of adapalene 0.3% gel and tretinoin 0.05% cream as treatment for cutaneous photoaging. Eur. J. Dermatol. 2018, 28, 343–350.
- Nautiyal, A.; Wairkar, S. Management of hyperpigmentation: Current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021, 34, 1000–1014.
- Ferraris, C.; Rimicci, C.; Garelli, S.; Ugazio, E.; Battaglia, L. Nanosystems in cosmetic products: A brief overview of functional, market, regulatory and safety concerns. Pharmaceutics 2021, 13, 1408.
- Usatine, R.; Tinitigan, M. Diagnosis and treatment of lichen planus. Am. Fam. Physician 2011, 84, 53–60.
- Korabiusz, K.; Wawryków, A.; Fabian-Danielewska, A.; Stecko, M.; Wilczyńska, A.; Janik-Fuks, I.; Martyna, M.; Harasimowicz, J. Laser removal of tattoo-A case report. J. Educ. Health Sport 2019, 9, 415–419.
- Doucette, K.; Forster, S.; Marcus, A. Study to Assess Visual Elimination of a Novel Otic Gel (Florfenicol, Terbinafine, Betamethasone Acetate) in Comparison to an Otic Solution (Florfenicol, Terbinafine, Mometasone Furoate) and an Otic Suspension (Gentamicin Sulfate, Clotrimazole, Mometasone Furoate Monohydrate) in Dogs Immediately after Application to the Ear Canal. In BSAVA Congress Proceedings 2018; BSAVA Library: Gloucester, UK, 2018; p. 489.
- Grammatikova, N.É. Comparative study of the antimicrobial activity of combined topical medicinal formulations of betamethasone, gentamicin, and clotrimazole in vitro. Pharm. Chem. J. 2020, 53, 971–975.
- Cole, L.K.; Rajala-Schultz, P.J.; Lorch, G. Conductive hearing loss in four dogs associated with the use of ointment-based otic medications. Vet. Dermatol. 2018, 29, 341-e120.
- Hikmatovich, I.N. Evaluation of the Efficacy of External Therapy in Sick Children with Alergodermatosis. Web Semant. Univers. J. Innov. Educ. 2023, 2, 50–54.
- Harris, J.E.; Rashighi, M.; Nguyen, N.; Jabbari, A.; Ulerio, G.; Clynes, R.; Christiano, A.M.; Mackay-Wiggan, J. Rapid skin repigmentation on oral ruxolitinib in a patient with coexistent vitiligo and alopecia areata (AA). J. Am. Acad. Dermatol. 2016, 74, 370–371.
- Rosmarin, D.; Pandya, A.G.; Lebwohl, M.; Grimes, P.; Hamzavi, I.; Gottlieb, A.B.; Butler, K.; Kuo, F.; Sun, K.; Ji, T.; et al. Ruxolitinib cream for treatment of vitiligo: A randomised, controlled, phase 2 trial. Lancet 2020, 396, 110–120.
- Rothstein, B.; Joshipura, D.; Saraiya, A.; Abdat, R.; Ashkar, H.; Turkowski, Y.; Vaneeta Sheth, V.; Huang, V.; Chung, S.; Kachuk, C.; et al. Treatment of vitiligo with the topical Janus kinase inhibitor ruxolitinib. J. Am. Acad. Dermatol. 2017, 76, 1054–1060.
- Sheikh, A.; Rafique, W.; Owais, R.; Malik, F.; Ali, E. FDA approves Ruxolitinib (Opzelura) for Vitiligo Therapy: A breakthrough in the field of dermatology. Ann. Med. Surg. 2022, 81, 104499–104506.
- Shreberk-Hassidim, R.; Ramot, Y.; Zlotogorski, A. Janus kinase inhibitors in dermatology: A systematic review. J. Am. Acad. Dermatol. 2017, 76, 745–753.
- Chapman, S.; Kwa, M.; Gold, L.S.; Lim, H.W. Janus kinase inhibitors in dermatology: Part I. A comprehensive review. J. Am. Acad. Dermatol. 2022, 86, 406–413.
- Rosmarin, D.; Passeron, T.; Pandya, A.G.; Grimes, P.; Harris, J.E.; Desai, S.R.; Lebwohl, M.; Mulard, M.; Seneschal, J.; Wolkerstorfer, A.; et al. Two phase 3, randomized, controlled trials of ruxolitinib cream for vitiligo. N. Engl. J. Med. 2022, 387, 1445–1455.
- Seneschal, J.; Wolkerstorfer, A.; Desai, S.R.; Grimes, P.; Ezzedine, K.; Kornacki, D.; Butler, K.; Kuo, F.I.; Sun, K.; Grimes, P.; et al. Efficacy and safety of ruxolitinib cream for the treatment of vitiligo by patient demographics and baseline clinical characteristics: Week 52 pooled subgroup analysis from two randomized phase 3 studies. Br. J. Dermatol. 2023, 188 (Suppl. S1), ljac106-006.
- Sripathi, S.K.; Lalitha, P. Keratolytic Molecule Aided Inhibition of DNA Damage and Tyrosinase Activity of a Herbal Formulation. Int. J. BioSci. Technol. 2016, 9, 7–14.
- Arif, T. Salicylic acid as a peeling agent: A comprehensive review. Clin. Cosmet. Investig. Dermatol. 2015, 8, 455–461.
- Liu, J.; Jiang, R.; Zhou, J.; Xu, X.; Sun, Z.; Li, J.; Chen, X.; Li, Z.; Yan, X.; Zhao, D.; et al. Salicylic acid in ginseng root alleviates skin hyperpigmentation disorders by inhibiting melanogenesis and melanosome transport. Eur. J. Pharmacol. 2021, 910, 174458.
- Karnes, J.B.; Usatine, R.P. Management of external genital warts. Am. Fam. Physician 2014, 90, 312–318.
- Lu, J.; Cong, T.; Wen, X.; Li, X.; Du, D.; He, G.; Jiang, X. Salicylic acid treats acne vulgaris by suppressing AMPK/SREBP 1 pathway in sebocytes. Exp. Dermatol. 2019, 28, 786–794.
- Yeoh, S.C.; Goh, C.F. Topical delivery of salicylates. Drug Deliv. Transl. Res. 2021, 12, 981–1001.
- Kanlayavattanakul, M.; Lourith, N. Plants and natural products for the treatment of skin hyperpigmentation–A review. Planta Med. 2018, 84, 988–1006.
- Hollinger, J.C.; Angra, K.; Halder, R.M. Are natural ingredients effective in the management of hyperpigmentation? A systematic review. J. Clin. Aesthetic Dermatol. 2018, 11, 28–37.
- Panzella, L.; Napolitano, A. Natural and bioinspired phenolic compounds as tyrosinase inhibitors for the treatment of skin hyperpigmentation: Recent advances. Cosmetics 2019, 6, 57.
- Grimes, P.; Bhawan, J.; Howell, M.; Desai, S.; Coryell, E.; Einziger, M.; Simpson, A.; Yaroshinsky, A.; McCraw, T. Histopathological Changes Induced by Malassezin: A Novel Natural Microbiome Indole for Treatment of Facial Hyperpigmentation. J. Drugs Dermatol. JDD 2022, 21, 141–145.
- Karadas, F.; Erdoğan, S.; Kor, D.; Oto, G.; Uluman, M. The effects of different types of antioxidants (Se, vitamin E and carotenoids) in broiler diets on the growth performance, skin pigmentation and liver and plasma antioxidant concentrations. Braz. J. Poult. Sci. 2016, 18, 101–116.
- Lucock, M.D. The evolution of human skin pigmentation: A changing medley of vitamins, genetic variability, and UV radiation during human expansion. Am. J. Biol. Anthropol. 2023, 180, 252–271.
- Rembe, J.D.; Fromm-Dornieden, C.; Stuermer, E.K. Effects of vitamin B complex and vitamin C on human skin cells: Is the perceived effect measurable? Adv. Skin Wound Care 2018, 31, 225–233.
- Farzanfar, S.; Kouzekonan, G.S.; Mirjani, R.; Shekarchi, B. Vitamin B12-loaded polycaprolacton/gelatin nanofibrous scaffold as potential wound care material. Biomed. Eng. Lett. 2020, 10, 547–554.
- Vivcharenko, V.; Wojcik, M.; Przekora, A. Cellular response to vitamin C-enriched chitosan/agarose film with potential application as artificial skin substitute for chronic wound treatment. Cells 2020, 9, 1185.
- Barrios-Garay, K.; Toledano-Serrabona, J.; Gay-Escoda, C.; Sánchez-Garcés, M.Á. Clinical effect of vitamin C supplementation on bone healing: A systematic review. Med. Oral Patol. Oral Y Cirugía Bucal 2022, 27, e205–e215.
- Al-Niaimi, F.; Chiang, N.Y.Z. Topical vitamin C and the skin: Mechanisms of action and clinical applications. J. Clin. Aesthetic Dermatol. 2017, 10, 14–17.
- Ravetti, S.; Clemente, C.; Brignone, S.; Hergert, L.; Allemandi, D.; Palma, S. Ascorbic acid in skin health. Cosmetics 2019, 6, 58.
- Ahn, K.Y.; Song, H.J.; Kim, D.C. Effect of alpha-tocopheryl acetate, retinyl palmitate, and phytantriol on hair protection. J. Appl. Biol. Chem. 2022, 65, 307–312.
- Santos, J.S.; Tavares, G.D.; Barradas, T.N. Vitamin E and derivatives in skin health promotion. In Vitamin E in Health and Disease-Interactions, Diseases and Health Aspects; IntechOpen: London, UK, 2021.
- Putranti, A.R.; Primaharinastiti, R.; Hendradi, E. Effectivity and physicochemical stability of nanostructured lipid carrier coenzyme Q10 in different ratio of lipid cetyl palmitate and alpha tocopheryl acetate as carrier. Asian J. Pharm. Clin. Res. 2017, 10, 146–152.
- Panichakul, T.; Rodboon, T.; Suwannalert, P.; Tripetch, C.; Rungruang, R.; Boohuad, N.; Youdee, P. Additive effect of a combination of Artocarpus lakoocha and Glycyrrhiza glabra extracts on tyrosinase inhibition in melanoma B16 cells. Pharmaceuticals 2020, 13, 310.
- Gupta, A.K.; Pathak, U.; Medhi, M.; Mastinu, A.; Sikarwar, M.S.; Mishra, P. Botanical, chemical and pharmacological properties of artocarpus lakoocha (monkey fruit): A review. Agric. Rev. 2020, 41, 305–316.
- Ullah, S.; Shoaib, R.; Khan, S.; Masood, A. Phytochemicals; Targeted-Based Therapeutic Approaches for Pigmentation Disorders. Open Access Indones. J. Med. Rev. 2023, 3, 368–381.
- Vaughn, A.R.; Clark, A.K.; Sivamani, R.K.; Shi, V.Y. Natural oils for skin-barrier repair: Ancient compounds now backed by modern science. Am. J. Clin. Dermatol. 2018, 19, 103–117.
- Sarkic, A.; Stappen, I. Essential oils and their single compounds in cosmetics—A critical review. Cosmetics 2018, 5, 11.
- Ali, S.A.; Galgut, J.M.; Choudhary, R.K. On the novel action of melanolysis by a leaf extract of Aloe vera and its active ingredient aloin, potent skin depigmenting agents. Planta Med. 2012, 78, 767–771.
- Gad, H.A.; Roberts, A.; Hamzi, S.H.; Gad, H.A.; Touiss, I.; Altyar, A.E.; Kensara, A.O.; Ashour, M.L. Jojoba Oil: An updated comprehensive review on chemistry, pharmaceutical uses, and toxicity. Polymers 2021, 13, 1711.
- Matsumoto, Y.; Ma, S.; Tominaga, T.; Yokoyama, K.; Kitatani, K.; Horikawa, K.; Suzuki, K. Acute effects of transdermal administration of jojoba oil on lipid metabolism in mice. Medicina 2019, 55, 594.
- Blaak, J.; Staib, P. An updated review on efficacy and benefits of sweet almond, evening primrose and jojoba oils in skin care applications. Int. J. Cosmet. Sci. 2022, 44, 1–9.
- Sturtevant, D.; Lu, S.; Zhou, Z.W.; Shen, Y.; Wang, S.; Song, J.M.; Zhong, J.; Burks, D.J.; Yang, Z.Q.; Yang, Q.Y.; et al. The genome of jojoba (Simmondsia chinensis): A taxonomically isolated species that directs wax ester accumulation in its seeds. Sci. Adv. 2020, 6, e3240–e3253.
- Nasr, M.; Abdel-Hamid, S.; Moftah, N.H.; Fadel, M.; Alyoussef, A.A. Jojoba oil soft colloidal nanocarrier of a synthetic retinoid: Preparation, characterization and clinical efficacy in psoriatic patients. Curr. Drug Deliv. 2017, 14, 426–432.
- Sánchez, M.; Avhad, M.R.; Marchetti, J.M.; Martínez, M.; Aracil, J. Jojoba oil: A state of the art review and future prospects. Energy Convers. Manag. 2016, 129, 293–304.
- Manoharan, S.; Vishnupriya, V.; Gayathri, R. Phytochemical analysis and in vitro antioxidant activity of jojoba oil. J. Pharm. Sci. Res. 2016, 8, 512–516.
- Goik, U.; Goik, T.; Załęska, I. The properties and application of argan oil in cosmetology. Eur. J. Lipid Sci. Technol. 2019, 121, 1800313–1800342.
- Phong, C.; Lee, V.; Yale, K.; Sung, C.; Mesinkovska, N. Coconut, Castor, and Argan Oil for Hair in Skin of Color Patients: A Systematic Review. J. Drugs Dermatol. JDD 2022, 21, 751–757.
- Charrouf, Z.; Guillaume, D. The argan oil project: Going from utopia to reality in 20 years. OCL 2018, 25, D209–D214.
- Leite, C.D.S.; Bonafé, G.A.; Carvalho Santos, J.; Martinez, C.A.R.; Ortega, M.M.; Ribeiro, M.L. The anti-inflammatory properties of licorice (Glycyrrhiza glabra)-derived compounds in intestinal disorders. Int. J. Mol. Sci. 2022, 23, 4121.
- Kwon, Y.J.; Son, D.H.; Chung, T.H.; Lee, Y.J. A review of the pharmacological efficacy and safety of licorice root from corroborative clinical trial findings. J. Med. Food 2020, 23, 12–20.
- Mohiuddin, A.K. Skin lightening & management of hyperpigmentation. Pharma Sci. Anal. Res. J. 2019, 2, 180020–180068.
- Kimyon, R.S.; Liou, Y.L.; Schlarbaum, J.P.; Warshaw, E.M. Allergic contact dermatitis to licorice root extract. Dermatitis® 2019, 30, 227–228.
- Spencer, J.M.; Accioly, J.; Kitchen, N. Double Blind, Placebo Controlled Evaluation of a Novel Skin Lightening Agent. J. Drugs Dermatol. JDD 2018, 17, 113–115.
- Dhariwala, M.Y.; Ravikumar, P. An overview of herbal alternatives in androgenetic alopecia. J. Cosmet. Dermatol. 2019, 18, 966–975.
- Boscariol, R.; Junior, J.M.O.; Baldo, D.A.; Balcão, V.M.; Vila, M.M. Transdermal permeation of curcumin promoted by choline geranate ionic liquid: Potential for the treatment of skin diseases. Saudi Pharm. J. 2022, 30, 382–397.
- Vo, T.S.; Vo, T.T.B.C.; Vo, T.T.T.N.; Lai, T.N.H. Turmeric (Curcuma longa L.): Chemical components and their effective clinical applications. J. Turk. Chem. Soc. Sect. A Chem. 2021, 8, 883–898.
- Firmansyah, D.; Sumiwi, S.A.; Saptarini, N.M.; Levita, J. Curcuma longa extract inhibits the activity of mushroom tyrosinase and the growth of murine skin cancer B16F10 cells. J. Herbmed Pharmacol. 2023, 12, 153–158.
- Farooqui, R.K.; Kaurav, M.; Kumar, M.; Sudheesh, M.S.; Pandey, R.S. Permeation enhancer nanovesicles mediated topical delivery of curcumin for the treatment of hyperpigmentation. J. Liposome Res. 2022, 32, 332–339.
- Akter, J.; Islam, M.Z.; Hossain, M.A.; Takara, K. Anti-tyrosinase properties of different species of turmeric and isolation of active compounds from Curcuma amada. Med. Chem. Res. 2021, 30, 1669–1676.
- Rodríguez-Cid, L.; Qian, W.; Iribarra-Araya, J.; Etcheverry-Berríos, Á.; Martínez-Olmos, E.; Choquesillo-Lazarte, D.; Sañudo, E.C.; Roubeau, O.; Periago, A.M.L.; González-Camp, A.; et al. Broadening the scope of high structural dimensionality nanomaterials using pyridine-based curcuminoids. Dalton Trans. 2021, 50, 7056–7064.
- Colantonio, S.; Rivers, J.K. Botanicals with dermatologic properties derived from first nations healing: Part 2—Plants and algae. J. Cutan. Med. Surg. 2017, 21, 299–307.
- Vaughn, A.R.; Clark, A.K.; Notay, M.; Sivamani, R.K. Randomized controlled pilot study of dietary supplementation with turmeric or herbal combination tablets on skin barrier function in healthy subjects. J. Med. Food 2018, 21, 1260–1265.
- Kallis, P.J.; Price, A.; Dosal, J.R.; Nichols, A.J.; Keri, J. A Biologically Based Approach to Acne and Rosacea. J. Drugs Dermatol. JDD 2018, 17, 611–617.
- Song, X.C.; Canellas, E.; Wrona, M.; Becerril, R.; Nerin, C. Comparison of two antioxidant packaging based on rosemary oleoresin and green tea extract coated on polyethylene terephthalate for extending the shelf life of minced pork meat. Food Packag. Shelf Life 2020, 26, 100588–100597.
- Bagheri, R.; Rashidlamir, A.; Ashtary-Larky, D.; Wong, A.; Alipour, M.; Motevalli, M.S.; Chebbi, A.; Laher, I.; Zouhal, H. Does green tea extract enhance the anti-inflammatory effects of exercise on fat loss? Br. J. Clin. Pharmacol. 2020, 86, 753–762.
- Gaweł-Bęben, K.; Kukula-Koch, W.; Hoian, U.; Czop, M.; Strzępek-Gomółka, M.; Antosiewicz, B. Characterization of Cistus× incanus L. and Cistus ladanifer L. extracts as potential multifunctional antioxidant ingredients for skin protecting cosmetics. Antioxidants 2020, 9, 202.
- Tang, G.; Xu, Y.; Zhang, C.; Wang, N.; Li, H.; Feng, Y. Green tea and epigallocatechin gallate (EGCG) for the management of nonalcoholic fatty liver diseases (NAFLD): Insights into the role of oxidative stress and antioxidant mechanism. Antioxidants 2021, 10, 1076.
- Hodges, J.K.; Sasaki, G.Y.; Bruno, R.S. Anti-inflammatory activities of green tea catechins along the gut–liver axis in nonalcoholic fatty liver disease: Lessons learned from preclinical and human studies. J. Nutr. Biochem. 2020, 85, 108478–108524.
- Chaikul, P.; Sripisut, T.; Chanpirom, S.; Ditthawutthikul, N. Anti-skin aging activities of green tea (Camelliasinensis (L) Kuntze) in B16F10 melanoma cells and human skin fibroblasts. Eur. J. Integr. Med. 2020, 40, 101212–101240.
- Bhattacharya, S.; Sherje, A.P. Development of resveratrol and green tea sunscreen formulation for combined photoprotective and antioxidant properties. J. Drug Deliv. Sci. Technol. 2020, 60, 102000–102023.
- Winkelman, W.J. Aromatherapy, botanicals, and essential oils in acne. Clin. Dermatol. 2018, 36, 299–305.
- Patidar, K. Unmet Need and Challenges of Skin Aging by Herbal Anti-aging Cosmeceuticals: An Overview. Asian J. Pharm. (AJP) 2018, 12, 410–418.
- Phasha, V.; Senabe, J.; Ndzotoyi, P.; Okole, B.; Fouche, G.; Chuturgoon, A. Review on the use of kojic acid—A skin-lightening ingredient. Cosmetics 2022, 9, 64.
- Saeedi, M.; Eslamifar, M.; Khezri, K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed. Pharmacother. 2019, 110, 582–593.
- Khezri, K.; Saeedi, M.; Morteza-Semnani, K.; Akbari, J.; Hedayatizadeh-Omran, A. A promising and effective platform for delivering hydrophilic depigmenting agents in the treatment of cutaneous hyperpigmentation: Kojic acid nanostructured lipid carrier. Artif. Cells Nanomed. Biotechnol. 2021, 49, 38–47.
- Khan, A.; Park, T.J.; Ikram, M.; Ahmad, S.; Ahmad, R.; Jo, M.G.; Kim, M.O. Antioxidative and Anti-inflammatory Effects of Kojic Acid in Aβ-Induced Mouse Model of Alzheimer’s Disease. Mol. Neurobiol. 2021, 58, 5127–5140.
- Zilles, J.C.; Dos Santos, F.L.; Kulkamp-Guerreiro, I.C.; Contri, R.V. Biological activities and safety data of kojic acid and its derivatives: A review. Exp. Dermatol. 2022, 31, 1500–1521.
- Bakhouche, I.; Aliat, T.; Boubellouta, T.; Gali, L.; Şen, A.; Bellik, Y. Phenolic contents and in vitro antioxidant, anti-tyrosinase, and anti-inflammatory effects of leaves and roots extracts of the halophyte Limonium delicatulum. S. Afr. J. Bot. 2021, 139, 42–49.
- Li, T.X.; Liang, J.X.; Liu, L.L.; Shi, F.C.; Jia, X.W.; Li, M.H.; Xu, C.P. Novel kojic acid derivatives with anti-inflammatory effects from Aspergillus versicolor. Fitoterapia 2021, 154, 105027–105033.
- Gust, P.J.; Luke, J.D. Kojic acid. J. Dermatol. Nurses’ Assoc. 2016, 8, 338–340.
- Searle, T.; Al-Niaimi, F.; Ali, F.R. The top 10 cosmeceuticals for facial hyperpigmentation. Dermatol. Ther. 2020, 33, e14095–e14139.
- Ohno, Y.; Kondo, S.; Tajima, K.; Shibata, T.; Itoh, T. Effect of phlorotannins isolated from Eisenia bicyclis on melanogenesis in mouse B16 melanoma cells. Nat. Prod. Commun. 2021, 16, 1934578X211019264.
- Phang, S.J.; Teh, H.X.; Looi, M.L.; Arumugam, B.; Fauzi, M.B.; Kuppusamy, U.R. Phlorotannins from brown algae: A review on their antioxidant mechanisms and applications in oxidative stress-mediated diseases. J. Appl. Phycol. 2023, 35, 867–892.
- Jesumani, V.; Du, H.; Aslam, M.; Pei, P.; Huang, N. Potential use of seaweed bioactive compounds in skincare—A review. Mar. Drugs 2019, 17, 688.
- Zhao, W.; Yang, A.; Wang, J.; Huang, D.; Deng, Y.; Zhang, X.; Qu, Q.; Ma, W.; Xiong, R.; Zhu, M.; et al. Potential application of natural bioactive compounds as skin-whitening agents: A review. J. Cosmet. Dermatol. 2022, 21, 6669–6687.
- Kim, K.N.; Yang, H.M.; Kang, S.M.; Ahn, G.; Roh, S.W.; Lee, W.; Kim, D.K.; Jeon, Y.J. Whitening effect of octaphlorethol A isolated from Ishige foliacea in an in vivo zebrafish model. J. Microbiol. Biotechnol. 2015, 25, 448–451.
- Lee, S.H.; Kang, N.; Kim, E.A.; Heo, S.J.; Moon, S.H.; Jeon, B.T.; Jeon, Y.J. Antidiabetogenic and antioxidative effects of octaphlorethol a isolated from the brown algae Ishige foliacea in streptozotocin-induced diabetic mice. Food Sci. Biotechnol. 2014, 23, 1261–1266.
- Thawabteh, A.M.; Swaileh, Z.; Ammar, M.; Jaghama, W.; Yousef, M.; Karaman, R.; Bufo, S.A.; Scrano, L. Antifungal and Antibacterial Activities of Isolated Marine Compounds. Toxins 2023, 15, 93.
- Shanura Fernando, I.P.; Asanka Sanjeewa, K.K.; Samarakoon, K.W.; Kim, H.S.; Gunasekara, U.K.D.S.S.; Park, Y.J.; Abeytunga, D.T.U.; Lee, W.W.; Jeon, Y.J. The potential of fucoidans from Chnoospora minima and Sargassum polycystum in cosmetics: Antioxidant, anti-inflammatory, skin-whitening, and antiwrinkle activities. J. Appl. Phycol. 2018, 30, 3223–3232.
- Kok, J.M.L.; Jee, J.M.; Chew, L.Y.; Wong, C.L. The potential of the brown seaweed Sargassum polycystum against acne vulgaris. J. Appl. Phycol. 2016, 28, 3127–3133.
- Lourenço-Lopes, C.; Fraga-Corral, M.; Soria-Lopez, A.; Nuñes-Estevez, B.; Barral-Martinez, M.; Silva, A.; Li, N.; Liu, C.; Gandara, J.S.; Prieto, M.A. Fucoxanthin’s optimization from Undaria pinnatifida using conventional heat extraction, bioactivity assays and in silico studies. Antioxidants 2022, 11, 1296.
- Park, E.J.; Choi, J.I. Melanogenesis inhibitory effect of low molecular weight fucoidan from Undaria pinnatifida. J. Appl. Phycol. 2017, 29, 2213–2217.
- Lee, S.H.; Kang, S.M.; Ko, S.C.; Lee, D.H.; Jeon, Y.J. Octaphlorethol A, a novel phenolic compound isolated from a brown alga, Ishige foliacea, increases glucose transporter 4-mediated glucose uptake in skeletal muscle cells. Biochem. Biophys. Res. Commun. 2012, 420, 576–581.
- Lajis, A.F.B.; Ariff, A.B. Discovery of new depigmenting compounds and their efficacy to treat hyperpigmentation: Evidence from in vitro study. J. Cosmet. Dermatol. 2019, 18, 703–727.
- Haggag, Y.A.; Abd Elrahman, A.A.; Ulber, R.; Zayed, A. Fucoidan in pharmaceutical formulations: A comprehensive review for smart drug delivery systems. Mar. Drugs 2023, 21, 112.
- Guan, B.; Chen, K.; Tong, Z.; Chen, L.; Chen, Q.; Su, J. Advances in fucoxanthin research for the prevention and treatment of inflammation-related diseases. Nutrients 2022, 14, 4768.
- Natsume, C.; Aoki, N.; Aoyama, T.; Senda, K.; Matsui, M.; Ikegami, A.; Tanaka, K.; Azuma, Y.T.; Fujita, T. Fucoxanthin ameliorates atopic dermatitis symptoms by regulating keratinocytes and regulatory innate lymphoid cells. Int. J. Mol. Sci. 2020, 21, 2180.
- Garcia-Jimenez, A.; Teruel-Puche, J.A.; Berna, J.; Rodriguez-Lopez, J.N.; Tudela, J.; Garcia-Ruiz, P.A.; Garcia-Canovas, F. Characterization of the action of tyrosinase on resorcinols. Bioorg. Med. Chem. 2016, 24, 4434–4443.
- Xie, X.Y.; Fu, G.L.; Yang, Q.; Zeng, Y.; Ke, H.; Lu, J.J.; Yi, H. Clinical Efficacy of 755 nm Laser Treatment of Lip Mucosal Pigmentation in Children with Peutz–Jeghers Syndrome. Dermatol. Ther. 2023, 2023, 8020443–8020447.
- Nunez, J.H.; Strong, A.L.; Comish, P.; Hespe, G.E.; Harvey, J.; Sorkin, M.; Levi, B. A Review of Laser Therapies for the Treatment of Scarring and Vascular Anomalies. Adv. Wound Care 2023, 12, 68–84.
- Purohit, S.J.; Tharmavaram, M.; Rawtani, D.; Prajapati, P.; Pandya, H.; Dey, A. Niosomes as cutting edge nanocarrier for controlled and targeted delivery of essential oils and biomolecules. J. Drug Deliv. Sci. Technol. 2022, 73, 103438.
- Sharma, S.; Vashist, S.; Lamba, A.K.; Arora, S. Novel Strategies in the Treatment of Acne: A Review. Int. J. Pharm. Investig. 2022, 12, 123–128.
- Yonekawa, Y.; Thomas, B.J.; Thanos, A.; Todorich, B.; Drenser, K.A.; Trese, M.T.; Capone Jr, A. The cutting edge of retinopathy of prematurity care: Expanding the boundaries of diagnosis and treatment. Retina 2017, 37, 2208–2225.
- Al Qarqaz, F.; Al-Yousef, A. Skin microneedling for acne scars associated with pigmentation in patients with dark skin. J. Cosmet. Dermatol. 2018, 17, 390–395.
- Ziaeifar, E.; Ziaeifar, F.; Mozafarpoor, S.; Goodarzi, A. Applications of microneedling for various dermatologic indications with a special focus on pigmentary disorders: A comprehensive review study. Dermatol. Ther. 2021, 34, e151–e159.
- Lima, E.V.A.; Lima, M.M.D.A.; Miot, H.A. Induction of pigmentation through microneedling in stable localized vitiligo patients. Dermatol. Surg. 2020, 46, 434–435.
- Ahmed, N.A.; Mohammed, S.S.; Fatani, M.I. Treatment of periorbital dark circles: Comparative study of carboxy therapy vs chemical peeling vs mesotherapy. J. Cosmet. Dermatol. 2019, 18, 169–175.
- Sarkar, R.; Arsiwala, S.; Dubey, N.; Sonthalia, S.; Das, A.; Arya, L.; Gokhale, N.; Torsekar, R.G.; Somani, V.K.; Majid, I.; et al. Chemical peels in melasma: A review with consensus recommendations by Indian pigmentary expert group. Indian J. Dermatol. 2017, 62, 578–584.
- Kadry, M.; Tawfik, A.; Abdallah, N.; Badawi, A.; Shokeir, H. Platelet-rich plasma versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of vitiligo: A comparative study. Clin. Cosmet. Investig. Dermatol. 2018, 11, 551–559.
- Mohamad, N.E.; ELgameel, R.M.; Mohamed, M.H. Comparative study between the effectiveness of plasma skin regeneration versus micro-needling in the treatment of striae distensae. J. Cosmet. Dermatol. 2022, 21, 4545–4553.
- Wulandari, P.; Jusuf, N.K.; Nasution, K. Microneedling and platelet-rich plasma (PRP) treatment for mixed melasma. J. Gen. Proced. Dermatol. Venereol. Indones. 2022, 6, 44.
- Rezapour, A.; Arabloo, J.; Moradi, N.; Ehsanzadeh, S.J.; Hourzad, M.; Alipour, V. Safety and effectiveness of endodermal radiofrequency for skin rejuvenation: A systematic review. Aesthetic Plast. Surg. 2023, 47, 378–386.
- Goel, A.; Gatne, V. Use of nanofractional radiofrequency for the treatment of acne scars in Indian skin. J. Cosmet. Dermatol. 2017, 16, 186–192.
