Acute myocardial infarction (AMI) remains the leading cause of mortality in the world, highlighting an urgent need for the development of novel, more effective approaches for the treatment of AMI. Remote postconditioning (RPost) of the heart could be a useful approach. It was demonstrated that RPost triggers infarct size reduction, improves contractile function of the heart in reperfusion, mitigates apoptosis, and stimulates autophagy in animals with coronary artery occlusion and reperfusion. Endogenous opioid peptides and adenosine could be involved in RPost. It was found that kinases and NO-synthase participate in RPost. KATP channels, MPT pore, and STAT3 could be hypothetical end-effectors of RPost.
- heart
- remote postconditioning
- ischemia
1. Introduction
2. Experimental Data
2.1. The Involvement of the Nervous System in the Mechanism of Remote Postconditioning
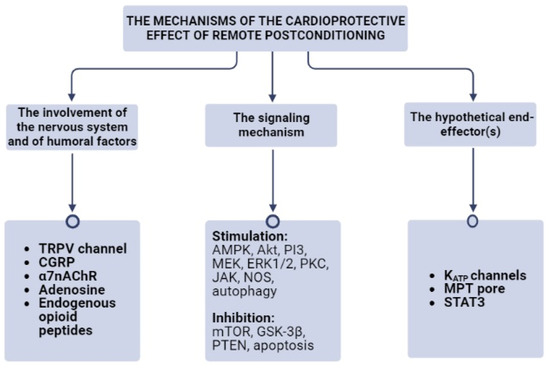
2.2. The Involvement of Humoral Factors in the Mechanism of Remote Postconditioning
3. The Signaling Mechanism of Remote Postconditioning
3.1. AMPK and mTOR
3.2. Akt, ERK, and PI3 Kinase
3.3. Protein Kinase C (PKC)
3.4. JAK
3.5. JNK and GSK-3β
3.6. PTEN
3.7. NO-Synthase
4. The Hypothetical End-Effector(s) of Remote Postconditioning
5. Remote Postconditioning and Experimental Metabolic Syndrome
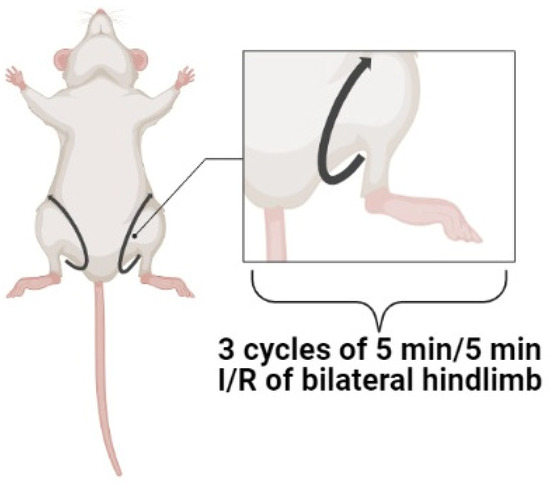
6. The Optimal Protocol of Remote Postconditioning
7. Remote Postconditioning in Clinical Practice
This entry is adapted from the peer-reviewed paper 10.3390/cells12121622
References
- Menees, D.S.; Peterson, E.D.; Wang, Y.; Curtis, J.P.; Messenger, J.C.; Rumsfeld, J.S.; Gurm, H.S. Door-to-balloon time and mortality among patients undergoing primary PCI. N. Engl. J. Med. 2013, 369, 901–909.
- Fabris, E.; Kilic, S.; Schellings, D.A.A.M.; Ten Berg, J.M.; Kennedy, M.W.; van Houwelingen, K.G.; Giannitsis, E.; Kolkman, E.; Ottervanger, J.P.; Hamm, C.; et al. Long-term mortality and prehospital tirofiban treatment in patients with ST elevation myocardial infarction. Heart 2017, 103, 1515–1520.
- Olier, I.; Sirker, A.; Hildick-Smith, D.J.R.; Kinnaird, T.; Ludman, P.; de Belder, M.A.; Baumbach, A.; Byrne, J.; Rashid, M.; Curzen, N.; et al. British Cardiovascular Intervention Society and the National Institute for Cardiovascular Outcomes Research. Association of different antiplatelet therapies with mortality after primary percutaneous coronary intervention. Association of different antiplatelet therapies with mortality after primary percutaneous coronary intervention. Heart 2018, 104, 1683–1690.
- Maslov, L.N.; Popov, S.V.; Mukhomedzyanov, A.V.; Naryzhnaya, N.V.; Voronkov, N.S.; Ryabov, V.V.; Boshchenko, A.A.; Khaliulin, I.; Prasad, N.R.; Fu, F.; et al. Reperfusion cardiac injury: Receptors and the signaling mechanisms. Curr. Cardiol. Rev. 2022, 18, 63–79.
- Wang, Q.; Cheng, Y.; Xue, F.S.; Yuan, Y.J.; Xiong, J.; Li, R.P.; Liao, X.; Liu, J.H. Postconditioning with vagal stimulation attenuates local and systemic inflammatory responses to myocardial ischemia reperfusion injury in rats. Inflamm. Res. 2012, 61, 1273–1282.
- Basalay, M.; Barsukevich, V.; Mastitskaya, S.; Mrochek, A.; Pernow, J.; Sjöquist, P.O.; Ackland, G.L.; Gourine, A.V.; Gourine, A. Remote ischaemic pre- and delayed postconditioning—Similar degree of cardioprotection but distinct mechanisms. Exp. Physiol. 2012, 97, 908–917.
- Song, Y.; Shan, J.G.; Xue, Z.; Wang, S.Y.; Xu, H.; Liu, Y.; Guo, Y.S.; Ren, X. Remote postconditioning induced by trauma protects the mouse heart against ischemia reperfusion injury. Involvement of the neural pathway and molecular mechanisms. Cardiovasc. Drugs Ther. 2016, 30, 271–280.
- Ren, X.; Roessler, A.E.; Lynch, T.L.; Haar, L.; Mallick, F.; Lui, Y.; Tranter, M.; Ren, M.H.; Xie, W.R.; Fan, G.C.; et al. Cardioprotection via the skin: Nociceptor-induced conditioning against cardiac MI in the NIC of time. Am. J. Physiol. Heart Circ. Physiol. 2019, 316, H543–H553.
- Gao, Y.; Song, J.; Chen, H.; Cao, C.; Lee, C. TRPV1 activation is involved in the cardioprotection of remote limb ischemic postconditioning in ischemia-reperfusion injury rats. Biochem. Biophys. Res. Commun. 2015, 463, 1034–1039.
- Kerendi, F.; Kin, H.; Halkos, M.E.; Jiang, R.; Zatta, A.J.; Zhao, Z.Q.; Guyton, R.A.; Vinten-Johansen, J. Remote postconditioning. Brief renal ischemia and reperfusion applied before coronary artery reperfusion reduces myocardial infarct size via endogenous activation of adenosine receptors. Basic Res. Cardiol. 2005, 100, 404–412.
- Klabunde, R.E. Dipyridamole inhibition of adenosine metabolism in human blood. Eur. J. Pharmacol. 1983, 93, 21–26.
- Breivik, L.; Helgeland, E.; Aarnes, E.K.; Mrdalj, J.; Jonassen, A.K. Remote postconditioning by humoral factors in effluent from ischemic preconditioned rat hearts is mediated via PI3K/Akt-dependent cell-survival signaling at reperfusion. Basic Res. Cardiol. 2011, 106, 135–145.
- Maslov, L.N.; Lishmanov, Y.B. Permeability of the blood-brain barrier for opioid peptides. Exp. Clin. Pharmacol. 2017, 80, 39–44. (In Russia)
- Xie, B.; Gao, X.; Huang, Y.; Zhang, Y.; Zhu, S. Remote Ischemic Postconditioning Inhibits Hippocampal Neuronal Apoptosis and Mitophagy after Cardiopulmonary Resuscitation in Rats. Shock 2021, 55, 74–82.
- Huang, Y.; Gao, X.; Zhou, X.; Zhang, Y.; Tan, Z.; Zhu, S. Remote Ischemic Postconditioning Inhibited Mitophagy to Achieve Neuroprotective Effects in the Rat Model of Cardiac Arrest. Neurochem. Res. 2021, 46, 573–583.
- Yu, H.H.; Ma, X.T.; Ma, X.; Chen, M.; Chu, Y.H.; Wu, L.J.; Wang, W.; Qin, C.; Tian, D.S. Remote Limb Ischemic Postconditioning Protects Against Ischemic Stroke by Promoting Regulatory T Cells Thriving. J. Am. Heart Assoc. 2021, 10, e023077.
- Skyschally, A.; Gent, S.; Amanakis, G.; Schulte, C.; Kleinbongard, P.; Heusch, G. Across-species transfer of protection by remote ischemic preconditioning with species-specific myocardial signal transduction by reperfusion injury salvage kinase and survival activating factor enhancement pathways. Circ. Res. 2015, 117, 279–288.
- Koyama, T.; Munakata, M.; Akima, T.; Kageyama, T.; Shibata, M.; Moritani, K.; Kanki, H.; Ishikawa, S.; Mitamura, H. Impact of postconditioning with lactate-enriched blood on in-hospital outcomes of patients with ST-segment elevation myocardial infarction. Int. J. Cardiol. 2016, 220, 146–148.
- Koyama, T. Lactated Ringer’s solution for preventing myocardial reperfusion injury. Int. J. Cardiol. Heart Vasc. 2017, 15, 1–8.
- Koyama, T.; Munakata, M.; Akima, T.; Miyamoto, K.; Kanki, H.; Ishikawa, S. Muscle squeezing immediately after coronary reperfusion therapy using postconditioning with lactate-enriched blood. Int. J. Cardiol. 2019, 275, 36–38.
- Chepelev, S.N.; Vismont, F.I.; Goubkin, S.V.; Maslov, L.N. The influence of old age on cardioprotective efficiency of pharmacological postconditioning using lactic acid in ischemia-reperfusion of the myocardium in experiment. Dokl. Natl. Acad. Sci. Belarus 2021, 65, 207–216.
- Yellon, D.M.; Downey, J.M. Preconditioning the myocardium: From cellular physiology to clinical cardiology. Physiol. Rev. 2003, 83, 1113–1151.
- de Miranda, D.C.; de Oliveira Faria, G.; Hermidorff, M.M.; Dos Santos Silva, F.C.; de Assis, L.V.M.; Isoldi, M.C. Pre- and Post-Conditioning of the Heart: An Overview of Cardioprotective Signaling Pathways. Curr. Vasc. Pharmacol. 2021, 19, 499–524.
- Tyagi, S.; Singh, N.; Virdi, J.K.; Jaggi, A.S. Diabetes abolish cardioprotective effects of remote ischemic conditioning: Evidences and possible mechanisms. J. Physiol. Biochem. 2019, 75, 19–28.
- Xu, S.; Xia, X.; Liu, Y.; Chen, F.; Gu, R.; Bian, X.; Xu, X.; Jia, C.; Lu, S.; Gu, Y.; et al. Remote cyclic compression ameliorates myocardial infarction injury in rats via AMPK-dependent pathway. Microvasc. Res. 2022, 141, 104313.
- Popov, S.V.; Mukhomedzyanov, A.V.; Voronkov, N.S.; Derkachev, I.A.; Boshchenko, A.A.; Fu, F.; Sufianova, G.Z.; Khlestkina, M.S.; Maslov, L.N. Regulation of autophagy of the heart in ischemia and reperfusion. Apoptosis 2022, 28, 55–80.
- Yu, Y.; Jia, X.J.; Zong, Q.F.; Zhang, G.J.; Ye, H.W.; Hu, J.; Gao, Q.; Guan, S.D. Remote ischemic postconditioning protects the heart by upregulating ALDH2 expression levels through the PI3K/Akt signaling pathway. Mol. Med. Rep. 2014, 10, 536–542.
- Gao, S.; Zhan, L.; Yang, Z.; Shi, R.; Li, H.; Xia, Z.; Yuan, S.; Wu, Q.P.; Wang, T.; Yao, S. Remote limb ischaemic postconditioning protects against myocardial ischaemia/reperfusion injury in mice: Activation of JAK/STAT3-mediated Nrf2-antioxidant signalling. Cell. Physiol. Biochem. 2017, 43, 1140–1151.
- Wang, X.; Wang, J.; Tu, T.; Iyan, Z.; Mungun, D.; Yang, Z.; Guo, Y. Remote ischemic postconditioning protects against myocardial ischemia-reperfusion injury by inhibition of the RAGE-HMGB1 pathway. Biomed. Res. Int. 2018, 2018, 4565630.
- Mukhomedzyanov, A.V.; Naryzhnaya, N.V.; Maslov, L.N. The role of protein kinase C and PI3-kinase in the mechanism of the cardioprotective effect of remote ischemic postconditioning. Bull. Sib. Med. 2021, 20, 6–10.
- Miura, T.; Miki, T. GSK-3β, a therapeutic target for cardiomyocyte protection. Circ. J. 2009, 73, 1184–1192.
- Milano, G.; Morel, S.; Bonny, C.; Samaja, M.; von Segesser, L.K.; Nicod, P.; Vassalli, G. A peptide inhibitor of c-Jun NH2-terminal kinase reduces myocardial ischemia-reperfusion injury and infarct size in vivo. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H1828–H1835.
- Li, H.X.; Cui, X.L.; Xue, F.S.; Yang, G.Z.; Liu, Y.Y.; Liu, Q.; Liao, X. Inhibition of glycogen synthase kinase-3β is involved in cardioprotection by α7nAChR agonist and limb remote ischemic postconditionings. Biosci. Rep. 2018, 38, BSR20181315.
- Hong, J.; Ge, H.W.; Liu, J.Q.; Sun, R.H.; Kong, F.J. Pharmacological Inhibition of PTEN Restores Remote Ischemic Postconditioning Cardioprotection in Hypercholesterolemic Mice: Potential Role of PTEN/AKT/GSK3β SIGNALS. Shock 2019, 52, 522–531.
- Popov, S.V.; Maslov, L.N.; Naryzhnaya, N.V.; Mukhomezyanov, A.V.; Krylatov, A.V.; Tsibulnikov, S.Y.; Ryabov, V.V.; Cohen, M.V.; Downey, J.M. The Role of Pyroptosis in Ischemic and Reperfusion Injury of the Heart. J. Cardiovasc. Pharmacol. Ther. 2021, 26, 562–574.
- Baxter, G.F.; Ferdinandy, P. Delayed preconditioning of myocardium: Current perspectives. Basic Res. Cardiol. 2001, 96, 329–344.
- Tang, Y.H.; Xu, J.J.; Li, J.X.; Cheng, X.S. Remote postconditioning induced by brief pulmonary ischemia and reperfusion attenuates myocardial reperfusion injury in rabbits. Chin. Med. J. 2011, 124, 1683–1688.
- Tang, Y.H.; Yang, J.S.; Xiang, H.Y.; Xu, J.J. PI3K-Akt/eNOS in remote postconditioning induced by brief pulmonary ischemia. Clin. Investig. Med. 2014, 37, E26–E37.
- Kleinbongard, P.; Skyschally, A.; Gent, S.; Pesch, M.; Heusch, G. STAT3 as a common signal of ischemic conditioning: A lesson on “rigor and reproducibility” in preclinical studies on cardioprotection. Basic Res. Cardiol. 2017, 113, 3.
- Behmenburg, F.; Trefz, L.; Dorsch, M.; Ströthoff, M.; Mathes, A.; Raupach, A.; Heinen, A.; Hollmann, M.W.; Berger, M.M.; Huhn, R. Milrinone-induced postconditioning requires activation of mitochondrial Ca2+-sensitive potassium (mBKCa) channels. J. Cardiothorac. Vasc. Anesth. 2018, 32, 2142–2148.
- Logvinov, S.V.; Naryzhnaya, N.V.; Kurbatov, B.K.; Gorbunov, A.S.; Birulina, Y.G.; Maslov, L.N.; Oeltgen, P.R. High carbohydrate high fat diet causes arterial hypertension and histological changes in the aortic wall in aged rats: The involvement of connective tissue growth factors and fibronectin. Exp. Gerontol. 2021, 154, 111543.
- Naryzhnaya, N.V.; Logvinov, S.V.; Kurbatov, B.K.; Mukhomedzyanov, A.V.; Sirotina, M.A.; Chepelev, S.N.; Vismont, F.I.; Maslov, L.N. The efficiency of remote ischemic postconditioning of the myocardium in rats with induced metabolic syndrome depends on the leptin level. Proc. Natl. Acad. Sci. Belarus Med. Ser. 2022, 19, 38–47.
- Logvinov, S.V.; Mukhomedzyanov, A.V.; Kurbatov, B.K.; Sirotina, M.A.; Naryzhnaya, N.V.; Maslov, L.N. Participation of Leptin and Corticosterone in the Decrease in Infarct-Limiting Efficiency of Remote Postconditioning and in the Development of Arterial Hypertension in Metabolic Syndrome in Rats. Bull. Exp. Biol. Med. 2023, 174, 312–317.
- Smith, C.C.; Dixon, R.A.; Wynne, A.M.; Theodorou, L.; Ong, S.G.; Subrayan, S.; Davidson, S.M.; Hausenloy, D.J.; Yellon, D.M. Leptin-induced cardioprotection involves JAK/STAT signaling that may be linked to the mitochondrial permeability transition pore. Am. J. Physiol. Heart Circ. Physiol. 2010, 299, H1265–H1270.
- Crimi, G.; Pica, S.; Raineri, C.; Bramucci, E.; De Ferrari, G.M.; Klersy, C.; Ferlini, M.; Marinoni, B.; Repetto, A.; Romeo, M.; et al. Remote ischemic post-conditioning of the lower limb during primary percutaneous coronary intervention safely reduces enzymatic infarct size in anterior myocardial infarction: A randomized controlled trial. JACC Cardiovasc. Interv. 2013, 6, 1055–1063.
- Zhong, H.; Gao, Z.; Chen, M.; Zhao, J.; Wang, F.; Li, L.; Dong, H.; Liu, L.; Wang, Q.; Xiong, L. Cardioprotective effect of remote ischemic postconditioning on children undergoing cardiac surgery: A randomized controlled trial. Paediatr. Anaesth. 2013, 23, 726–733.
- Hong, D.M.; Lee, E.H.; Kim, H.J.; Min, J.J.; Chin, J.H.; Choi, D.K.; Bahk, J.H.; Sim, J.Y.; Choi, I.C.; Jeon, Y. Does remote ischaemic preconditioning with postconditioning improve clinical outcomes of patients undergoing cardiac surgery? Remote Ischaemic Preconditioning with Postconditioning Outcome Trial. Eur. Heart J. 2014, 35, 176–183.
- Prunier, F.; Angoulvant, D.; Saint Etienne, C.; Vermes, E.; Gilard, M.; Piot, C.; Roubille, F.; Elbaz, M.; Ovize, M.; Bière, L.; et al. The RIPOST-MI study, assessing remote ischemic perconditioning alone or in combination with local ischemic postconditioning in ST-segment elevation myocardial infarction. Basic Res. Cardiol. 2014, 109, 400.
- Wang, N.; Wang, G.S.; Yu, H.Y.; Mi, L.; Guo, L.J.; Gao, W. Myocardial protection of remote ischemic postconditioning during primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction. Beijing Da Xue Xue Bao 2014, 46, 838–843.
- Eitel, I.; Stiermaier, T.; Rommel, K.P.; Fuernau, G.; Sandri, M.; Mangner, N.; Linke, A.; Erbs, S.; Lurz, P.; Boudriot, E.; et al. Cardioprotection by combined intrahospital remote ischaemic perconditioning and postconditioning in ST-elevation myocardial infarction: The randomized LIPSIA CONDITIONING trial. Eur. Heart J. 2015, 36, 3049–3057.
- Cho, Y.J.; Lee, E.H.; Lee, K.; Kim, T.K.; Hong, D.M.; Chin, J.H.; Choi, D.K.; Bahk, J.H.; Sim, J.Y.; Choi, I.C.; et al. Long-term clinical outcomes of Remote Ischemic Preconditioning and Postconditioning Outcome (RISPO) trial in patients undergoing cardiac surgery. Int. J. Cardiol. 2017, 231, 84–89.
- Hausenloy, D.J.; Kharbanda, R.K.; Møller, U.K.; Ramlall, M.; Aarøe, J.; Butler, R.; Bulluck, H.; Clayton, T.; Dana, A.; Dodd, M.; et al. CONDI-2/ERIC-PPCI Investigators. Effect of remote ischaemic conditioning on clinical outcomes in patients with acute myocardial infarction (CONDI-2/ERIC-PPCI): A single-blind randomised controlled trial. Lancet 2019, 394, 1415–1424.
- Ikonomidis, I.; Vlastos, D.; Andreadou, I.; Gazouli, M.; Efentakis, P.; Varoudi, M.; Makavos, G.; Kapelouzou, A.; Lekakis, J.; Parissis, J.; et al. Vascular conditioning prevents adverse left ventricular remodelling after acute myocardial infarction: A randomised remote conditioning study. Basic Res. Cardiol. 2021, 116, 9.
- Garcia-de-la-Asuncion, J.; Moreno, T.; Duca, A.; García-Del-Olmo, N.; Perez-Griera, J.; Belda, J.; Soro, M.; García-Del-Olmo, E. Effects of remote ischemic postconditioning on HIF-1α and other markers in on-pump cardiac surgery. Gen. Thorac. Cardiovasc. Surg. 2022, 70, 239–247.
