Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Gastroenterology & Hepatology
The intestinal immune balance is disrupted by a high-fat diet (HFD) in several ways, such as impairing the intestinal barrier, influencing immune cells, and altering the gut microbiota. In contrast, a rational diet is thought to maintain intestinal immunity by regulating gut microbiota.
- high-fat diet
- inflammatory bowel disease
- intestinal barrier
- intestinal microflora
1. Introduction
Inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), causes significant gastrointestinal symptoms, such as diarrhea, abdominal pain, bleeding, and weight loss. IBD is associated with a spectrum of extraintestinal manifestations, including sclerosing cholangitis, uveitis, arthritis, erythema nodosum, and pyoderma gangrenosum [1]. The steadily increasing emergence of IBD has cause great burden to the health care system and society worldwide; therefore, it is important to explore its underlying pathogenesis. Although identifying its exact pathogenesis remains difficult, overwhelming data suggests that its prevalence is related to Western diets [2] which feature high saturated fat, high sugar (HS), and low fiber exposure [3,4]. Similar to Western diets, a high fat diet (HFD) contains high amounts of fatty acids and is low in fiber and vitamins [5]. This dietary shift has been proposed as an etiological factor of IBD because the accelerating incidence of IBD in newly industrialized countries is in line with the westernized dietary structure [6,7,8]. The severity of IBD is also influenced by hormonal regulation under food intake [9]. For example, ghrelin is not only a multi-faceted gut hormone that regulates gastrointestinal motility, stimulates food intake, and promotes fat deposition [10]; it is also a mediator to prevent intestinal inflammation [10,11]. Research demonstrates that ghrelin supplements can alleviate inflammation in different models of IBD or accelerate the healing of gastrointestinal ulceration [12,13,14,15,16,17], while consequently a high fat diet could decrease levels of ghrelin and impair its anti-inflammatory effect [18]. Additionally, HFD can reduce the secretion of somatostatin and increase the level of serotonin [19,20], resulting in the exacerbated inflammation of IBD [20,21]. Therefore, to adopt appropriate therapies to treat IBD, it is imperative to uncover the mechanisms between diet and IBD and their potential implication in reducing IBD morbidity, achieving IBD remission, and reducing the disease burden on patients and healthcare systems.
Intestinal immunity, as a pivotal factor in IBD pathogenesis, cannot be underestimated in IBD progression because of its unique roles in warding off pathogen invasion from the gut and retaining host–microbial immune homeostasis [22]. The dysfunction of intestinal immunity may lead, for various reasons, to increased intestinal permeability and makes it easier for pathogens and their products to enter host tissues, thus resulting in worsening conditions [23]. Therefore, increased intestinal permeability has significance in predicting disease recurrence in IBD [24,25]. Moreover, the dysregulation of adaptive immunity is also a predictor of the clinical course of IBD [26], and genetics are also essential participants in these immune processes [27]. These studies conclude that intestinal immunity is intimately involved in the pathogenesis of IBD. The intestinal microbiota has been linked to the development of IBD for many years. Firmicutes and Bacteroidetes are the predominant bacteria in the human intestine; however, a lower proportion of these species was found in IBD patients, both in children and adults [28]. Notably, these two obligate anaerobes are responsible for catabolizing fiber into short-chain fatty acids. A reduction in their abundance would reduce the production of short chain fatty acids and result in IBD occurrence or accelerate the IBD course due to the loss of their anti-inflammatory properties [29,30].
Additionally, an increase in adherent–invasive E. Coli (AIEC), which plays a pathogenic effect on disease development with the ability to adhere and invade intestinal epithelial cells [31], was also displayed in CD patients. The role of gut microbiota composition and function in the development and severity of IBD is demonstrated by the changes in microbiota composition among IBD patients observed in these studies. Engineering the microbiota as an adjunct to boost current IBD therapies would be a promising approach.
Because of the meaningful roles of diet, intestinal immunity, and microbiota in IBD, many studies have attempted to explore their links to the three entities in IBD (Figure 1).
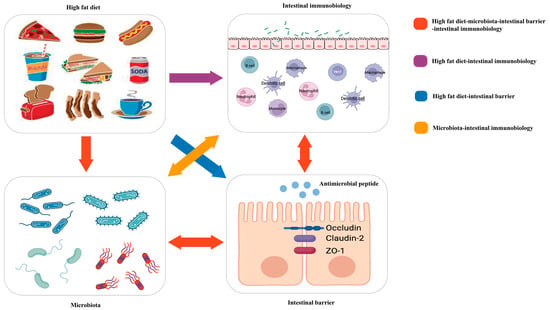
Figure 1. Red arrow: the high-fat diet shapes the gut microbiota, which changes the function of the intestinal barrier and further influences intestinal immunobiology. The intestinal immunobiology also affects the intestinal barrier and IECs, i.e., the components of the intestinal barrier, which also influence microbiota. Purple arrow: the high-fat diet modulates immune cell infiltration and polarization. Blue arrow: the high-fat diet influences the intestinal barrier. Orange arrow: gut microbiota interacts with intestinal immunobiology.
Researchers will focus on the critical roles of a high-fat diet (HFD) on intestinal immunity and gut microbiota and the impacts of the altered intestinal microecological imbalance on intestinal immunity in IBD, aiming to offer a direction for the pathogenesis of IBD (Figure 2).
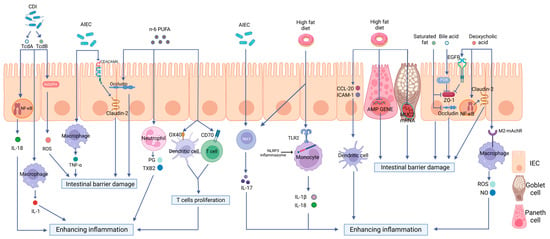
Figure 2. The effects of a high-fat diet on intestinal immunity in IBD. The specific manifestations are as follows: (1) Intestinal barrier dysfunction. A high-fat diet (HFD) disrupts the intestinal tight junction (TJ) structure and reduces Mucin 2 abundance and antimicrobial peptide (AMP) secretion. (2) Dysregulated PRR activation. HFD activates Toll-like receptor 2(TLR2) and consequently activates the NLRP3 inflammasome and promotes the release of inflammatory mediators, such as interleukin-18 (IL-18) and interleukin-1 beta (IL-1β), through monocytes to enhance intestinal inflammation. (3) The disordered function of immune cells. HFD can increase the production of OX40 and CD70 in both DCs and T cells, therefore inducing T cell proliferation and causing a proinflammatory effect. HFD can also stimulate the maturation of DCs, the polarization of Th17 cells, neutrophil migration, and the release of inflammatory mediators. (4) Intestinal dysbiosis. HFD can increase the abundance rates of AIEC and Clostridioides difficile, causing intestinal barrier disruption and enhancing intestinal inflammation via multiple mechanisms.
2. High-Fat Diet and the Intestinal Barrier in IBD
Intestinal epithelial cells (IECs) and tight junctions (TJs) constitute the epithelial barrier of intestinal immunity; its integrity is the precondition for intestinal defense [32]. Mucosal defense, as the front of the epithelial barrier, including immune molecules and mucus proteins, represents the most prominent interaction zone between the microbiota and host [33]. The receptors expressed in the intestinal epithelial cells also play vital roles in the constant communication of gut microflora and immune cells aggregated in the mucosal epithelium or submucosal lamina propria. Various studies have shown that an abnormal intestinal barrier function is crucial to the pathogenesis of IBD [34,35,36]. Moreover, HFD was shown to participate in intestinal inflammatory responses by affecting the intestinal barrier function [37] (Figure 2).
3. High-Fat Diet and Pattern Recognition Receptors in IBD
Pattern recognition receptors (PRRs) are immune sensors that recognize pathogen-associated molecular patterns (PAMPs) inside and outside the cells. Many PRRs, such as Toll-like receptors (TLRs) and NOD-like receptors (NLRs) and the molecules interacting with them, have been identified and characterized. PRRs are essential in the detection and elimination of pathogens. However, dysregulated PRR activation can lead to inflammatory diseases. It has been shown by increasing evidence that innate immune dysfunction, which is mediated by TLRs and NLRP3, plays a crucial role in the pathogenesis of IBD [65,66]. Previous research has shown that PRR-mediated inflammation, which is caused by an HFD, plays a notable role in intestinal inflammation [67,68,69,70,71,72] (Figure 3).
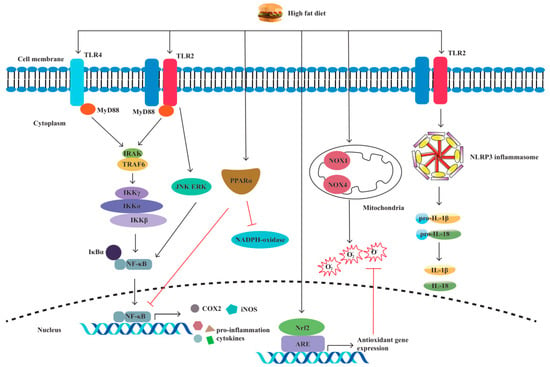
Figure 3. A high-fat diet regulates proinflammatory factors and oxidative stress through TLRs and NLRP. The specific manifestations are as follows: (1) Through the TLR4/NF−κB/MyD88 pathway, a high-fat diet (HFD) causes intestinal inflammation by elevating cytokine levels and alleviating cellular oxidative stress. (2) HFD activates oxidative stress markers nicotinamide adenine dinucleotide phosphate (NADPH), NADPH oxidase 4 (NOX4), and NOX1. (3) HFD increases the production of inducible nitric oxide synthase (iNOS) and cyclooxygenase-2 (COX-2). (4) HFD activates TLR2, resulting in M1 macrophage polarization and proinflammatory cytokine production. (5) HFD induces NLRP3 expression and promotes pro-IL-1β and IL-1β secretion by activating TLR2.
4. High-Fat Diet and Immune Cells in IBD
The disordered function and the number of adaptive immune cells, especially T lymphocytes, are crucial to IBD etiology [91,92,93,94] (Figure 2). A regulatory role of HFD in adaptive immune cells was also demonstrated in HFD-fed DSS-induced colitis mice; increased non-CD1d-restricted NKT cells and decreased Tregs were observed in the colon. This is paralleled by the fact that a higher ratio of effector T cells/regulatory T cells will contribute to the inflammatory state in the intestine [95]. Moreover, HFD can disrupt the steady state of intraepithelial lymphocytes (IELs), reducing homeostatic proliferation in intraepithelial T lymphocytes and the expression of CD103 and CCR9 on these cells to worsen the outcome of DSS-induced colitis in mice [96]. Similarly, HFD-fed mice substantially increased Th17 polarization [97] and CD3+ T cell infiltration in the gut [98], resulting in colitis aggravation. HFD-produced peroxidized lipids, such as 13-HPODE, could stimulate the secretion of pro-inflammatory granzymes by resident NK cells, thereby contributing to intestinal inflammation [99]. Previous studies of IBD suggest the involvement of innate lymphoid cells (ILCs) [100]. There was an increase in IL-17-producing type 3 innate lymphoid cells (ILC3s) in the offspring of mice that were fed a high-fat diet, leading to high susceptibility to inflammation [101]. In another animal study, significantly increased expression of caspase-3 was found in type 1 innate lymphoid cells (ILC1) and ILC3 in the mice fed with HFD as compared to the control group, possibly resulting in pro-apoptotic mechanisms [102]. In terms of B cells, in the plasma and spleen of C57BL/6 mice, the HFD induced evident decreases in the number of B cells, accompanied by oxidative stress and increased oxidative damage [103]. Gurzell et al. [104] found that docosahexaenoic acid (DHA), a type of n-3 polyunsaturated fatty acid that is low in Western diets, enhances B cell activation, thereby boosting the humoral immunity of mice, which may up-regulate the resolution phase of inflammation.
Furthermore, an increased presence of colonic macrophages has been shown in HFD-induced obese mice [105]. Still, they are deficient in forkhead box O3 (FOXO3) in macrophages [105], which mediates the proapoptotic or anti-inflammatory effects of macrophages [106]. Neutrophils, generally regarded as keys to inflammation, play a crucial role in intestinal inflammation in IBD [107]. Neutrophil migration is enhanced by an HFD due to the elevated expression of associated cytokines [108], such as monocyte chemoattractant protein-1 (MCP-1) [109] and chemokine (C-X-C motif) ligands 1 (CXCL1) and 2 (CXCL2), in the intestine of mice [110]. Yoshida et al. [111] found that the secretion of growth-regulated oncogene/cytokine-induced neutrophil chemoattractant-1 (GRO/CINC-1) could be increased by long-chain fatty acids in rat IECs.
In a mice model of Crohn’s disease-like ileitis, DCs recruited into the intestinal lamina propria also appear because of the enhanced levels of chemokine (C-C motif) ligand (CCL) 20 and intercellular cell adhesion molecule 1 (ICAM1) induced by the HFD [112]. Moreover, increased maturity markers of DCs were found in a DSS-induced colitis model that was fed an HFD, which exacerbated intestinal inflammation [71,113].
All these data illustrate that an HFD could influence intestinal immune cells and the humoral immune response to induce intestinal inflammation, disrupt tissue structure, and exacerbate IBD conditions. More emphasis should be placed on the fact that some studies have concentrated on the changes in these cytokines and immune cells under an HFD but have not explored the alterations in intestinal microorganisms. Whether these immunity-related changes are just the results of this dietary model, the results of intestinal microorganisms, or both, is still obscure. Therefore, it is necessary to conduct these studies in germ-free mice, which may better elaborate on the direct effect of diet on intestinal immunity and help explain how environmental factors can increase susceptibility to IBD.
5. Polyunsaturated Fatty Acids (PUFAs) in IBD
Polyunsaturated fatty acids (PUFAs) are a type of fatty acid that contains more than two double bonds. PUFAs contain two principal families: n-6 (or omega-6) and n-3 (or omega-3). Eicosapentaenoic acid (EPA) and DHA are precursors of n-3 PUFAs and are classified as essential lipid mediators. The typical Western-style diet has a high n-6/n-3 ratio of approximately 10–15:1 [114]. The increase in dietary n-6/n-3 PUFAs was positively correlated with the increased incidence of IBD [115] (Figure 2). John et al. [116] suggested that increasing the consumption of n-3 PUFAs may help prevent UC. In addition, prospective research has revealed that increasing the proportion of n-3/n-6 PUFA ingestion can help to maintain IBD remission [117].
Beguin et al. [118] showed that 150 mM of DHA could increase ZO-1 intensity in vitro. A lower intensity of occludin, when incubated with n-6 PUFAs, was also found in this research. Previous research has shown that TLR-2 gene expression in TNBS-induced colitis may be promoted by n-3 PUFAs [119]. The effect of n-3 PUFAs on neutrophils in the inflammatory process has also been investigated in TNBS mice in vivo; DHA and EPA could inhibit PMN transepithelial migration by reducing VCAM-1 and ICAM-1 [119]. Studies have revealed that the serum level of leukotriene B4 (LTB4) secreted by neutrophils in UC patients could be reduced by n-3 PUFAs and that the extravascular tissue damage caused by excessively activated neutrophils could also be avoided [120]. Current studies in mice show that n-3 polyunsaturated fatty acids could reduce the antigen-presenting function of DCs by inhibiting the expression of CD69 and CTLA-4 on T lymphocytes [121,122]. The metabolites of linoleic acid (LA, n-6 PUFAs) and arachidonic acid (AA, n-6) can produce thromboxane B2 (TXB2) and 4-series leukotrienes (LTS) through the cyclooxygenase (COX) pathway [123]. Additionally, n-6 PUFAs could also promote the production of PGE2 in vitro, thereby increasing the production of costimulatory molecules, including OX40 and CD70 in both DCs and T cells; this could induce T-cell proliferation and cause proinflammatory effects [124,125]. Moreover, the role of n-3 PUFAs in distinct types of enteritis models seems to differ. In the chronic model of intestinal inflammation, higher levels of suppressive cytokines are expressed by Th17 cells in the colon of mice than in the spleen. At the same time, there was no difference in the acute model [126,127]. Therefore, the relationship between PUFAs and T cells, especially Th17 cells in IBD, requires further study.
6. Short Chain Fatty Acids (SCFAs) in IBD
SCFAs are the products of anaerobic fermentation of dietary fiber, primarily containing acetate, propionate, and butyrate [8,128]. Nowadays, the beneficial roles of SCFAs on intestinal barrier integrity and immune cell functions in IBD have been highlighted by increasing evidence. Zheng et al. [129] revealed that claudin-2 formation is negatively regulated by butyrate via upregulating IL-10RA expression to protect gut barrier function, which was related to the signal transducing activator of transcription 3 (STAT3)-Histone Deacetylase inhibition (HDACi) pathway. Moreover, Hatayama et al. [130], who treated the human colon cancer cell line with butyrate and confirmed that SCFAs stimulates MUC2 production both in protein and mRNA levels, revealed that SCFAs increase MUC2 production.
The mechanism of butyrate stimulating AMP production has been investigated by Zhao et al. [131]. They used mammalian target of rapamycin (mTOR) siRNA and STAT3 siRNA to knockdown mTOR and STAT3, respectively, in intestinal epithelial cell (IEC) models and found that the mRNA and protein expressions of RegIIIγ and β-defensins were prominently impaired in these IECs, thus indicating that butyrate could active mTOR and STAT3 to promote AMP synthesis and confer resistance to colitis. The STAT3 and mTOR pathways have also been demonstrated to promote Th1 cells producing IL-10 by using butyrate to deal with the T cells from IBD patients and the DSS model, therefore limiting colitis [132]. Noteworthy, the role of SCFAs on T cells is related to the cytokine milieu. In the case of SCFA treatment, effector T cells, including Th1 and Th17 cells, are generated from naive T cells under a steady inflammatory condition, whereas in the active immune responses, the productions are regulatory T cells, such as IL-10+ T cells and FoxP3+ T cells [133]. Meanwhile, DC differentiation has also been reflected to be associated with mTOR and SATA3 pathways [134]. Butyrate, as a HDAC3 inhibitor, increases the antimicrobial functions of intestinal macrophages through a reduction in mTOR kinase activity [135] and downregulates macrophages secreting proinflammatory mediators [136]. The effect of SCFAs on neutrophils in the inflammatory process has also been investigated both in rats vivo and in vitro. On the one hand, SCFAs can promote neutrophils recruited into inflammatory sites by increasing L-selectin expression and chemokine release [137]. On the other hand, pro-inflammatory cytokines, TNF-α, and NO, produced by lipopolysaccharide (LPS)-stimulated neutrophils, are inhibited by SCFA treatment [138]. In view of the fact that mTOR is crucial in regulating the differentiation and function of innate and adaptive immune cells for intestinal immunity and that STAT3 has prominent aspects in the expressions of cytokines and chemokines, great insights must be explored about the interrelations between immune homeostasis and SCFAs in IBD.
7. High-Fat Diet and Intestinal Dysbacteriosis in IBD
It is well acknowledged that IBD is linked to compositional and metabolic alterations in intestinal microbiota. Fecal microbiota transplantation has been reported as a potential treatment of IBD [139,140]. Microbial communities can speedily and flexibly convert their components and functional repertoires following modern dietary challenges. Examples of this conversion could be supported by studies showing that a high HFD intake would increase the abundance rates of AIEC and Clostridioides difficile, decrease the abundance rates of Akkermansia muciniphila, and reduce the abundance rates of both Firmicutes and Bacteroidetes [141]. The clinical trial devised by Fritsch et al. [142] revealed that UC patients treated with a low-fat, high-fiber diet experienced a reduction in inflammation and an increase in the abundance of Bacteroidetes. Several studies have shown that these gut microbiotas and their metabolites are strongly correlated with IBD by potentially affecting intestinal immunity (Figure 2).
This entry is adapted from the peer-reviewed paper 10.3390/biom13060905
This entry is offline, you can click here to edit this entry!
