Reducing low-density lipoprotein cholesterol (LDL-C) levels is a key target for lowering cardiovascular risk and preventing atherosclerotic cardiovascular disease (ASCVD). Red yeast rice (RYR) is a nutraceutical widely used as a lipid-lowering dietary supplement. The main cholesterol-lowering components of RYR are monacolins, particularly monacolin K, which is structurally identical to lovastatin and targets the same key enzyme of cholesterol biosynthesis. RYR supplementation reduces LDL-C levels by approximately 15–34% versus placebo, with a similar effect to low-dose, first-generation statins in subjects with mild-to-moderate dyslipidemia.
- efficacy
- endothelial function
- inflammatory markers
1. Epidemiology and Natural History of Hypercholesterolemia and ASCVD
2. Purpose and Outcome of Treatment
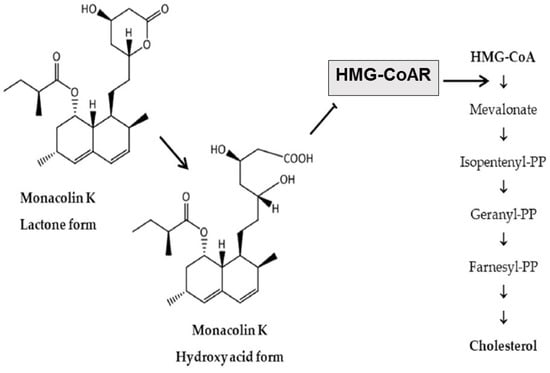
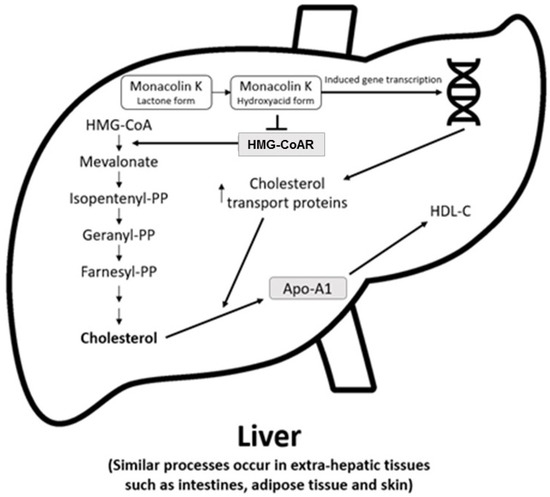
3. Metabolism of the Bioactive Components and Mechanism of Action of RYR
4. Effects of RYR on Lipids
4.1. RYR versus Placebo
4.2. RYR versus Other Statin Preparations
4.3. RYR versus Placebo and Other Statins Meta-Analyses
5. Effects of RYR on Inflammatory and Vascular Remodeling Biomarkers and Endothelial Function
6. Beneficial Effects of Exposure to RYR on ASCVD Risk and Events
6.1. RYR versus Placebo
6.2. RYR versus Other Statins
7. Beneficial Effects of RYR-Berberine Combinations
8. Convenience and Preference, and Health Economic Impact
This entry is adapted from the peer-reviewed paper 10.3390/nu15102288
References
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 9 August 2022).
- Cicero, A.F.G.; Colletti, A.; Bajraktari, G.; Descamps, O.; Djuric, D.M.; Ezhov, M.; Fras, Z.; Katsiki, N.; Langlois, M.; Latkovskis, G.; et al. Lipid lowering nutraceuticals in clinical practice: Position paper from an International Lipid Expert Panel. Arch. Med. Sci. 2017, 13, 965–1005.
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472.
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337.
- Carroll, M.D.; Fryar, C.D. Total and High-Density Lipoprotein Cholesterol in Adults: United States, 2015–2018. Centers for Disease Control and Prevention. 2020. Available online: https://www.cdc.gov/nchs/products/databriefs/db363.htm (accessed on 27 April 2023).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation 2020, 141, e139–e596.
- Lin, C.-F.; Chang, Y.-H.; Chien, S.-C.; Lin, Y.-H. Epidemiology of dyslipidemia in the Asia Pacific region. Int. J. Gerontol. 2018, 12, 2–6.
- Bilitou, A.; Were, J.; Farrer, A.; Rabe, A.; Ming, S.W.Y.; Haq, I.; Dunton, K. Prevalence and patient outcomes of adult primary hypercholesterolemia and dyslipidemia in the UK: Longitudinal retrospective study using a primary care dataset from 2009 to 2019. Clinicoecon. Outcomes Res. 2022, 14, 189–203.
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021.
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188.
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 2019, 139, e1082–e1143.
- Cholesterol Treatment Trialists’ (CTT) Collaboration; Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681.
- Ference, B.A.; Yoo, W.; Alesh, I.; Mahajan, N.; Mirowska, K.K.; Mewada, A.; Kahn, J.; Afonso, L.; Williams, K.A.; Flack, J.M. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: A mendelian randomization analysis. J. Am. Coll. Cardiol. 2012, 60, 2631–2639.
- Ference, B.A.; Majeed, F.; Penumetcha, R.; Flack, J.M.; Brook, R.D. Effect of naturally random allocation to lower low-density lipoprotein cholesterol on the risk of coronary heart disease mediated by polymorphisms in NPC1l1, HMGCR, or both: A 2 × 2 factorial Mendelian randomization study. J. Am. Coll. Cardiol. 2015, 65, 1552–1561.
- Penson, P.E.; Banach, M. Nutraceuticals for the control of dyslipidaemias in clinical practice. Nutrients 2021, 13, 2957.
- Banach, M.; Bruckert, E.; Descamps, O.S.; Ellegård, L.; Ezhov, M.; Föger, B.; Fras, Z.; Kovanen, P.T.; Latkovskis, G.; März, W.; et al. The role of red yeast rice (RYR) supplementation in plasma cholesterol control: A review and expert opinion. Atheroscler. Suppl. 2019, 39, e1–e8.
- Younes, M.; Aggett, P.; Aguilar, F.; Crebelli, R.; Dusemund, B.; Filipič, M.; Frutos, M.J.; Galtier, P.; Gott, D.; Gundert-Remy, U.; et al. Scientific opinion on the safety of monacolins in red yeast rice. EFSA J. 2018, 16, e05368.
- Song, J.; Luo, J.; Ma, Z.; Sun, Q.; Wu, C.; Li, X. Quality and authenticity control of functional red yeast rice-a review. Molecules 2019, 24, 1944.
- Cicero, A.F.G.; Fogacci, F.; Zambon, A. Red yeast rice for hypercholesterolemia: JACC focus seminar. J. Am. Coll. Cardiol. 2021, 77, 620–628.
- Mannino, G.; Iovino, P.; Lauria, A.; Genova, T.; Asteggiano, A.; Notarbartolo, M.; Porcu, A.; Serio, G.; Chinigò, G.; Occhipinti, A.; et al. Bioactive triterpenes of protium heptaphyllum gum resin extract display cholesterol-lowering potential. Int. J. Mol. Sci. 2021, 22, 2664.
- Martin, G.; Duez, H.; Blanquart, C.; Berezowski, V.; Poulain, P.; Fruchart, J.C.; Najib-Fruchart, J.; Glineur, C.; Staels, B. Statin-induced inhibition of the Rho-signaling pathway activates PPARalpha and induces HDL apoA-I. J. Clin. Investig. 2001, 107, 1423–1432.
- Bjarnadottir, O.; Kimbung, S.; Johansson, I.; Veerla, S.; Jonsson, M.; Bendahl, P.O.; Grabau, D.; Hedenfalk, I.; Borgquist, S. Global transcriptional changes following statin treatment in breast cancer. Clin. Cancer. Res. 2015, 21, 3402–3411.
- Dichtl, W.; Dulak, J.; Frick, M.; Alber, H.F.; Schwarzacher, S.P.; Ares, M.P.; Nilsson, J.; Pachinger, O.; Weidinger, F. HMG-CoA reductase inhibitors regulate inflammatory transcription factors in human endothelial and vascular smooth muscle cells. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 58–63.
- Ahmadi, Y.; Ghorbanihaghjo, A.; Argani, H. The effect of statins on the organs: Similar or contradictory? J. Cardiovasc. Thorac. Res. 2017, 9, 64–70.
- Chen, C.H.; Uang, Y.S.; Wang, S.T.; Yang, J.C.; Lin, C.J. Interaction between red yeast rice and CYP450 enzymes/P-glycoprotein and its implication for the clinical pharmacokinetics of lovastatin. Evid. Based Complement. Altern. Med. 2012, 2012, 127043.
- Li, Z.; Seeram, N.P.; Lee, R.; Thames, G.; Minutti, C.; Wang, H.J.; Heber, D. Plasma clearance of lovastatin versus Chinese red yeast rice in healthy volunteers. J. Altern. Complement. Med. 2005, 11, 1031–1038.
- Cohen, P.A.; Avula, B.; Khan, I.A. Variability in strength of red yeast rice supplements purchased from mainstream retailers. Eur. J. Prev. Cardiol. 2017, 24, 1431–1434.
- Gordon, R.Y.; Cooperman, T.; Obermeyer, W.; Becker, D.J. Marked variability of monacolin levels in commercial red yeast rice products: Buyer beware! Arch. Intern. Med. 2010, 170, 1722–1727.
- Marcheluzzo, S.; Faggian, M.; Zancato, M.; Peron, G. Analysis of monacolins and berberine in food supplements for lipid control: An overview of products sold on the Italian market. Molecules 2021, 26, 2222.
- Zhu, B.; Qi, F.; Wu, J.; Yin, G.; Hua, J.; Zhang, Q.; Qin, L. Red yeast rice: A systematic review of the traditional uses, chemistry, pharmacology, and quality control of an important Chinese folk medicine. Front. Pharmacol. 2019, 10, 1449.
- Tomlinson, B.; Chan, P.; Liu, Z.M. Statin intolerance-an Asian perspective. J. Atheroscler. Thromb. 2020, 27, 485–488.
- Lee, E.; Ryan, S.; Birmingham, B.; Zalikowski, J.; March, R.; Ambrose, H.; Moore, R.; Lee, C.; Chen, Y.; Schneck, D. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin. Pharmacol. Ther. 2005, 78, 330–341.
- Gandelman, K.; Fung, G.L.; Messig, M.; Laskey, R. Systemic exposure to atorvastatin between Asian and Caucasian subjects: A combined analysis of 22 studies. Am. J. Ther. 2012, 19, 164–173.
- Heber, D.; Yip, I.; Ashley, J.M.; Elashoff, D.A.; Elashoff, R.M.; Go, V.L. Cholesterol-lowering effects of a proprietary Chinese red-yeast-rice dietary supplement. Am. J. Clin. Nutr. 1999, 69, 231–236.
- Zhao, S.-P.; Liu, L.; Cheng, Y.-C.; Li, Y.-L. Effect of xuezhikang, a cholestin extract, on reflecting postprandial triglyceridemia after a high-fat meal in patients with coronary heart disease. Atherosclerosis 2003, 168, 375–380.
- Zhao, S.P.; Liu, L.; Cheng, Y.C.; Shishehbor, M.H.; Liu, M.H.; Peng, D.Q.; Li, Y.L. Xuezhikang, an extract of cholestin, protects endothelial function through antiinflammatory and lipid-lowering mechanisms in patients with coronary heart disease. Circulation 2004, 110, 915–920.
- Lin, C.-C.; Li, T.-C.; Lai, M.-M. Efficacy and safety of monascus purpureus went rice in subjects with hyperlipidemia. Eur. J. Endocrinol. 2005, 153, 679–686.
- Becker, D.J.; Gordon, R.Y.; Halbert, S.C.; French, B.; Morris, P.B.; Rader, D.J. Red yeast rice for dyslipidemia in statin-intolerant patients: A randomized trial. Ann. Intern. Med. 2009, 150, 830–839.
- Bogsrud, M.P.; Ose, L.; Langslet, G.; Ottestad, I.; Strøm, E.C.; Hagve, T.A.; Retterstøl, K. HypoCol (red yeast rice) lowers plasma cholesterol—A randomized placebo controlled study. Scand. Cardiovasc. J. 2010, 44, 197–200.
- Cicero, A.F.; Derosa, G.; Parini, A.; Maffioli, P.; D’Addato, S.; Reggi, A.; Giovannini, M.; Borghi, C. Red yeast rice improves lipid pattern, high-sensitivity C-reactive protein, and vascular remodeling parameters in moderately hypercholesterolemic Italian subjects. Nutr. Res. 2013, 33, 622–628.
- Verhoeven, V.; Lopez Hartmann, M.; Remmen, R.; Wens, J.; Apers, S.; Van Royen, P. Red yeast rice lowers cholesterol in physicians—A double blind, placebo controlled randomized trial. BMC Complement. Altern. Med. 2013, 13, 178.
- Moriarty, P.M.; Roth, E.M.; Karns, A.; Ye, P.; Zhao, S.P.; Liao, Y.; Capuzzi, D.M.; Bays, H.E.; Zhang, F.; Liu, S.; et al. Effects of Xuezhikang in patients with dyslipidemia: A multicenter, randomized, placebo-controlled study. J. Clin. Lipidol. 2014, 8, 568–575.
- Heinz, T.; Schuchardt, J.P.; Möller, K.; Hadji, P.; Hahn, A. Low daily dose of 3 mg monacolin K from RYR reduces the concentration of LDL-C in a randomized, placebo-controlled intervention. Nutr. Res. 2016, 36, 1162–1170.
- Wang, T.J.; Lien, A.S.; Chen, J.L.; Lin, C.H.; Yang, Y.S.; Yang, S.H. A randomized clinical efficacy trial of red yeast rice (monascus pilosus) against hyperlipidemia. Am. J. Chin. Med. 2019, 47, 323–335.
- Minamizuka, T.; Koshizaka, M.; Shoji, M.; Yamaga, M.; Hayashi, A.; Ide, K.; Ide, S.; Kitamoto, T.; Sakamoto, K.; Hattori, A.; et al. Low dose red yeast rice with monacolin K lowers LDL cholesterol and blood pressure in japanese with mild dyslipidemia: A multicenter, randomized trial. Asia Pac. J. Clin. Nutr. 2021, 30, 424–435.
- Kou, W.; Lu, Z.; Guo, J. Effect of xuezhikang on the treatment of primary hyperlipidemia. Zhonghua Nei Ke Za Zhi 1997, 36, 529–531.
- Chen, L.L.; Liu, J. The effects of Xuezhikang on hypercholesterolemia. Her. Med. 2002, 21, 31–32.
- Cui, F.; Zhang, Y.; Wei, Q.; Liu, C.; Wang, J.; Zhang, M. A novel medical treatment for lipid control in patients with unstable angina pectoris and statin-induced liver dysfunction. Acta Cardiol. Sin. 2015, 31, 66–71.
- Ruscica, M.; Gomaraschi, M.; Mombelli, G.; Macchi, C.; Bosisio, R.; Pazzucconi, F.; Pavanello, C.; Calabresi, L.; Arnoldi, A.; Sirtori, C.R.; et al. Nutraceutical approach to moderate cardiometabolic risk: Results of a randomized, double-blind and crossover study with armolipid plus. J. Clin. Lipidol. 2014, 8, 61–68.
- Marazzi, G.; Campolongo, G.; Pelliccia, F.; Quattrino, S.; Vitale, C.; Cacciotti, L.; Massaro, R.; Volterrani, M.; Rosano, G. Comparison of low-dose statin versus low-dose statin + armolipid plus in high-intensity statin-intolerant patients with a previous coronary event and percutaneous coronary intervention (ADHERENCE trial). Am. J. Cardiol. 2017, 120, 893–897.
- Gheith, O.; Sheashaa, H.; Abdelsalam, M.; Shoeir, Z.; Sobh, M. Efficacy and safety of monascus purpureus went rice in subjects with secondary hyperlipidemia. Clin. Exp. Nephrol. 2008, 12, 189–194.
- Shang, X. Clinical observation of xuezhikang and atorvastatin on dyslipidemia and hemorheology in patients with coronary heart disease. Guangxi Med. 2007, 8, 1158–1159.
- Halbert, S.C.; French, B.; Gordon, R.Y.; Farrar, J.T.; Schmitz, K.; Morris, P.B.; Thompson, P.D.; Rader, D.J.; Becker, D.J. Tolerability of red yeast rice (2400 mg twice daily) versus pravastatin (20 mg twice daily) in patients with previous statin intolerance. Am. J. Cardiol. 2010, 105, 198–204.
- Xue, Y.; Tao, L.; Wu, S.; Wang, G.; Qian, L.; Li, J.; Liao, L.; Tang, J.; Ji, K. Red yeast rice induces less muscle fatigue symptom than simvastatin in dyslipidemic patients: A single center randomized pilot trial. BMC Cardiovasc. Disord. 2017, 17, 127.
- Li, B.; Hu, S.-Y.; Wu, X.; Xu, H.-L.; Zhang, H.-M.; Wang, L. Anti-oxidant and anti-inflammatory effects of xuezhikang capsule on patients with coronary heart diseases. Prog. Mod. Biomed. 2011, 12, 2289–2291.
- Liu, L.T.; Wu, M.; Wang, H.X. Clinical study on the treatment of abnormal blood lipids complicated with carotid atherosclerosis with lipid-reducing red rice minute powder: A randomized controlled trial. Zhongguo Zhong Xi Yi Jie He Za Zhi 2011, 31, 1196–1200.
- Li, P.; Wang, Q.; Chen, K.; Zou, S.; Shu, S.; Lu, C.; Wang, S.; Jiang, Y.; Fan, C.; Luo, Y. Red yeast rice for hyperlipidemia: A meta-analysis of 15 high-quality randomized controlled trials. Front. Pharmacol. 2021, 12, 819482.
- Gerards, M.C.; Terlou, R.J.; Yu, H.; Koks, C.H.; Gerdes, V.E. Traditional Chinese lipid-lowering agent red yeast rice results in significant LDL reduction but safety is uncertain—A systematic review and meta-analysis. Atherosclerosis 2015, 240, 415–423.
- Xu, G.; Lin, M.; Dai, X.; Hu, J. Comparing the effectiveness of Chinese patent medicines containing red yeast rice on hyperlipidaemia: A network meta-analysis of randomized controlled trials. Endocrinol. Diabetes Metab. 2022, 5, e00314.
- Kandelouei, T.; Abbasifard, M.; Imani, D.; Aslani, S.; Razi, B.; Fasihi, M.; Shafiekhani, S.; Mohammadi, K.; Jamialahmadi, T.; Reiner, Z.; et al. Effect of statins on serum level of hs-CRP and CRP in patients with cardiovascular diseases: A systematic review and meta-analysis of randomized controlled trials. Mediat. Inflamm. 2022, 2022, 8732360.
- Lu, Z.; Kou, W.; Du, B.; Wu, Y.; Zhao, S.; Brusco, O.A.; Morgan, J.M.; Capuzzi, D.M.; Li, S. Effect of Xuezhikang, an extract from red yeast Chinese rice, on coronary events in a Chinese population with previous myocardial infarction. Am. J. Cardiol. 2008, 101, 1689–1693.
- Li, J.J.; Lu, Z.L.; Kou, W.R.; Chen, Z.; Wu, Y.F.; Yu, X.H.; Zhao, Y.C. Impact of Xuezhikang on coronary events in hypertensive patients with previous myocardial infarction from the China Coronary Secondary Prevention Study (CCSPS). Ann. Med. 2010, 42, 231–240.
- Li, J.J.; Lu, Z.L.; Kou, W.R.; Chen, Z.; Wu, Y.F.; Yu, X.H.; Zhao, Y.C. Beneficial impact of Xuezhikang on cardiovascular events and mortality in elderly hypertensive patients with previous myocardial infarction from the China Coronary Secondary Prevention Study (CCSPS). J. Clin. Pharmacol. 2009, 49, 947–956.
- Sungthong, B.; Yoothaekool, C.; Promphamorn, S.; Phimarn, W. Efficacy of red yeast rice extract on myocardial infarction patients with borderline hypercholesterolemia: A meta-analysis of randomized controlled trials. Sci. Rep. 2020, 10, 2769.
- Yuan, R.; Yuan, Y.; Wang, L.; Xin, Q.; Wang, Y.; Shi, W.; Miao, Y.; Leng, S.X.; Chen, K.; Cong, W. Red yeast rice preparations reduce mortality, major cardiovascular adverse events, and risk factors for metabolic syndrome: A systematic review and meta-analysis. Front. Pharmacol. 2022, 13, 744928.
- Chang, C.-C.; Sun, M.-F.; Chou, Y.-C.; Yeh, C.-C.; Hu, C.-J.; Cherng, Y.-G.; Chen, T.-L.; Liao, C.-C. Decreased risk of stroke in people using red yeast rice prescriptions (LipoCol Forte®): A total population-based retrospective cohort study. Evid. Based Complement. Altern. Med. 2022, 2022, 8160425.
- Banach, M.; Katsiki, N.; Latkovskis, G.; Rizzo, M.; Pella, D.; Penson, P.E.; Reiner, Z.; Cicero, A.F.G. Postmarketing nutrivigilance safety profile: A line of dietary food supplements containing red yeast rice for dyslipidemia. Arch. Med. Sci. 2021, 17, 856–863.
- Cicero, A.F.G.; Kennedy, C.; Knežević, T.; Bove, M.; Georges, C.M.G.; Šatrauskienė, A.; Toth, P.P.; Fogacci, F. Efficacy and safety of armolipid plus®: An updated prisma compliant systematic review and meta-analysis of randomized controlled clinical trials. Nutrients 2021, 13, 638.
- Pirro, M.; Mannarino, M.R.; Bianconi, V.; Simental-Mendía, L.E.; Bagaglia, F.; Mannarino, E.; Sahebkar, A. The effects of a nutraceutical combination on plasma lipids and glucose: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2016, 110, 76–88.
- Castano, G.; Mas, R.; Fernandez, J.; Lopez, E.; Illnait, J.; Fernandez, L.; Mesa, M. Effects of policosanol on borderline to mildly elevated serum total cholesterol levels: A prospective, double-blind, placebo-controlled, parallel-group, comparative study. Curr. Ther. Res. Clin. Exp. 2003, 64, 522–537.
- Cicero, A.F.; Morbini, M.; Parini, A.; Urso, R.; Rosticci, M.; Grandi, E.; Borghi, C. Effect of red yeast rice combined with antioxidants on lipid pattern, hs-CRP level, and endothelial function in moderately hypercholesterolemic subjects. Ther. Clin. Risk Manag. 2016, 12, 281–286.
- Cicero, A.F.; Morbini, M.; Rosticci, M.; D’Addato, S.; Grandi, E.; Borghi, C. Middle-term dietary supplementation with red yeast rice plus Coenzyme Q10 improves lipid pattern, endothelial reactivity and arterial stiffness in moderately hypercholesterolemic subjects. Ann. Nutr. Metab. 2016, 68, 213–219.
- Baumgartner, S.; Bruckert, E.; Gallo, A.; Plat, J. The position of functional foods and supplements with a serum LDL-C lowering effect in the spectrum ranging from universal to care-related CVD risk management. Atherosclerosis 2020, 311, 116–123.
- Murphy, A.; Palafox, B.; O’Donnell, O.; Stuckler, D.; Perel, P.; AlHabib, K.F.; Avezum, A.; Bai, X.; Chifamba, J.; Chow, C.K.; et al. Inequalities in the use of secondary prevention of cardiovascular disease by socioeconomic status: Evidence from the PURE observational study. Lancet Glob. Health 2018, 6, e292–e301.
- Yusuf, S.; Islam, S.; Chow, C.K.; Rangarajan, S.; Dagenais, G.; Diaz, R.; Gupta, R.; Kelishadi, R.; Iqbal, R.; Avezum, A.; et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE study): A prospective epidemiological survey. Lancet 2011, 378, 1231–1243.
- Toth, P.P.; Patti, A.M.; Giglio, R.V.; Nikolic, D.; Castellino, G.; Rizzo, M.; Banach, M. Management of statin intolerance in 2018: Still more questions than answers. Am. J. Cardiovasc. Drugs 2018, 18, 157–173.
- Lopes, J.; Santos, P. Determinants of non-adherence to the medications for dyslipidemia: A systematic review. Patient Prefer. Adherence 2021, 15, 1853–1871.
- Cicero, A.F.; Derosa, G.; Parini, A.; Baronio, C.; Borghi, C. Factors associated with 2-year persistence in fully non reimbursed lipid-lowering treatments. Atherosclerosis 2014, 235, 81–83.
