Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
In 2016, the SOFA score was proposed as the main evaluation system for diagnosis in the definition of sepsis 3.0, and the SOFA score has become a new research focus in sepsis. Some people are skeptical about diagnosing sepsis using the SOFA score. Experts and scholars from different regions have proposed different, modified versions of SOFA score to make up for the related problems with the use of the SOFA score in the diagnosis of sepsis.
- sepsis
- SOFA score
- machine learning
1. Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. Sepsis is characterized by high morbidity, high mortality, and a high proportion of medical intervention [2][3]. According to the statistics, the incidence of sepsis has also significantly increased in recent years, with about 300 per 100,000 people diagnosed with sepsis, while 6% of hospitalized patients are diagnosed with sepsis [4][5]. Nearly $24 billion USD was spent on sepsis treatment in 2013, accounting for 13% of U.S. health spending [6][7]. Sepsis has become a major challenge in the field of emergency and critical medical care worldwide [8].
The standard nomenclature of sepsis began In 1991 [9]. The term sepsis is a broad term, and there is currently no single clinical standard or imaging or laboratory indicators that can be used to uniquely identify septic patients [10]. Therefore, the definition of sepsis continues to evolve and iterate. According to the third edition of the 2016 definition of sepsis, sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. Infection is especially emphasized as the starting point of sepsis, rather than a single pathogen invading the body, and organ failure is regarded as an important sign for the diagnosis of sepsis. This is similar to the definition of severe sepsis in sepsis 1.0/2.0, and the definition of severe sepsis has been removed from sepsis 3.0 [9][11]. The diagnosis scale of sepsis changed from SIRS score to ∆SOFA ≥ 2 (Figure 1). It should be noted that, in the diagnosis of sepsis, although the SIRS score has been replaced by the SOFA score, it still has widespread clinical uses, assisting in determining the degree of infection in patients and predicting the onset of sepsis [12][13]. With the introduction of the third version of the definition of sepsis, people’s understanding of sepsis has become clearer. At the same time, the diagnosis of organ dysfunction is added to the definition of sepsis, indicating that the pathological process of sepsis and the related verification response are more complex [14]. The SOFA score citation plays a very important role in the diagnosis of sepsis. Experts believe that sepsis requires a higher level of detection and intervention, and the inclusion of the SOFA score is more convenient for the clinical diagnosis of sepsis while unifying the conceptual differences in the incidence of sepsis, which is conducive to the follow-up development and promotion of sepsis-related research [15].
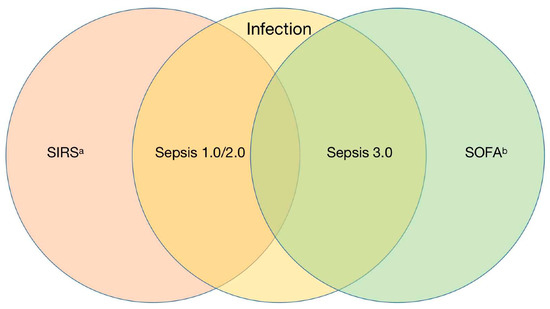
Figure 1. Comparison of new and old diagnosis criteria of sepsis. Abbreviations: SIRS, Systemic Inflammatory Response Syndrome; SOFA, Sequential Organ Failure Assessment. a Inflammatory response caused by pancreatitis, trauma, burns, etc. b Sepsis-related SOFA score, life-threatening organ dysfunction caused by dysregulated host response.
With the popularization of SOFA score, people have gradually found that the SOFA score has some problems in the diagnosis of sepsis, such as delays in diagnosis, lack of sensitivity, and a complex evaluation [16][17][18]. In view of the above problems, different studies have been carried out regarding the application of the SOFA score to diagnose sepsis. On the one hand, the concept of sepsis is extended, in which many emergency critical field experts, led by Dr. Wang, put forward the concept of preventing and blocking sepsis [19], while some scholars believe that patients who survive sepsis have serious cognitive, mental, and physical disorders, and they put forward the concept of post-sepsis syndrome [20]. Countries have also tried different ways of modifying and optimizing the SOFA score according to their own national conditions.
2. The Proposal of the SOFA Score
In the 1980s, people found that severe host response disorder infections can lead to multiple organ failure (MOF), which greatly increases the mortality of critically ill patients [21]. With increases in the understanding of organ function, and to describe the MOF degree of patients as objectively and quantitatively as possible, the European Association of critical Care Medicine formally formulated the SOFA score in Paris in 1994 [22]. The expert group believes that the original intention of establishing the SOFA score was to evaluate organ function damage through a limited number of simple and objective indicators, all of which should be easy to measure in hospitals at all levels and should not exceed the scope of routine testing in the intensive care unit [22]. It is worth mentioning that the expert group agreed that intestinal tissue is the first organ to suffer from functional damage caused by infection, and because intestinal function is too complex and there are no readily available and reliable specific indicators, intestinal function was not included in the evaluation system of SOFA score. This problem has been left until now [23]. The proposal of SOFA score provides a very reliable clinical guidance method to reasonably quantify the degree of organ dysfunction. On this basis, people gradually improve their awareness of multiple organ dysfunction, which provides a favorable reference scheme for clinical diagnosis and treatment. In the continuous development of modern medicine, the SOFA score has always been a recognized and reliable evaluation system in critical medicine [24]. The third edition of sepsis guidelines in 2016 regards SOFA scores as the main evaluation system for the diagnosis of sepsis. SOFA score is no longer limited to applications to the critical care system, but has become a research hot spot in emergency and critical areas and has received more and more attention [25]. With the expansion of the scope of application of SOFA score, it was also found to have many shortcomings, and many related studies on modified SOFA score have been carried out. Different countries and institutions have put forward many new ideas for the SOFA score, but these ideas have not yet been agreed on and are still at the verification stage. Researchers will describe the current modifications to the SOFA score in detail in the following pages.
3. Modification of SOFA Score (Related to Sepsis)
Researchers stated that SOFA score has been a routine method to evaluate the prognosis of patients with multiple organ dysfunction since it was proposed in 1996 [22]. However, there have always been voices challenging the SOFA score; for example, in 2010, the American Medical Association considered it impractical to collect four laboratory parameters in the SOFA score in the event of a massive influx of critically ill patients in an influenza pandemic, natural disasters, or some manmade disasters. Therefore, the laboratory parameters in the SOFA score were cut to a certain extent, and the score was named mSOFAa [26]. However, this modification has not been widely promoted. On the one hand, the purpose of this modification is to deal with sudden public health events and quickly judge the severity of the disease. On the other hand, this scoring system will overlook some critically ill patients who cannot be judged by routine vital signs. After the announcement of new sepsis guidelines in 2016, medical staff in various countries not only adapted and accepted the corresponding new definition of sepsis, but also began to modify the SOFA score for the diagnosis of sepsis. The first station for most patients with sepsis is the emergency room, where the flow of people is large, and monitoring measures are limited. To screen and to identify patients in the emergency room more quickly and to provide timely and positive detection and treatment to patients with risk factors, the SOFA score must urgently be modified. In the nearly six years that have passed since sepsis 3.0 was put forward, countries such as the United States, Australia, Republic of Korea, France, and Spain have successively proposed modified versions of the SOFA score according to national conditions [27][28][29][30][31]. At the same time, different degrees of improvement tests were carried out according to the low sensitivity of the qSOFA score in the rapid diagnosis of disease.
This entry is adapted from the peer-reviewed paper 10.3390/jcm12103493
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810.
- Iwashyna, T.J.; Ely, E.W.; Smith, D.M.; Langa, K.M. Long-term Cognitive Impairment and Functional Disability Among Survivors of Severe Sepsis. JAMA 2010, 304, 1787–1794.
- Xie, J.; Wang, H.; Kang, Y.; Zhou, L.; Liu, Z.; Qin, B.; Ma, X.; Cao, X.; Chen, D.; Lu, W.; et al. The Epidemiology of Sepsis in Chinese ICUs. Crit. Care Med. 2020, 48, e209–e218.
- Fleischmann, M.C.; Scherag, A.; Adhikari, N.K.J.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K.; International Forum of Acute Care Trialists. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272.
- Moss, M. Epidemiology of Sepsis: Race, Sex, and Chronic Alcohol Abuse. Clin. Infect. Dis. 2005, 41, S490–S497.
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211.
- Rhee, C.; Dantes, R.; Epstein, L.; Murphy, D.J.; Seymour, C.W.; Iwashyna, T.J.; Kadri, S.S.; Angus, D.C.; Danner, R.L.; Fiore, A.E.; et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009–2014. JAMA 2017, 318, 1241–1249.
- Reinhart, K.; Daniels, R.; Kissoon, N.; Machado, F.R.; Schachter, R.D.; Finfer, S. Recognizing Sepsis as a Global Health Priority—A WHO Resolution. N. Engl. J. Med. 2017, 377, 414–417.
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.H.; Sibbald, W.J. Definitions for Sepsis and Organ Failure and Guidelines for the Use of Innovative Therapies in Sepsis. Chest 1992, 101, 1644–1655.
- Mileski, W.J. Sepsis: What It Is and How to Recognize It. Surg. Clin. N. Am. 1991, 71, 749–764.
- Levy, M.M.; Fink, M.P.; Marshall, J.C.; Abraham, E.; Angus, D.; Cook, D.; Cohen, J.; Opal, S.M.; Vincent, J.-L.; Ramsay, G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003, 29, 530–538.
- Usman, O.A.; Usman, A.A.; Ward, M.A. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am. J. Emerg. Med. 2019, 37, 1490–1497.
- Jaramillo-Bustamante, J.C.; Piñeres-Olave, B.E.; González-Dambrauskas, S. SIRS o no SIRS: ¿es esa la infección? Una revisión crítica de los criterios de definición de sepsis. Bol. Med. Hosp. Infant. Mex. 2020, 77, 293–302.
- Esposito, S.; De Simone, G.; Boccia, G.; De Caro, F.; Pagliano, P. Sepsis and septic shock: New definitions, new diagnostic and therapeutic approaches. J. Glob. Antimicrob. Resist. 2017, 10, 204–212.
- Shankar-Hari, M.; Phillips, G.S.; Levy, M.L.; Seymour, C.W.; Liu, V.X.; Deutschman, C.S.; Angus, D.C.; Rubenfeld, G.D.; Singer, M.; for the Sepsis Definitions Task Force. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 775–787.
- Moreno, R.; Vincent, J.-L.; Matos, R.; Mendonça, A.; Cantraine, F.; Thijs, L.; Takala, J.; Sprung, C.; Antonelli, M.; Bruining, H.; et al. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Intensive Care Med. 1999, 25, 686–696.
- Ferreira, F.L.; Bota, D.P.; Bross, A.; Mélot, C.; Vincent, J.-L. Serial Evaluation of the SOFA Score to Predict Outcome in Critically Ill Patients. JAMA 2001, 286, 1754–1758.
- Verdonk, F.; Blet, A.; Mebazaa, A. The new sepsis definition. Curr. Opin. Anaesthesiol. 2017, 30, 200–204.
- Emergency Medicine Branch of Chinese Medical Care International Exchange Promotion Association; Emergency Medical Branch of Chinese Medical Association; Chinese Medical Doctor Association Emergency Medical Brabch; Chinese People’s Liberation Army Emergency Medicine Professional Committee. Consensus of Chinese Experts on Early Prevention and Blocking of Sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2020, 32, 518–530.
- Mostel, Z.; Perl, A.; Marck, M.; Mehdi, S.F.; Lowell, B.; Bathija, S.; Santosh, R.; Pavlov, V.A.; Chavan, S.S.; Roth, J. Post-sepsis syndrome—An evolving entity that afflicts survivors of sepsis. Mol. Med. 2019, 26, 6.
- Fry, D.E.; Pearlstein, L.; Fulton, R.L.; Polk, H.C. Multiple System Organ Failure. Arch. Surg. 1980, 115, 136–140.
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710.
- Arts, D.G.T.; de Keizer, N.F.; Vroom, M.B.; de Jonge, E. Reliability and accuracy of Sequential Organ Failure Assessment (SOFA) scoring. Crit. Care Med. 2005, 33, 1988–1993.
- Lambden, S.; Laterre, P.F.; Levy, M.M.; Francois, B. The SOFA score—Development, utility and challenges of accurate assessment in clinical trials. Crit. Care 2019, 23, 374.
- Bin Abdullah, S.O.; Sørensen, R.H.; Nielsen, F.E. Prognostic Accuracy of SOFA, qSOFA, and SIRS for Mortality Among Emergency Department Patients with Infections. Infect. Drug Resist. 2021, 14, 2763–2775.
- Grissom, C.K.; Brown, S.M.; Kuttler, K.G.; Boltax, J.P.; Jones, J.; Jephson, A.R.; Orme, J.F., Jr. A Modified Sequential Organ Failure Assessment Score for Critical Care Triage. Disaster Med. Public Health Prep. 2010, 4, 277–284.
- Rhee, C.; Zhang, Z.; Kadri, S.S.; Murphy, D.J.; Martin, G.; Overton, E.; Seymour, C.W.; Angus, D.C.; Dantes, R.; Epstein, L.; et al. Sepsis Surveillance Using Adult Sepsis Events Simplified eSOFA Criteria Versus Sepsis-3 Sequential Organ Failure Assessment Criteria. Crit. Care Med. 2019, 47, 307–314.
- Raymond, N.J.; Nguyen, M.; Allmark, S.; Woods, L.; Peckler, B. Modified Sequential Organ Failure Assessment sepsis score in an emergency department setting: Retrospective assessment of prognostic value. Emerg. Med. Australas. 2019, 31, 339–346.
- Lee, J.; Song, J.-U. Performance of a quick sofa-65 score as a rapid sepsis screening tool during initial emergency department assessment: A propensity score matching study. J. Crit. Care 2020, 55, 1–8.
- Vacheron, C.-H.; Friggeri, A.; Iwaz, J.; Allaouchiche, B.; Bohe, J.; Monneret, G.; Venet, F.; Cour, M.; Argaud, L.; Aubrun, F.; et al. A new simplified and accurate sa-SOFA score. J. Crit. Care 2020, 57, 240–245.
- Martín-Rodríguez, F.; Sanz-García, A.; Vegas, C.D.P.; Ortega, G.J.; Villamor, M.A.C.; López-Izquierdo, R. Time for a prehospital-modified sequential organ failure assessment score: An ambulance—Based cohort study. Am. J. Emerg. Med. 2021, 49, 331–337.
This entry is offline, you can click here to edit this entry!
