The spontaneous evolution of colorectal cancer is always burdened by complications. The most common complication is low bowel obstruction, found in approximately 20% of the cases of colorectal cancer, and it can occur either relatively abruptly, or is preceded by initially discrete premonitory symptoms, non-specific (until advanced evolutionary stages) and generally neglected or incorrectly interpreted. Success in the complex treatment of a low neoplastic obstruction is conditioned by a complete diagnosis, adequate pre-operative preparation, a surgical act adapted to the case (in one, two or three successive stages), and dynamic postoperative care. The moment of surgery should be chosen with great care and is the result of the experience of the anesthetic-surgical team. The operative act must be adapted to the case and has as its main objective the resolution of intestinal obstruction and only in a secondary way the resolution of the generating disease.
1. Introduction
Despite the improvement of early diagnosis methods for multiple pathological entities belonging to the digestive tract, bowel obstruction determined by multiple etiologies represents an important percentage of surgical emergencies, accounting for approximately 20–30% of the cases diagnosed with acute abdomen [
1]. Efforts made to identify and treat inflammatory diseases of the small intestine and colon, diagnosis of colic and rectal neoplasms in early stages, or the surgical resolution of parietal defects in uncomplicated stage have brought improvements regarding the precipitation of an obstructive episode of various etiologies [
2].
2. Development of the Obstructive Mechanism
The spontaneous evolution of colorectal cancer is always burdened by complications. Their variety is very large. Among the local complications, the most common are: loco-regional invasion with possible inter-visceral or external fistulas, tumor infection with adjacent sclerolipomatous reaction or abscesses, peritonitis by evacuation of tumor abscesses or intestinal perforations, intestinal obstructions, lower digestive bleeding, etc. General complications are represented by anemia, paraneoplastic venous thrombosis, multiple metastases, hepatic abscesses with systemic sepsis, etc. [
44,
45].
The most common complication is low bowel obstruction, found in approximately 20% of the cases of colorectal cancer and can occur either relatively abruptly, or is preceded by initially discrete premonitory symptoms, non-specific (until advanced evolutionary stages), and generally neglected or incorrectly interpreted [
18,
46].
The common obstructive mechanism is simple obstruction and is specific to situations with preceding manifestations (transit disorders, anemia, weight loss, etc.). For forms with sudden onset may occur intussusceptions (rare at the colic level and non-existent at the rectal level), volvuluses of supratumoral mobile segments and the association of peritoneal carcinomatosis or enteral ischemic phenomena. Colic volvulus is favored by the increased weight of endoluminal content and hypermobility, with fixed points of the extremities as close as possible. In intestinal volvuluses, necrosis is not directly correlated with the number of rotations of the loop, but with the degree of “constriction of the affected mesenteries” [
29,
47].
Low bowel obstruction due to neoplastic cause (colon and rectal cancer) presents anatomical and functional characteristics important in stage, pathogenic, topographic, and etiological diagnosis, orienting therapeutic consequences.
2.1. Anatomical Factors
2.1.1. The Diameter of the Colorectal Segments
The simple obstructive mechanism is installed later in colic segments with large caliber. Subsequently, the ileocecal valve follows the segment with the largest diameter (the cecum and the ascending colon), which explains the lower frequency of right colon occlusions if the Bauhin valve is not interested. The diameter of the colic lumen decreases discreetly to the distal segments (except the rectal ampulla). Peritumoral sclerolipomatosis and anemia are more common in the right colon, contributing to the shaping of the characteristics specific to this level of tumor location [
48,
49].
2.1.2. The Thickness of the Colic Wall
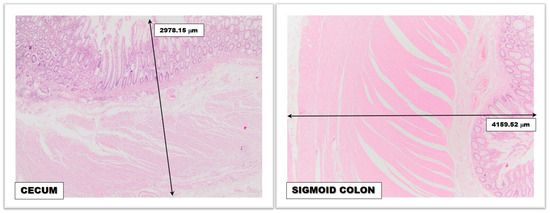
The thickness of the colic wall has less importance regarding the frequency of colorectal neoplasms on certain topographies but has profound relevance in relation to retrograde diastatic perforations (Laplace’s law) (
Figure 1). The large colic caliber associated with the reduced thickness of the wall allows the development of lateral rupture pressure that makes the cecum and ascending colon wall vulnerable (the rupture pressure at this level is approximately 80–100 cm H
2O, compared to the one in the small intestine where it is approximately 200–300 cm H
2O) [
50,
51,
52,
53].
Figure 1. Microscopic image revealing the difference between the thickness of the normal cecal wall and the normal sigmoid colon wall; magnifying glass, 4× (obtained from the Histopathology Department, “Bagdasar-Arseni” Clinical Emergency Hospital from Bucharest).
2.1.3. Colorectal Vascularization
Although it enjoys two important arterial sources (upper mesenteric artery for the right colon and lower mesenteric artery for the left colon) and marginal arches Drummond and Riolan-Haller and inconstant central intermesenteric anastomosis Huard, the colon does not benefit through long and short vasa recta arteries of a generous arterial flow comparable to the upper segments of the tract digestive system (stomach and small intestine). Mesenteric arteries are the preferred territories for the phenomenon of atheromatosis contributing to the progressive decrease of blood flow in irrigated territories. Elongation of vasa recta in the distended colic wall favors ischemia and parietal microthromboses, precipitating colic perforation. The closing of the venous network (a consequence of parietal pressure) is an additional factor in the irreversibility of parietal lesions [
54,
55].
2.1.4. Anatomical and Functional Sphincters
The colorectal area stretches between the ileocecal valve and the anal sphincter. The latter is of limited importance in low intestinal obstruction, being most commonly located under the obstacle. The ileocecal valve is deeply involved in the pressure play and dynamics of the cholic stasis content in low intestinal obstruction. A “permissive” valve can favor the reflux of stercoral content towards the ileal and then jejunal territory, tempering for the moment the axial and lateral pressures from the obstructed colon. Its increased pressure competence can close the possibility of retrograde reflux, with the exponential increase of intracolic pressures.
The functional sphincters of the colon (Cannon-Boehm, Payr, Moutier, and Obiern) are limited areas with better represented circular musculature and may have a limited role in colon dynamics in the early stages of the obstruction evolution. It can be concluded that Laplace’s physical law may be influenced by cholic morphofunctional characteristics [
56,
57].
2.1.5. The Mobility of Colic Segments
The mobility of colic segments can influence the dynamics of the obstructive process. If the fixed segments are the site of tumor development, they will suffer a simple process of obstruction, while for mobile segments other obstructive mechanisms may overlap (intussusceptions, volvuluses, etc.) [
58].
2.1.6. Tumor Morphopathology
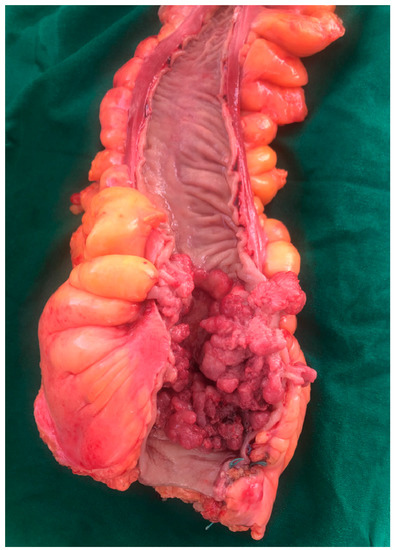
Obstruction of the colic lumen is more common in ulcer-vegetative (
Figure 2), exophytic, and polypoid forms. Diffuse infiltrative forms can also be incriminated, especially in situations where the axial extension of the tumor is very large [
59].
Figure 2. Postoperative specimen of a tumor located in the colorectal junction (collection of General Surgery Department—“Bagdasar-Arseni” Clinical Emergency Hospital from Bucharest).
2.2. Functional Factors
2.2.1. Colic Peristalsis
Colic innervation is vegetative, receptor and effector. The Meissner submucous plexus and axons of neurons in the posterior root node of the spinal nerves T11-L1 are responsible for visceral sensitivity. The secretive and motor activities are modulated by the Auerbach myenteric plexus, unequally represented for the right colon (related to the upper mesenteric plexus) and the left colon (dependent on the lower mesenteric plexus). The poor representation of the myenteric plexus is associated with a diminished peristaltic accompanied by a background distension of the left colon (megadolichocolon), decompensated early in the obstacles of colorectal junction or below this level. Colic hyperdistension makes the action of pharmacological active factors (acetylcholine, neostigmine) ineffective on tonus and peristalsis [
60,
61].
2.2.2. Other Functional Factors
Other functional factors involved in the pathogenic mechanisms of low intestinal obstruction depend on the individual characteristics of each patient, or derive from anatomical considerations: cholic resorptive function, dramatically extracted dysmicrobisms [
62,
63], nutrition prior to the installation of the obstruction, degree of damage to the mucus-epithelium barrier [
64], associated diseases that amplify the effects of dysvolemia and sepsis, various reflex factors, etc. [
65,
66].
Success in the complex treatment of a low neoplastic obstruction is conditioned by a complete diagnosis, adequate pre-operative preparation, a surgical act adapted to the case (in one, two or three successive stages) and dynamic postoperative care. Diagnostic errors consist both in overestimating the case (sometimes practicing exploratory laparotomy in medical conditions that evolve with intestinal paresis), but especially in the negative (assessment of the case as a non-surgical emergency, failure to identify cases with initial ischemic mechanism, not performing intraoperatively the diagnosis of all obstructive mechanisms involved and incomplete, inadequate or with potential for relapse surgical solutions). Etiological clarification is only possible sometimes, but this aspect is not a major drawback given the indication of surgical exploration, which will clarify this aspect as well.
Preoperative management of patients diagnosed with bowel obstruction involves, even from the emergency room, the placement of a peripheric venous catheter and starting the infusion of crystalloid solutions such as saline or Ringer solution. Acid-base and electrolyte rebalancing is a priority, often requiring repeated assessments of serum ions and pH. Considering the potential for dehydration and the rapid evolution of the disease, a urinary catheter is necessary for monitoring diuresis. In patients with severe cardiac, renal, or pulmonary failure, monitoring of fluid and electrolyte rebalancing using central Swan-Ganz catheters may be helpful. Preoperative hematological imbalances such as severe anemic syndromes can be adjusted by blood transfusions and severe thrombocytopenia by administering platelet masses. In the case of coagulopathy (liver cirrhosis, hematological disorders) or in case of changes in coagulation parameters due to treatments for various cardiologic disorders, prompt administration of plasma or vitamin K is necessary. Antibiotherapy, thromboembolic prophylaxis, and treatment of associated diseases are equally important [
52,
67,
68,
69,
70].
The moment of surgery should be chosen with great care and is the result of the experience of the anesthetic-surgical team. The operative act must be adapted to the case and has as its main objective the resolution of intestinal obstruction and only in a secondary way the resolution of the generating disease. The resection of the involved colorectal segment is performed (right or left colectomy, segmental colectomy, rectocolectomy), respecting oncological principles. Afterward, anastomosis is taken into account when the proximal segment shows no structural changes. Otherwise, to avoid a digestive fistula, it is recommended to close the distal segment and perform an ostomy at the level of the proximal one [
71].
Often, the surgical procedure does not involve the removal of the obstructive process, but only the restoration of the digestive transit. This involves cases in which is intended to shorten the duration of the surgical intervention due to the patient’s comorbidities and the general condition at the time or procedures performed for palliative purposes, for advanced neoplasia. In the case of external digestive derivations without removal of the obstructive process, it is recommended to perform a continuous ostomy, in order to avoid a “closed loop” [
72].
“The patient with intestinal obstruction is in the situation of a rescued from drowning. This is not the case for a swimming lesson”—Wangensteen.
The postoperative stage can crown the effort made to save the patient or compromise the previous efforts and should be managed by a multidisciplinary team. Analgesic, antibiotic, prokinetic, and anticoagulation therapy in the case of prolonged immobilization should be taken into account. Diuresis and intestinal transit will be monitored, and oral nutrition will be gradually resumed. Local complications (wound abscess, necrosis, evisceration, ostomy dehiscence or parastomal abscess) or general complications, such as cardiorespiratory, renal, or hepatic failures, should be closely monitored and treated promptly [
73].
This entry is adapted from the peer-reviewed paper 10.3390/medicina59050875