Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Orthopedics
Articular cartilage has very low metabolic activity. While minor injuries may be spontaneously repaired within the joint by chondrocytes, there is very little chance of a severely impaired joint regenerating itself when damaged. Therefore, any significant joint injury has little chance of spontaneously healing without some type of therapy.
- mesenchymal stem cells
- arthritis
- tissue regeneration
1. Introduction to Articular Cartilage
Articular cartilage is a typical hyaline cartilage. It consists primarily of chondrocytes and extracellular matrix including mostly type II collagen, a slight amount of collagen type VI, IX, XI, and XIV, as well as proteoglycans that bind water. In fact, approximately 70–80% of hyaline cartilage is composed of water. This tissue is characterized by a lack of direct innervation, nutrient blood supply, and lymphatic drainage. Its metabolic activity is low, and the proliferation of chondrocytes is very slow. These characteristics lie behind the poor self-healing processes and capacity for spontaneous repair. Cartilage injury without regenerative treatment is the reason that it affects the surrounding tissues, which leads to degeneration and osteoarthritis (OA) development [1,2,3]. Chondrocytes are trapped in the niches and cannot migrate to the damaged areas. In both the normal and pathological states, the environment of chondrocytes in the articular cartilage is very low in oxygen and tension, meaning that the chondrocytes are not under the same physical stresses as the type II collagen fibers, but they are also farther away from the fibers that may need to be repaired. All these tissue-specific environmental conditions create problems for regeneration [4]. The absence of cartilage vascularity does not allow progenitor cells to enter the cartilage, which could participate in and support the regenerative process [5,6]. In adult articular cartilage, cellular components are mostly postmitotic, with a low turnover rate, and have very limited self-repair abilities. The supply of glucose and oxygen to the cells mostly depends on diffusion from the synovial fluid and from the subchondral bone [7]. Figure 1 depicts the general overall composition of articular cartilage in adults and shows the small percentage of chondrocytes normally available to repair damaged tissues.
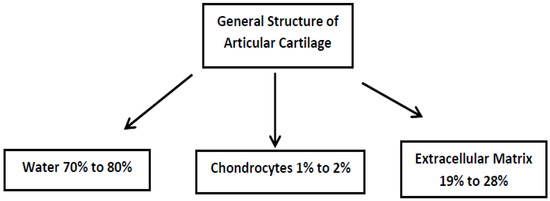
Figure 1. The general overall composition of adult articular cartilage. The majority of this cartilage is composed of water bonded to proteoglycans and extracellular matrix. Only chondrocytes can repair damaged cartilage. However, their low numbers and difficulty in migrating to where they are needed do not allow articular cartilage to be easily regenerated.
In the articular cartilage structure, there is an articular surface acting as the outermost layer followed by four main zones. They are distinguished based on the shape of the chondrocytes, the composition of the extracellular matrix, and the orientation of the type II collagen fibers. The thinnest layer is the superficial or tangential zone (10–20%), which protects deeper layers from potential damage caused by articulation and is in direct contact with synovial fluid. Often abbreviated as the STZ, the superficial zone is aligned parallel to the articular surface, is tightly packed, and is composed mainly of Type II and IX collagen. Chondrocytes in the STZ are relatively flat. Directly under the STZ is an intermediate or middle zone, which is the thickest layer (40–60%). The function of this layer is to resist moderate compression. Therefore, it has thick fibrils of collagen that are neither perpendicular nor parallel, but are slanted, and it also contains water bonded to proteoglycans, which help to resist compressive forces. The chondrocytes in the middle zone are characterized by their low density and spherical shape. Directly under the middle zone is the deep or basal zone (30–40%), which has the highest resistance to compression. This resistance to compression comes from radially arranged thick collagen fibrils that are arranged perpendicularly to the articular surface. This zone has many proteoglycans but very little water. The chondrocytes in this layer are arranged parallel to the collagen fibers and are columnar. Under the deep zone is a tidal mark that separates it from the calcified zone. The main job of the calcified zone is to attach the cartilage to the bone. In this layer, there are very few chondrocytes and the few that reside there are hypertrophic [4,8].
The chondrocytes are considered to be the only cellular component of the articular cartilage. Their main physiological function is the synthesis and degeneration of the extracellular matrix [9]. However, even adult articular cartilage contains MSCs and/or mesenchymal progenitor cells capable of differentiating into chondrocytes [7,10]. The highest concentration of stem cells is within the superficial zone of articular cartilage [8,11]. The chondrocytes of the articular cartilage are under physioxic/hypoxic conditions, but still have their normal metabolism (the oxygen gradient ranges from 10% to 1%, from the superficial to the deepest layers, respectively), and produce type II collagen and aggrecan (a proteoglycan made of chondroitin sulfate and keratin sulfate chains which can retain significant amounts of water).
All the structural and mechanical properties of the articular cartilage are subordinated into two major functions. These are the smooth gliding of the articular surfaces, as well as the protection of subchondral bone from mechanical stress [1]. In order to keep homeostasis in the tissue, there is a required homeostatic balance between the lytic, tissue-damaging mediators (cytokines that trigger catabolism, free radicals, proteases, and prostaglandins), as well as the reparative substances and physiological inhibitors (growth factors, inhibitors of catabolic cytokines, and degenerative enzymes) [9]. Aging is the major factor affecting the ability of chondrocytes to maintain and restore articular cartilage. With aging, the number of chondrocytes decreases, they begin to deteriorate (senescence), and more factors that cause apoptosis can be found. This is the main reason for the increased risk of articular cartilage degeneration with age [4].
Chondral and osteochondral defects mostly do not heal themselves without intervention, which leads to progressive joint degeneration [13]. If the cartilage repair processes take place, they are usually weak and nonfunctional, due to the replacement of damaged cartilage by a fibrocartilage-like scar tissue [4,14]. The biomechanical properties of fibrocartilage are inferior in quality when compared with hyaline cartilage, and effective joint restoration is not possible [15]. When compared to hyaline cartilage, fibrocartilage contains more collagen and fewer proteoglycans. Moreover, type I collagen is mostly represented. This has a lower compressive strength, elasticity, and wear resistance than type II collagen, which is specific and characteristic for “normal” articular cartilage [16]. Events that meet cartilage regeneration requirements occur in embryos, but quickly wear off after birth. In adults, this type of regeneration has never been noticed, and only the cartilage repair process is possible [1,15].
2. Osteoarthritis
Osteoarthritis (OA) is a chronic degenerative joint disease. The articular cartilage damage could be induced by biomechanical, metabolic, biochemical, or genetic factors. Increased risk factors of OA are obesity, aging, direct joint injury (a strong single event or cumulative micro-traumatic events), and/or a genetic predisposition. OA is a complex disease (it encompasses the entire joint) that activates all aspects of the immune system response. Progression of the disease involves cartilage, subchondral bone, synovium, tendons, ligaments, muscles, and even neural tissues. There is no doubt that in the late stages, OA is a systemic disease [17,18]. Two major categories of OA can be distinguished in general: (1) mechanical OA—healthy articular cartilage undergoes excessive loads leading to degeneration, and (2) structural OA—articular cartilage is weak, showing some abnormalities that contribute to rapid degradation. Even minor cartilage defects often lead to osteoarthritis [7]. Secondary OA might be the result of previous tendon or ligament injury, joint instability due to intra-articular fracture, or wear and tear of the articular cartilage. OA is one of the most challenging joint diseases and has several phenotypes [1,2].
Any of the body joints can be affected by OA. The knee is one of the most OA-affected joints in humans [19,20]. The knee, hip, elbow, carpal, tarsal, and vertebral joints are the most commonly osteoarthritic in both humans and pets [21,22]. Large and giant breed dogs are particularly vulnerable to OA; however, all sizes and breeds can be affected due to age and being overweight [21,22,23]. This is why canine animal models were used in studying stem cell therapy for the treatment of OA.
3. Stem Cells
Stem cells are precursor cells. The cells have the ability to self-renew, can stay in an undifferentiated state, show high plasticity, can transdifferentiate, and have quite a long life span. There are two pathways through which these cells can divide: (1) symmetric division—the daughter cell is identical to the antecessor and both cells remain as undifferentiated stem cells, or (2) asymmetric division—the daughter cell has limited developmental potential, which is the way stem cells differentiate and specialize into lineages [28]. These cells are unspecialized but can give rise to other specialized cell types [29]. There are two possible origins of stem cells. They may either be embryonic (ESCs), coming from a very early embryo or blastocyst, or they may be postnatal/adult stem cells (ASCs), which are undifferentiated, capable of self-renewal, and responsible for adult tissue regeneration [28,29].
There are various types of adult stem cells. There are hemopoietic stem cells (HSCs) that give rise to all blood cell components, including neutrophils, lymphocytes, natural killer cells, dendritic cells, macrophages, and monocytes. These HSCs are of mesodermal origin, are derived from bone marrow, and generate all blood cell types [28]. There are also mesenchymal stem cells (MSCs) that give rise to osteoblasts, chondrocytes, adipocytes, and the reticular stroma.
4. Mesenchymal Stem Cells (MSCs)
The most useful stem cell for tissue engineering and implantation for the treatment of OA are mesenchymal stem cells (MSCs). These are usually restricted to forming only mesodermal specific cell types (adipocytes, osteoblasts, myocytes, and chondrocytes), but several are able to differentiate into other cell varieties. The trophic effects of MSCs include the secretion of bioactive molecules that are anti-apoptotic, immunomodulatory, angiogenic, ant-scarring, and/or chemoattractant [32,33]. Stem cells in adults reside in niches, which are limited and have a specialized microenvironment. These cells have a physical anchoring site with a set of factors that control the cell number, activation, proliferation, self-renewal, or lineage differentiation. The microenvironment of the niche, with all its factors and signaling modulators, maintain homeostatic regulation of the stem cells by the up- or downregulation of the signaling pathways.
The paracrine effects of MSCs can be divided into three types: trophic, immunomodulatory, or chemoattractant. The trophic effects mainly stimulate neighboring parenchymal cells. These include the inhibition of apoptosis, and the support of regeneration, stimulation, maintenance, proliferation, and differentiation of tissue specific progenitors [32]. The immunomodulatory aspects may include an immunosuppressive effect, and immunoactivity mediation by direct cell–cell contact and by the secretion of bioactive molecules. The cells involved in interactions may include dendritic cells, B cells, T cells—including T regulatory cells and T helper cells—and killer cells.
Although MSCs can be found in various niches, they have many functional similarities. MSCs derived from various sources display different toll-like receptors (TLRs), which have functional properties, and respond to stimulation by TLRs agonists. TLRs are transmembrane proteins which play critical roles in the immune system by mediating inflammatory responses, primarily through the binding of ligands. MSCs are not spontaneously immunosuppressive, and the presence of inflammatory mediators may be essential for MSC-mediated immunosuppression and modulation of the functional properties.
5. Causes of Osteoarthritis
Unfortunately, chondrocytes may over-produce matrix-degenerating enzymes, such as matrix metalloproteinase 13 (MMP-13) [2,36]. While MMP-13 is needed for the healthy maintenance of articular cartilage, its overproduction can promote OA. In the osteoarthritic joint, there is a great mobilization of macrophages, and this consequently produces cytokines. The two major pro-inflammatory cytokines that have an impact on the progression of cartilage breakdown are IL-1β and TNF-α, which work by promoting catabolic and degradative processes. Experiments conducted on mice have suggested that a decrease in the TGF-β level (produced by synovial macrophages) induced osteophyte formation [17,36].
There are catabolic and pro-inflammatory mediators in OA, such as cytokines and nitric oxide, which play an important role in triggering the pathophysiology of OA by instigating the formation of free radicals (reactive oxygen species). The overproduction of cytokines triggers inflammatory stress that is responsible for degenerative and inflammatory tissue damage. Another type of mechanism is a destructive process activated by reactive oxygen species, which involves the induction of chondrocyte apoptosis [9].
6. Traditional Therapy and Models of OA
There is no effective therapy against the progression of OA. Currently, pain management, activity modification, and weight loss are prescribed in the early stages, but in the advanced stages there are very few options available. There are a few alternatives to help with moderate OA such as high tibial osteotomy of the knee joint, for example, in order to attempt to realign that particular joint. However, the patient must not be in too advanced of a stage of the disease [39]. Another traditional therapy has been hyaluronic acid; however, artificial hyaluronic acid can only provide temporary pain relief [40]. Joint replacement is generally the therapeutic procedure employed [41]. Animal models of OA of the knee have included horse, sheep, rat, mouse, rabbit, and guinea pig [41], as well as a caprine model (goats) [26] and dogs [42,43]. The large-animal models have had the most advantage in modelling the human progression of the disease, as compared to small-animal models, since they have a larger body, longer life, long-term follow-up, and are a better simulation of human pathology [44].
The main aim of traditional pharmacotherapy for OA is pain relief or reduction. Commonly used pharmacotherapies are acetaminophen, non-steroidal anti-inflammatory drugs, and opioid analgesics (tramadol). Intra-articular injections of corticosteroids are also applied; however, these treatments do not inhibit the decay process and adverse events are frequently noticed with prolonged use of these pharmacotherapies [2]. The prolonged administration of drugs is an inherent problem in most chronic diseases and is associated with possible gastrointestinal, renal, and hepatic adverse events [18]. The traditional multi-modal therapy of inflammation and pain reduction includes long-term cyclo-oxygenase-inhibiting non-steroidal anti-inflammatory drug (NSAID) therapy, physical therapy, diet, weight management, and dietary supplements.
7. Regenerative Medicine
The most important and most difficult task of cartilage tissue engineering is creating a functional substitute for native cartilage [5,34]. In 1993, Langer and Vacanti defined tissue engineering as accentuating the interdisciplinary character to restore, maintain, or improve tissue function [3]. Regenerative therapy/cell therapy, especially with the use of stem cell technology, may one day fulfil the requirements of delaying OA progression and joint tissue repair [2,34]. In 1968 in the United States, the first successful allogenic stem cell graft in humans using donor bone marrow was undertaken [31]. This was perhaps the first step in using mesenchymal stem cell technology.
Chondrocyte implantations for cartilage regeneration has quite a long history, dating back to 1994 [46]. The clinical use in human patients actually began in 1987 [4]; however, since OA has such complex degenerative joint changes in different age groups of patients, the therapy was not fully effective. Mesenchymal stem cells are preferred since they may be collected from different tissues, are actively immunosuppressive, have a capacity for chondro-differentiation, and have a high proliferation potential [2,14]. Bone marrow and adipose derived MSCs have been most commonly used for OA treatment and repair. The disadvantage of autologous chondrocytes as regenerative cells is that they have a limited capacity to proliferate [18,47].
8. Mesenchymal Stem Cells and the Treatment of OA
As previously mentioned, but worth reiterating, there are two types of cells used for cartilage engineering: (1) chondrocytes, which were the first to be used and are obtained by the isolation and amplification of autologous chondrocytes unless the monolayer cultured chondrocytes rapidly lose their phenotype, and (2) mesenchymal stem cells (adult MSCs from different sources). Adult MSCs are of major interest in tissue engineering. MSCs that have already been applied have been sourced from bone marrow (most popular source), adipose tissue, muscles, periosteum, perichondrium, synovium [3,33], umbilical cord blood, as well as muscle and peripheral blood [1,48].
MSCs seem to provide some important advantages over chondrocytes when considering the treatment of degenerative joint diseases. They are easier to culture, more rapidly proliferate, and can specialize to become all tissues within the joint. Moreover, the paracrine activity seems to be most beneficial in treating OA conditions. The anti-inflammatory and immunomodulatory properties of MSCs play a pivotal role in orchestrating the reparative response of damaged joint tissues [36,41,49]. Mesenchymal stem cells (MSCs) interact with immune cells and are responsible for the modulation of a number of effector functions, immunomodulatory properties, migratory abilities, the induction of peripheral tolerance, inhibiting the release of pro-inflammatory cytokines, and the promotion of tissue repair.
The advantage of using MSCs for treating OA include their capacity to differentiate into chondrocytes and their potential to prevent chondrocyte apoptosis and to prevent the overall process of degeneration (through a paracrine effect) [37]. They also modulate the activity of the immune system (via an immunosuppressive function), secrete cytokines and chemokines, suppress T cell proliferation, and inhibit the respiratory burst in neutrophils. The environment is responsible for modulating the balance between the pro-inflammatory and anti-inflammatory properties of MSCs [49]. Many pre-clinical and clinical trials have employed MSCs for OA management. The most important issues are the accuracy of evaluating the processes of disease progression, and the evaluation of cartilage regeneration. For quite some time, MSCs were regarded to be ‘immune privileged’, meaning that they are hypoimmunogenic. However, recent studies have suggested that MSCs may not be ‘immune privileged’, but “immune evasive”.
The reason for allogenic MSC transplantation, rather than an autograft, is that there is a suspicion that OA patients, especially in advanced stages, are not the best donors of MSCs for their own treatment. Some authors have suggested that OA patients may have systemic depletion and derangement of MSCs. Cell differentiation and proliferation capacity may be too low to make a positive difference in the rebuilding of joint homeostasis. This negative impact on MSC dysfunction seems to be greater in bone marrow-derived cells than in MSCs derived from adipose tissue [41].
This entry is adapted from the peer-reviewed paper 10.3390/ijms24108925
This entry is offline, you can click here to edit this entry!
