Oral and maxillofacial tissue defects caused by trauma, tumor reactions, congenital anomalies, ischemic diseases, infectious diseases, surgical resection, and odontogenic cysts present a formidable challenge for reconstruction. Antioxidants are materials that preserve cells from the damage caused by free radicals [21]. They can control the harm of oxidative stress directly through the reaction with free radicals or indirectly through inhibition of the activity of free radical-producing enzymes or improvement of the activity of intracellular antioxidant enzymes. In addition to the inhibitory impact of antioxidant materials on ROS products, their osteogenic/odontogenic differentiation effects are of great interest in dental and facial tissue regeneration.
1. Introduction
Oral and craniomaxillofacial diseases in the area of the face, dental arches, and craniofacial hard and soft tissues are caused by chemical, physical, microbial factors, and systemic diseases [
1]. Among these diseases are oral infectious diseases such as dental caries and periodontitis; craniofacial tissue disorders (due to cysts, tumors, trauma, and abnormalities); and other conditions, including salivary gland disorders, neurological diseases, and temporomandibular joint (TMJ) disorders, which are usually related to teeth [
2]. Some clinical strategies are available for treating damaged tissue, such as autografting, allografting, and xenografting; however, none of these methods is the ideal solution due to their drawbacks and limitations [
3,
4]. Multifunctional biomaterials have been proven to be a promising alternative treatment strategy [
5]. However, in practice, implanted biomaterials face some problems, such as reactive oxygen species (ROS) and free radicals generated by immune responses and surrounding connective tissue, such as hydrogen peroxide (H
2O
2), superoxide ions (O
2−), hydroxyl radical (OH·), and nitrogen oxide (NO), which can interfere with successful cellular repopulation and tissue regeneration following transplantation [
6,
7]. While oxidative stress at low concentrations has many physiological functions and plays an important role in tissue regeneration [
8], the high level of ROS may hinder tissue repair as it commonly causes severe tissue injuries, leading to cell damage through distinct mechanisms, such as membrane disorganization and protein/nucleic acid damage [
9,
10]. Tissue-engineered implants are susceptible to increasing ROS levels because of the destruction caused by reperfusion after ischemia, which occurs in tissue and organ engineering transplants [
11,
12].
Additionally, tissue oxygenation during in vitro implant preservation and surgery may lead to local hyperoxia and contribute to ROS-induced organ damage [
13,
14]. Consequently, it has been proposed that delivering antioxidant materials combined with tissue engineering may be viable to achieve efficient tissue/organ regeneration and limit post-implantation failure. Specific kinds of antioxidant materials in the form of micro/nanosized particles (e.g., ceria (nanoceria)), carbon materials (e.g., carbon nanotubes), manganese, and selenium [
15,
16,
17] and medicinal herb extracts (e.g., enzymatic (catalase and glutathione peroxidase)) and non-enzymatic antioxidants (flavonoids and polyphenols) have been successfully applied to scavenge free radicals and prevent excess ROS generation in tissue engineering and regenerative medicine applications [
18,
19,
20]. There is an emerging trend of using antioxidants as bioactive, ROS-reducing molecules to modify implants/tissue-engineered grafts. The ability of these biomolecules to control oxidation-reduction (redox) processes in vivo and in vitro (3D cell culture before surgical implantation) can facilitate cell survival and homeostasis.
2. Antioxidant Materials
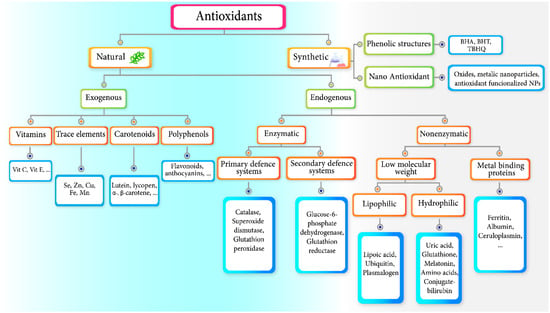
There are two main classes of antioxidants, depending on their source: natural and synthetic. The diagram of the antioxidant classification is presented in Figure 1.
Figure 1. Summary of antioxidant classification.
2.1. Natural Antioxidants
Plants, such as edible fruits, vegetables, spices, and herbs, are the main source of natural antioxidants because they are rich in polyphenols, carotenoids, vitamins, and minerals [
30,
31]. Natural antioxidants can hinder the approaches of oxidation and the microorganism’s growth [
32]. As depicted in
Figure 1, there are two major categories of natural antioxidants, i.e., exogenous and endogenous antioxidants. While endogenous antioxidants are responsible for repairing all of the damages caused by free radicals via initiating cell regeneration from the inside on out, exogenous antioxidants only repair some of the damages caused by free radicals outside and inside by stimulating (not initiating) cell regeneration. The endogenous antioxidants are divided into enzymatic and non-enzymatic antioxidants. They are different in place and mode of action and final effects. Enzymatic antioxidants mainly protect the cells, while non-enzymatic antioxidants generally act in the plasma. Enzymatic antioxidants are uniquely generated by the human body and as indicated in
Figure 1 and are classified into primary and secondary antioxidants. Primary antioxidants are as follows: catalase (CAT), superoxide dismutase (SOD), and glutathione peroxidase (GPx) [
33]. Because of its vital role in maintaining cellular redox homeostasis, glutathione (GSH) is one of the essential cellular antioxidants. The cysteine amino acid contains a thiol group, which is a reducing agent, and regularly and repeatedly undergoes a reversible oxidation-reduction reaction. The cells preserve a high concentration of the reduced form of glutathione with the help of glutathione reductase (GR). GSH, in turn, can reduce other enzymes and metabolites [
33]. Nonenzymatic antioxidants are not found in the human body naturally and must be supplemented in a diet for proper metabolism [
34].
2.2. Synthetic Antioxidants
Synthetic antioxidants are molecules of various chemical structures created by specialists to benefit humanity. These antioxidants have been successfully used in several products, including food, pharmaceuticals, and cosmetics; however, their carcinogenic activity has limited their usage [
38]. Butylated hydroxy anisole (BHA), butylated hydroxytoluene (BHT), propyl gallate (PG), tert-butyl hydroquinone (TBHQ), and ethylenediaminetetra acetic acid (EDTA) are the most commonly utilized synthetic antioxidants. Synthetic antioxidants are bioequivalent to their natural counterparts; for example, biovitamin C vs. chemically manufactured L-ascorbic acid [
21,
39]. These antioxidants are often more active and purer than natural antioxidants and have consistent antioxidant activity; however, they must meet the regulatory authorities’ nontoxicity and safety criteria before marketing.
3. Mechanisms of Antioxidants’ Activity
The mechanisms of the antioxidant compounds’ activities have a close relationship with the chemical structure of the free radicals, the reactivity of the free radicals, and the environment where the reactive species are found. Hence, describing the ROS and reactive nitrogen species (RNS), which include both free radicals and precursors, is very important. It should be mentioned that the reaction between the free radicals and antioxidants is a second-order reaction; therefore, it not only depends on the amount of free radicals and antioxidants but also depends on the chemical structure of both reagents, reaction conditions, and medium. For instance, phenolic structures inhibit or reduce free radicals through hydrogen atoms transferred from their hydroxyl group. The mechanism of the reaction of a peroxyl radical (ROO•) containing phenolic antioxidants involves a concerted transfer of the hydrogen cation from the phenol to the radical, forming a transition state of an H-O bond with one electron. The capacity of phenolic antioxidants is highly reduced when a solvent prone exists in the reaction medium to form a hydrogen bond with the phenolic antioxidants. Another antioxidant component, vitamin C, chemically reacts with the important ROS in the body and acts as a hydrosoluble antioxidant. The mechanism of its antioxidant activity is associated with hydrogen atom transfer to peroxyl radicals, molecular oxygen elimination, and inactivation of singlet oxygen [40,41].
4. Role of Antioxidant Materials in the Tissue Regeneration Process
4.1. Hard Tissues in the Craniofacial and Alveolar Area
4.1.1. Craniofacial Bone Regeneration
Craniofacial fractures and bone defects in both the maxilla and mandible area occur as a result of trauma, congenital anomaly, and osseous deficiency, following resection of tumors, and subsequent tooth loss and extraction. Despite the significant ability of the bone to regenerate itself, external interventions are often essential for the comprehensive recovery of large bone defects and complex fractures. Oxidative stress and delayed angiogenesis are two important fundamental factors related to the low-quality healing process of large craniofacial defects [
55].
Natural antioxidants have been extensively applied to reduce ROS products at the damaged tissue site. For example, green tea is one of the most popular drinks, which mainly consists of tea polyphenols (catechins). The main chatechins found in green tea are epicatechin (EC), epigallocatechin (EGC), epicatechin-3-gallate (ECG), and epigallocatechin-3-gallate (EGCG). Among them, EGCG is much more abundant than other tea polyphenols. Several studies have revealed that EGCG has significant inhibitory impacts on abnormal processes, such as antioxidant, anti-inflammatory, anticancer, antifibrosis, and anti-collagenase effects. Regarding this, Rodriguez et al. [
57] studied the impact of EGCG and α-tricalcium phosphate (α-TCP) on bone regeneration. These materials were applied after calvarial surgery in Wistar rats. They divided the rats into two groups. In the test group, the calvarial defect was filled with different doses of EGCG (0, 0.1, 0.2, 0.4 mg) combined with α-TCP particles, and, in the control group, the defect was not filled. The results revealed that the mixture of α-TCP with 0.2 mg of EGCG increased new bone formation in rat calvarial defects, and this mixture would become the potential bone graft material. Propolis is another natural antioxidant that is produced by honeybees from certain tree species. Caffeic acid phenethyl ester (CAPE) is an active component of propolis. It has been suggested that 10 μM of this substance could significantly inhibit the production of ROS in human neutrophils. Previous studies have also shown that CAPE has antioxidant, anti-inflammatory, and anticancer impacts [
58,
59].
As popular natural sources, plant-derived phenolic compounds exhibit antioxidant, osteogenic, and anti-inflammatory features, which make them suitable for the improvement of bone regeneration [
62]. In a study by Bahattarai et al. [
63], coumaric acid (3-[4-hydroxyphenyl]-2-propenoic acid) was combined with collagen and recombinant-human cartilage oligomeric matrix protein-angiopoietin 1 (rhCOMP-Ang1) to enhance osteogenesis in mandibular critical-sized defects. The antioxidant features of coumaric acid caused scavenging of ROS and halted inflammation reactions. To summarize, it showed that the synergetic interaction between rhCOMP-Ang1–enhanced angiogenesis and coumaric acid-related antioxidant responses could enhance the regeneration of critical-sized bone defects.
4.1.2. Alveolar Bone Regeneration
Periodontal tissue (periodontium) is a sophisticated and functional tooth-surrounding tissue. Periodontium includes both hard and soft tissue, such as alveolar bone, periodontal ligament (PDL), cementum, and gingiva [
99]. One of the most inflammatory diseases in dentistry is periodontitis. Plaque and oral bacteria are the important causes of this disease. More than 50% of people who live in the world suffer from periodontitis. The main source of periodontitis is bacteria and their elements, which can cause inflammation and subsequently damage the periodontium. When periodontitis occurs, ROS are produced, mostly by hyperactive neutrophils, and may not be balanced by the host antioxidant defense system, causing tissue damage; therefore, over the last few years, in support of the treatment of periodontitis, various biomaterials have been utilized as a contact inhibition membrane in guided tissue regeneration (GTR), which is the current gold standard clinical regeneration treatment [
100,
101].
As a natural antioxidant source, curcumin, an active ingredient of turmeric, was studied in the literature. Curcumin is considered an effective material for decreasing inflammation and bone resorption. Zhou et al. [
106] studied the effect of curcumin on bone after 30 days of daily administration of 100 mg/kg. They claimed that curcumin could reduce the inflammatory effect and alveolar bone loss in ligature-induced experimental periodontitis rats by reducing the levels of pro-inflammatory cytokines (and IL-6 and TNF-a) and osteoclastogenesis-related molecules, such as receptor activator of nuclear factor κ B (RANK) and receptor activator of nuclear factor kappa beta (RANKL). Another natural antioxidant material is Scutellaria baicalensis. Its extract contains baicalin and has shown anti-inflammatory and antioxidant properties. Chen et al. [
107] carried out a study to investigate the impact of baicalein with different concentrations (1.25, 2.5, 5, and 10 μM) on hPDLCs proliferation. Their results demonstrated that baicalein increased the growth of hPDLCs, increased ALP activity, activated the Wnt/β-catenin pathway, and up-regulated the expression of viability markers, such as β-catenin and lymphoid enhancer factor 1 (LEF1). They found that baicalein can improve hPDLC differentiation into osteoblast via the Wnt/β-catenin pathway.
Inflammation and alveolar bone resorption are the common side effects after tooth extraction. Inflammation can increase amounts of osteoclast and pro-inflammation cytokines ((TNF)-α and interleukin 1 β (IL-1 β)), as well as RANKL and RANK. RANKL and RANK molecules are important for osteoclast activation, thereby increasing alveolar bone resorption. To address this issue, several biomaterials are applied as anti-inflammatory and antioxidant factors. For example, Kresnoadi et al. [
109], combined polyethylene glycol (PEG) with demineralized freeze-dried bovine bone xenograft (DFDBBX) and xanthones (exists inside the mangosteen peel and containing dibenzopyran, an anti-inflammatory substance) in an animal study. Mangosteen peel extract (MPE) works as an anti-inflammatory and antioxidant agent. During the study, each mixture was applied locally after tooth extraction. One group received PEG only, the second group received DFDBBX + PEG, and the third group received MPE + DFDBBX + PEG. Finally, after 30 days, the immune histochemical evaluation demonstrated that the mixture of MPE with xenograft and PEG could improve the healing process and reduce bone resorption in tooth sockets. Hyaluronic acid (HA) also has distinctive physiochemical and biological properties, which make it beneficial in the treatment of the inflammatory process in medical fields such as periodontal disease treatment. It acts as an antioxidant agent by scavenging ROS and is able to stabilize the granulation tissue matrix. Moreover, it has a bone repair effect in periodontitis by inducing osteogenic substances, such as bone morphogenetic protein-2 and osteopontin. It was beneficial in controlling gingival bleeding and repair via decreasing peroxidase and lysozyme activities after a certain period.
4.2. Dental Hard Tissue Regeneration
In the oral and maxillofacial regions, teeth are crucial for chewing food, speaking, and maintaining facial beauty. The teeth are composed of four parts: three kinds of hard tissues called enamel, dentine, and cementum; and dental pulp in the central zone [
1]. Teeth have many similarities to bone in many aspects, including structural features, biomarkers, and mineralization activities; however, there are some differences. For example, while bone tissue undergoes continuous remodeling in life, including the development of new bones and the resorption of existing ones, dentine and cementum do not undergo remodeling; instead, they maintain their stability for a long time, while the dentine matrix is constantly deposited [
113]. Many reasons exist for teeth to be damaged or lost, including caries, radiation, dental disease, trauma, tumors, genetic factors, and oral deficits caused by hepatobiliary diseases that induce tooth discoloration, enamel, and dentine hypoplasia [
113,
114].
4.2.1. Enamel Regeneration
Enamel, the outer layer of the tooth crown, has the strongest bone structure in the body. A mature enamel consists of 95 wt.% carbonated hydroxyapatites, 4 wt.% water, and 1 wt.% organic matrix [
115]. Dental caries is one of the most prevalent medical conditions worldwide, which continues to be a considerable public health challenge [
116]. Dental plaque on teeth is a biofilm consisting of a smooth and sticky layer that often contains a gelatinous mass of bacteria. Natural antioxidants such as phenolic compounds can prevent radicals released from microbial activity from attaching to fluorescent compounds such as enamel. In addition, the effects of these materials as anticaries agents are significant even at low doses. These polyphenolic compounds found in herbs are believed to have many medicinal properties, including antioxidants, antibacterial, and anti-inflammatory effects [
117]. Different polyphenol sources with anticaries properties have been identified. For example, tea, cranberries [
118], and cacao bean husk extract [
119] have been reported to have anti-Streptococcus mutans properties.
4.2.2. Dentine Regeneration
Dentin, which is in the lateral walls of the pulp cavity and root canal and supports the enamel on its surface, constitutes the tooth’s main body [
83]. Dentine is composed of 70% minerals, 20% organic matter, and 10% water [
1]. Enamel caries that are left untreated will penetrate the deeper layer of dentin, break down the dentin collagen protein network, and cause severe pulpitis. Dentine collagen degradation may be facilitated by host-derived proteolytic enzymes, such as MMPs. Antioxidants can inhibit MMP activity and assist in the natural stabilization of collagen.
Dentinogenesis, the dentin formation process, begins when dental papilla cells (DPCs) differentiate into odontoblasts. Liu et al. [
123] have investigated how EGCG, a component of green tea, affects the odontogenic differentiation of stem cells from apical papilla (SCAPs). In the study, EGCG promoted SCAP proliferation without altering SCAP migration at low concentrations (0.1 or 1 µM). By activating the BMP–Smad signaling pathway, EGCG enhanced the osteo-/odontogenic differentiation of SCAPs. Therefore, EGCG can be beneficial for the dentin regeneration process.
4.2.3. Cementum Regeneration
Cementum is a mineralized bone-like tissue created by cementoblasts that surround the tooth root and connect the tooth by PDL to the alveolar bone [
127]. Therefore, it has a crucial role in the regeneration of periodontal tissues. The regeneration of periodontal tissues, especially cementum, is crucial to periodontal health. In a study by Gauthier et al. [
128], the effects of common osteogenic stimulants and vitamin C on the expression of cementogenic genes were investigated. Their results showed that periodontal ligament stem cells (PDLSCs) could not be guided toward cementogenic lineages by a common osteogenic medium containing vitamin D3, Dex, and β-glycerophosphate, indicating that, in response to such stimuli, pathways promoting specific cementogenic genes are inhibited rather than induced. In contrast, vitamin C was able to increase cementogenic gene expression. In addition, transplanting PDLSCs treated with vitamin C into immunocompromised mice in the study resulted in considerably more ectopic cementum and bone formation. Thus, for clinical cell-based periodontal regeneration, vitamin C treatment alone can be feasible and safe.
4.3. Oral Soft Tissue Regeneration
4.3.1. Periodontal Soft Tissue Regeneration
Periodontitis is a very usual infectious disease in the oral cavity and leads to the destruction of the periodontium. As mentioned previously, the periodontium consists of hard tissue (alveolar bone and cementum) and soft tissue (gingiva and periodontal ligament).
Naturally derived biomaterials with multifunctional properties have been suggested to have astonishing effects on periodontal repair and regeneration. Natural microbial exopolysaccharides (EPS) have attracted scientists’ attention because of their potential pharmaceutical properties such as antioxidant, anticancer, and anti-inflammatory effects. In a study by Kibar et al. [
112], EPS (50 mg/mL) exhibited 70% inhibition on biofilm formation, which could be in favor of suppressing periodontitis. In addition, dose-dependent antioxidant effects were detected for these biomaterials. Moreover, EPS increased the viability of hPDLFCs. Consequently, they concluded that EPS in the form of powder could enhance periodontium soft tissue regeneration and protect against free radicals.
4.3.2. Oral Wound Healing
Oral wound healing is a complicated biological process aimed at the restoration of anatomic structure and function, achieved by four different phases such as inflammation, hemostasis, proliferation, and remodeling [
132]. Non-healing oral wounds can significantly increase morbidity and possess negative effects on patients due to the unique properties of the oral cavity. During wound healing, excessive oxidative stress hinders the process by inducing inflammatory reactions. In addition, ROS suppress the regeneration of wound tissue by inhibiting the functions of endogenous stem cells and macrophages. Many researchers have reported the application of ROS-scavenging materials in the healing of oral wounds to speed up the regeneration process. Regarding this, Gu et al. [
133] investigated vitamin B2-modified iron oxide nanoparticles for promoting oral ulcer healing. Although oral ulcers are harmless and self-healing, they can be painful and reduce the patient’s ability to eat, drink, brush, and even speak, affecting his quality of life and working efficiency. Usually, oral ulcers are associated with inflammation and high levels of ROS, which exacerbate the patient’s symptoms. It was reported that vitamin B2-modified iron oxide nanoparticles improved peroxidase-like, catalase-like, and superoxide dismutase (SOD)-like activities. Additionally, vitamin B2 modification significantly increased the ROS-scavenging ability and protected human oral keratinocytes (HOK) and BALB/3T3 cells from hydrogen peroxide (H
2O
2).
4.4. Dental Pulp Tissue
In dental pulp tissue, similar to other tissues in the human body, medical treatments such as the removal of tissue during restorative and endodontic treatments or tooth movement during orthodontics, can induce oxidative stress and eventually increase the levels of pro-inflammatory factors, including TNF-α and interleukin-1β. Therefore, high levels of oxidative stress could be alleviated by applying antioxidants, which may enhance the healing of dental pulp tissue [
136]. In dental pulp tissue, ROS stress could damage different organic molecules, including proteins and DNA. Therefore, the production of internal antioxidants or the application of various biomaterials as an antioxidant treatment is helpful to neutralize the harmful effects of ROS in the pulp tissue [
137].
Dentin-pulp regeneration following tooth decay treatment plays an essential role in ensuring tooth viability. When hDPSCs differentiate into odontoblasts, intracellular ROS levels increase, consequently reducing the differentiation potential. Furthermore, antioxidants play a crucial role in odontoblast differentiation media, so preconditioning stem cells with antioxidants will synergistically enhance their differentiation. Researchers [
92] have incorporated an insoluble inorganic ceria nanoparticle (CNP), an antioxidant used for tissue regeneration in hard or nervous systems, into mineral trioxide aggregate (MTA) to accelerate odontoblast differentiation by reducing ROS levels. As a result of the utilization of CNP-incorporated MTA (CMTA), odontoblastic differentiation was accelerated without compromising compression strength. In this way, CMTA may provide dental materials capable of regenerating dentin-pulp complexes by directing pathological intracellular ROS toward beneficial biological outcomes. Researchers [
141] have evaluated the impact of grape seed extract (GSE), an antioxidant polyphenol, on the growth and mineralization of undifferentiated pulp cells (OD-21) and odontoblast-like cells (MDPC-23). MDPC-23 cells showed increased proliferation and protein content after 7 and 10 days, respectively. Additionally, undifferentiated pulp cells and odontoblast-like cells showed higher ALP staining intensity after 7 and 10 days. In the study, GSE enhanced differentiated cells’ functional activity more than OD-21 cells. However, to confirm GSE’s benefits for dentin regeneration, more studies should be conducted at various concentrations of GSE.
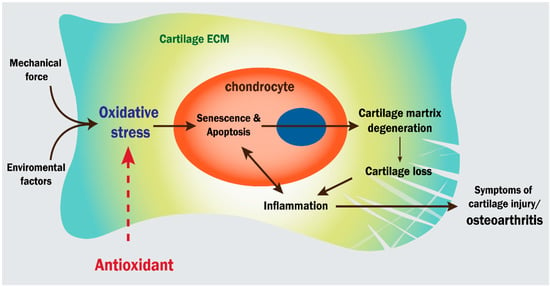
4.5. Cartilage Tissue
There is a limited ability for cartilage to regenerate itself [
143]. Degeneration of cartilage can be associated with ROS signaling, which is aggravated by inflammation, as seen in osteoarthritis (OA). Since cartilage lacks a vascular system, chondrocytes are dormant under normal circumstances and inhabit a hypoxic condition. A mitochondrial dysfunction triggers the activation of chondrocytes, increasing ROS production and resulting in more OA. Additionally, according to numerous studies, age can exacerbate oxidative stress, resulting in a loss of balance between ROS generation and antioxidative responses [
144]. Several antioxidants and free radical scavengers have been demonstrated to delay cartilage degradation (
Figure 6), including flavonoids (curcumin, quercetin, resveratrol), phenols (vitamin E), ubiquitin, thiols (thioredoxin and glutathione) [
145,
146], chondroitin sulfate (CS), xanthan gum [
147], dopamine melanin [
148], alginate, hyaluronic acid [
147,
149], fullerene and fullerol [
150], etc. Through the use of these materials, antioxidative substances, such as glutathione, catalase, nuclear factor erythroid-2-related factor 2 (Nrf2), and superoxide dismutase, can be increased and resulting in downregulating of ROS [
144].
Figure 6. Illustration of oxidative stress’ role in cartilage degeneration and osteoarthritis. Antioxidants interfere with this pathway, as indicated by the red arrow.
Researchers have extensively studied the antioxidant properties of black tea polyphenols, named theaflavins (TFs) [
151]. For example, Li et al. [
152] investigated the protective impacts of TFs on chondrocytes and discovered a reduction in ROS levels and apoptosis rates. CS is also an anti-inflammatory glycosaminoglycan found in soft tissues. Woo et al. [
153] have found that skate cartilage CS reduced inflammatory cytokine secretion and ROS levels in the murine cell line RAW 264.7 that had been treated with lipopolysaccharide.
4.5.1. TMJ Cartilage
Craniofacial skeletal defects primarily affect bony structures, whereas chondral and osteochondral deformities are less common but have serious consequences. TMJ tissue in adults contains articular cartilage [
161]. As a critical joint, TMJ maintains mandibular movements, including opening and closing the mouth. The TMJ is a ginglymoarthrodial joint consisting of a bone-cartilage interface and a bilateral synovial disc, whose function is heavily reliant upon the disc [
1]. Even with the rarity of cartilage defects, TMJ problems have significant clinical implications in maxillofacial surgery. TMJ structures are commonly degenerated or lost due to trauma, infection, or autoimmune disorders. In general, TMJ disorders are classified into arthritic, growth, and non-arthritic disorders. The first class is caused by inflammation and appears in patients with pain and facial deformities; treatment is aimed at removing risk factors and inflammatory markers. The second type appears in facial deformities, and treatment is aimed at removing the tumor by surgery. In the third type, mechanical derangement can play an important role. Some common clinical complaints in this type are luxation and disc replacement. It is important to reduce mechanical obstruction when treating this type of disorder. Consequently, treating TMJ defects can be challenging, depending on the causes of the defect [
161,
162]. Hence, researchers prefer to use natural, synthetic, and bio-compatible materials, such as antioxidants, in joint treatments to repair joint disorders [
163]. For healing TMJ disorders, some researchers and clinicians have tried to fabricate different prothesis to improve the oral cavity function. Regarding this, Pagano et al. [
163] evaluated the effect of different materials, such as PMMA resin (for making prosthesis), on the morphology, function, proliferation, and viability of the human keratinocyte. These cells have a critical role in creating a biological seal between the prosthesis and connective tissue that favors prosthesis adaptation to supporting tissues during joint treatments. Resin materials could induce p53 expression in human keratinocytes, preventing cell apoptosis and promoting cell viability against various damages in the oral cavity.
4.5.2. Auricular and Nasal Cartilage Regeneration
Auricular and nasal cartilage have an important role in maintaining their appearance and functionality. The nasal and auricular cartilage differ from the articular cartilage in the TMJ in terms of their structure and function [
1]. Auricular cartilage is elastic cartilage composed of a collagen type-II network and sulfated glycosaminoglycan. It does not self-repair or regenerate despite its high mechanical strength. Several auricular deformities can develop as a result of congenital defects, burns, and trauma, for which tissue engineering has been suggested as the most beneficial treatment [
171,
172].
An artificial auricular cartilage based on silk fibroin (SF)/polyvinyl alcohol (PVA) was developed by Lee et al. [
171]. This 3D cartilage with an ear shape was formed in rats after subcutaneous implantation of the chondrocyte-seeded hydrogel. Histological analysis confirmed the existence of mature cartilage with typical lacunar morphology, in vitro and in vivo. This 3D scaffold can be a basis for using antioxidants in auricular cartilage regeneration.
The condition of microtia, one of the ear disorders, refers to deformities of the external ear (auricle and pinna) caused by congenital birth defects. A tissue-engineered scaffold of ear pinna cartilage has been evaluated using various chemical treatment techniques to create a flexible and human-sized ear. In the study [
173], 5% Dimethyl sulfoxide (DMSO) (
v/
v) was utilized as an antioxidant treatment in one of the decellularization methods followed by freeze-thaw cycles. This method produced more durable pinna-shaped cartilage that was mechanically more stable and effective at removing antigenic material.
.6. Nerve Tissue Regeneration
Facial muscles are exceptionally functional for humans, have aesthetic functions, and have an important role in facial expression movements. The facial or seventh cranial nerve is the main nerve that controls all muscles that contributed to facial expression [
177]. Facial nerve paralysis is the most common neural disorder in the cranium, and it may be caused by several reasons [
177]. After nerve paralysis, trauma is the second most common type of neural disease in the cranium. Following post-traumatic recovery, inflammation makes extensive fibroconnective tissue and scars on the nerve tissue, and consequently, neuron tissue may lose its function [
178]. Nervous system injuries should be reduced to maximize nerve regeneration. Oxidative stress and greater numbers of oxygen-derived free radicals, including fatty acids and arachidonic acids from cell membranes, are considered to be harmful to the neuronal cells after axotomy. In this regard, antioxidants could be used as a strong defense system to remarkably combat the oxidative damage induced by nerve injuries [
178].
One of the short-lived, free radical gases in the central nervous system (CNS) is NO. NO may disrupt mitochondrial metabolism and induce apoptosis, and it acts as a neurotoxic agent during brain ischemia and hypoxia. NO is a toxic agent for cells and produces other deleterious free radicals in the nervous system. For this reason, Japanese scientists have discovered an influential antioxidant and free radical scavenger which increases the activity of the mitochondrial fraction SOD, which is called Tokishakuyakusan (TJ-23).
5. Conclusions
Oral and maxillofacial diseases are one of the most common disorders in the world which affect health and economic aspects of life. The application of graft materials and cell therapy strategies in the reconstruction of damaged organs can induce infection and increase the level of ROS products in the tissue environment and immune system of the host body, leading to the low-quality healing process of oral and maxillofacial defects. Hence, the application of antioxidant materials in combination with various scaffolds and medical hydrogels is highly recommended by scientists. Antioxidants can fight against several free radicals, including superoxide and hydroxyls, both directly and indirectly by altering the intracellular enzymes’ activities. They are classified into natural and synthetic, exogenous and endogenous, and enzymatic and non-enzymatic groups. As it is clear, oral and maxillofacial tissues consist of a wide range of tissues, such as craniofacial bone, periodontium, dental pulp, dentin, enamel, cartilage, and neuron. Both synthetic and natural antioxidant sources, especially polyphenol structures, are applied for large craniofacial bone defects and periodontal defects.
This entry is adapted from the peer-reviewed paper 10.3390/antiox12030594