Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Diabetic foot syndrome (DFS) is a complication associated with diabetes that has a strong negative impact, both medically and socio-economically.
- diabetic foot syndrome
- diabetes mellitus
- cardiovascular risk
1. Diabetes Mellitus and the Cardiovascular Continuum
Diabetes mellitus (DM) is one of the main medical challenges of the century, with multiple prognostic values representing a real cardiovascular risk factor responsible for increasing morbidity and mortality alike [1]. From 1550 BCE to the present day, advances in technology and the discovery of new therapeutic molecules have reduced the risk of potentially fatal complications leading to a reduced quality of life [2][3]. The widespread introduction of bariatric surgery, microbiome analysis as well as the deepening of pathophysiological mechanisms on the study of bile secretion and adipose tissue in terms of their effects on metabolism are some of the research directions in the field in recent years [4][5][6].
Epidemiological studies confirm the increasing prevalence of DM, especially in underdeveloped or developing countries, with the number of cases expected to double by 2045 [7][8]. From an economic point of view, the burden corresponds to more than 12% of the health systems budget, with most of the expenditure associated with the management of complications [9].
The psychological impact associated with the presence of diabetic foot syndrome (DFS) and its cardiovascular implications is negative from a psycho-emotional point of view [10]. Family support and understanding of the course of the disease are social factors that contribute to increased quality of life by improving adherence to treatment, combating depression and anxiety and maintaining a positive status regarding the outcome of the disease [11][12][13].
2. Cardio-Diabetology: The Role of Biomarkers and Inflammatory Molecules
Pathophysiological analysis of the adipovascular axis revealed the determinant role of inflammatory markers such as IL-6 and resistin in modulating cardiovascular risk in diabetic patients [14]. Patients with DF syndrome associate metabolic disorders that modulate the associated cardiovascular risk. Hyperglycemia causes axonal and microvascular injury over time. In addition, in diabetic patients, hypertriglyceridemia is a known independent risk factor for amputations [15][16].
Clinical studies in the field associate low serum levels of adiponectin and high levels of IL-6 with the development and progression of inflammatory mechanisms involved in the pathogenesis of diabetic ulcers. In diabetic patients, microalbuminuria correlates with serum IL-6 and adipocytokine levels, thus playing a dual role as a contributor to the progression of insulin resistance and the production of inflammatory cytokines [14]. Besides adiposity, oxidative stress, mitochondrial dysfunction, activation of the polyol pathway or accumulation of pro-inflammatory and advanced glycation end-products are pathophysiological mechanisms underlying the cardiovascular damage associated with DF syndrome [17][18][19][20].
Hyperglycemia affects ischemic preconditioning, being associated with elevated serum catecholamines, the presence of a no-reflow phenomenon, increased oxidative stress, pro-thrombotic status and inflammation (Figure 1) [21][22]. Hyperglycemia also leads to endothelial dysfunction, with activation of various metabolic pathways mediated by protein kinase C resulting in excessive production of reactive oxygen species [15]. Miric et al. [23] have shown that serum xanthine oxidase activity is an independent predictor for the occurrence of diabetic peripheral neuropathy, thus contributing to the development of DF syndrome. The administration of vitamin D for 12 weeks is accompanied by an improvement in carbohydrate metabolism, which also contributes to the healing process of diabetic ulcers [24]. Silent myocardial ischemia is common among diabetic patients, the presence of diabetic peripheral neuropathy being a risk factor associated with it; it has a screening role to detect patients at risk of developing an acute cardiovascular event [25].
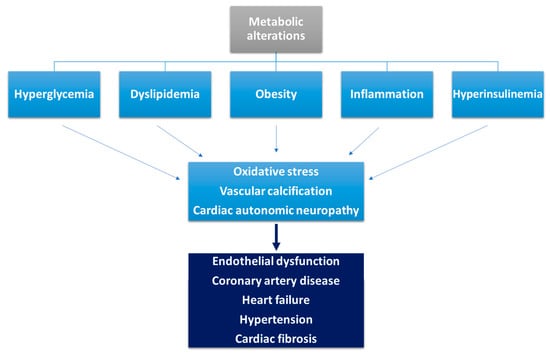
Figure 1. Pathophysiological mechanisms involved in the occurrence of cardiovascular disease in diabetic patients (adapted from [21]).
In addition to IL-6, other cytokines that modulate inflammatory processes have been identified such as leptin, tumor necrosis factor-α, plasminogen activator inhibitor, uric acid or oxidized low-density lipoproteins [26][27][28][29]. Afshinnia et al. [29] identified several lipid determinants with a role in the development and progression of diabetic neuropathy such as acylcarnitines, free fatty acids, phosphatidylcholines, and lysophosphatidylcholines, the presence of which can be identified up to 10 years earlier in a high titer. Some of these lipid compounds are also responsible for the development of cardiac autonomic dysfunction in patients with type 2 DM [30] and insulin resistance [31].
The identification of a serum cystatin C level above 0.735 mg/L is a potential biomarker for the identification of diabetes-associated complications and is correlated with the occurrence of DF and tissue loss in patients with type 2 DM [32].
In patients with type 2 diabetes, elevated homocysteine levels are associated with the presence of heart failure with a low ejection fraction and are an independent risk factor for all-cause mortality [33]. The connection between cardiac autonomic neuropathy and subclinical inflammation, with multiple prognostic implications on associated cardiovascular risk and morbidity, was examined in diabetic patients, with differential results depending on the type of molecule involved [34][35][36]. Heart rate variability is dependent on altered sympathetic and parasympathetic tone in young patients with DM, correlating with glycated hemoglobin values [37][38].
While IL-18 and soluble E-selectin are associated with reduced vagal activity, adiponectin can be used as a marker of decreased sympathetic activity [39]. Adiponectin has a dual, titer-dependent role, being both a cardioprotective hormone with an anti-inflammatory role and a marker of high cardiovascular risk through its association with an assessment of the risk of death [40][41]. Adiponectin also prevents cardiac remodeling after myocardial infarction and inhibits the action of the sympathetic nervous system on this pathophysiological process, also having a potential therapeutic role in these patients [42]. Zhu et al. [43] demonstrated that elevated serum adiponectin levels are an independent predictor of atrial fibrillation in women and men under 65 years old.
Peripheral somatic neuropathy contributes to the development of medial arterial calcification [44]. In diabetic patients, it plays a role in activating the receptor activator of nuclear factor kappa B ligand/osteoprotegerin signaling pathway that modulates the pathophysiological processes involved in the calcification of smooth muscle cells in the coronary arteries and peripheral limbs [16]. Advanced glycation end-products also contribute to the production of vascular calcification and, thus, to the progression of atherosclerotic lesions in diabetic patients [45][46].
Serum B-type natriuretic peptide levels correlate with the risk of onset and progression of diabetic neuropathy, but further clinical research is needed to unravel any pathophysiological implications. Data in the literature to date attest to the role of this cardiovascular biomarker in identifying and assessing the extent of neuropathic damage in diabetic patients. Based on the role of BNP to assess the presence of systolic and diastolic dysfunction as well as to assess the prognosis of patients with heart failure, the identification of a connection with DFS is of great clinical importance, as it can also assess the cardiovascular risk of patients without previously known cardiac pathology [47][48][49]. Yan et al. [50] demonstrated that serum BNP levels were higher in patients with type 2 DM and diabetic neuropathy compared to a cohort without microvascular damage (p = 0.001), while positively correlating with systolic blood pressure, serum creatinine, prevalence of diabetic ulcers (p = 0.039) and vibration perception threshold values (p = 0.021). Identification of a BNP value above 15.18 pg/mL has a sensitivity of 78.7% and a specificity of 48.2% in assessing the presence of diabetic neuropathy.
A recently published meta-analysis by Ramzi et al. [51] highlights that the presence of a serum N-terminal prohormone brain natriuretic peptide (NT-proBNP) level above 225 pg/mL correlates with a high risk of death from any cause among diabetic patients, while serum levels above 100 pg/mL are predictive of the occurrence of acute cardiovascular events. This biomarker, along with IL-6 and resistin, correlates with the presence of left ventricular dysfunction and left ventricular hypertrophy and can thus be used as non-invasive biomarkers for assessing cardiovascular risk in patients with DM [52].
3. Diabetic Foot Syndrome and Diabetic Cardiomyopathy
3.1. The Role of Artificial Intelligence in Assessing CVD Risk in DM
The applications of artificial intelligence in the medical field are becoming more and more extensive, being able nowadays to generate various models of cardiovascular risk assessment with both therapeutic and prognostic roles [53][54]. Imaging assessment of the ulcerative lesion is essential in order to identify an associated infection [55] and to provide accurate epidemiological data on the prevalence of DM [56]. Clinical studies in the literature have demonstrated that diabetic foot infections act as a cardiovascular marker based on a directly proportional correlation between the severity of infection and atherosclerotic lesions [15][57].
Machine Learning (ML) and Deep Learning (DL) algorithms have various applications in cardiology and diabetology [58][59], having both diagnostic and prognostic roles by identifying predictors associated with cardiovascular risk [60][61][62]. Technologies using artificial intelligence are based on the analysis of complex databases, and current data on diabetes-related cardiovascular risk assessment show non-linear connections between input predictors and the obtained risk. The advantage of using the aforementioned algorithms is obtaining intrinsic relationships between several predictors used simultaneously [63][64][65]. To date, several algorithms have been developed to assess associated cardiovascular risk [66][67][68], one such example being the one proposed by Jamthikar et al. [69] which, using carotid vascular Doppler assessment and the presence of traditional cardiovascular risk factors, can assess associated cardiovascular risk with superior accuracy to traditional methods of calculation. Based on the socio-economic importance of the complications associated with DFS, artificial intelligence algorithms have been developed to screen diabetic patients to identify risk factors for the development of ulcers using different optical sensors [70][71][72][73].
3.2. Predictive Risk Models for CVD Events in DM
The development of cardiovascular risk prediction models in diabetic patients is an extremely valuable clinical tool in the daily practice of cardio-diabetology [74]. Most risk prediction models to date are based on data from the Framingham Heart Study, in which diabetes is included as a risk factor [75][76]. This prediction model can be used among diabetic patients due to the underestimation of the associated cardiovascular risk, which has required the development of new prediction tools for this population [74][77]. The United Kingdom Prospective Diabetes Study and the ADVANCE study [78][79][80] identified a number of predictors which were demographic (age), associated with DM (time since diagnosis, glycosylated hemoglobin value) or derived from major cardiovascular risk factors.
Similarly, Mu et al. [81] developed an algorithm to predict the risk of an acute fatal or non-fatal cardiovascular event (especially acute myocardial infarction or stroke) in the next 10 years in patients with type 2 diabetes. Thus, the QRESEARCH risk estimator version 3 is superior to the Framingham risk score by using a much larger number of clinical–paraclinical parameters and has a much higher predictability among diabetic patients [82][83]. Based on the observation that approximately 50% of patients with cardiovascular disease do not associate with traditional cardiovascular risk factors, some clinical prediction models integrate biomarkers, comorbidities, polygenic-based scores [84][85] or metabolomic patterns [86][87][88].
Although various such prediction models have been developed, methodological issues, high risk of bias and lack of clinical validation studies are some of the main drawbacks identified that reinforce the need for extensive clinical research on large cohorts of patients before introduction into clinical practice [89].
3.3. Novel Therapeutic Targets
Advances in technology have enabled advanced clinical research, and various signaling pathways are currently being investigated for future use in the development of targeted therapeutic molecules [90]. P38 kinases are considered valuable and promising therapeutic targets in preventing the onset or progression of diabetic cardiomyopathy based on p38-MAPK-generated inhibition that resulted in improved inflammatory status and systolic function in previous animal studies of diabetic mice [91]. The use of phosphodiesterase type 5 inhibitors may prevent hyperglycemia-induced changes in cardiomyocyte gene expression, thereby counteracting the increased cyclic adenosine 5-monophosphate-responsive element modulator [92].
Modulation of nuclear factor erythroid 2-related factor 2 activity is associated with decreased inflammation and lipid accumulation or prevention of the development of fibrosis secondary to DM, thus representing a potential therapeutic target in patients with diabetic cardiomyopathy [93]. The use of exosomes developed from heat shock protein 20 has been shown in animal studies to modulate the secretory activity of cardiomyocytes [94]. microRNAs and the correction of intestinal dysbiosis interfere with the pathophysiological processes of diabetic cardiomyopathy [95]. In a previous clinical study, Katare et al. [96] demonstrated that anti-miR1 induces survival signals in cardiac progenitor cells or cardiomyocytes subjected to permanent hyperglycemic status.
Gene therapy is a very promising future research direction in relation to DM and DFS. To date, pre-clinical research with murine leukemia virus-1 (PIM-1) via cardiotropic serotype-9 adeno-associated virus (AAV) which increased PIM-1 expression and cardiac phosphoinositide 3-kinase using AAV6 has demonstrated in vitro prevention of cardiac apoptosis, fibrosis or development of heart failure and increased LV systolic function in diabetic mice [96][97][98].
The Charcot DF is frequently encountered in patients with DM, being one of the most disabling and severe complications [99]. The pathophysiology is complex and multifactorial, involving numerous signaling pathways and molecules that mediate diverse, interconnected processes that over time result in osteolysis and ultimately bone destruction [100][101]. One such example is the receptor activator of the NF-κB ligand receptor activator of NF-κB osteoprotegerin (RANKL-RANK-OPG) pathway which modulates inflammatory processes, its overexpression and activation being accompanied by increased osteoclast activity and osteolysis [102]. Taking into account the role of this signaling pathway in bone remodeling in patients with DFS, several therapeutic agents have been developed to act at different levels of the signaling pathway with the aim of halting the disabling progression of Charcot DF [102]. One such example is the administration of anti-RANKL monoclonal antibodies such as Denosumab, which—although it has, so far, been studied in small groups of patients—has encouraging results that justify further research in larger groups of patients [103][103][104][105].
In terms of wound healing, previous clinical and animal studies have demonstrated that ulcer-associated pro-inflammatory status, lack of ischemia correction and lesion maturation are therapeutic targets associated with improved wound healing in patients with DFS [106]. The neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are two easily measurable, reproducible inflammatory biomarkers with prognostic value in both the onset and progression of DFS. Among patients with DF-associated infections, elevated values of these biomarkers correlate with the occurrence of osteomyelitis, the need for amputation or septic complications [107][108].
This entry is adapted from the peer-reviewed paper 10.3390/app13105990
References
- Sakran, N.; Graham, Y.; Pintar, T.; Yang, W.; Kassir, R.; Willigendael, E.M.; Singhal, R.; Kooreman, Z.E.; Ramnarain, D.; Mahawar, K.; et al. The Many Faces of Diabetes. Is There a Need for Re-Classification? A Narrative Review. BMC Endocr. Disord. 2022, 22, 9.
- Zhang, G.Q.; Canner, J.K.; Haut, E.; Sherman, R.L.; Abularrage, C.J.; Hicks, C.W. Impact of Geographic Socioeconomic Disadvantage on Minor Amputation Outcomes in Patients with Diabetes. J. Surg. Res. 2021, 258, 38–46.
- Sharma, A.; Mittal, S.; Aggarwal, R.; Chauhan, M.K. Diabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and Treatment. Future J. Pharm. Sci. 2020, 6, 130.
- Jalilian, M.; Ahmadi Sarbarzeh, P.; Oubari, S. Factors Related to Severity of Diabetic Foot Ulcer: A Systematic Review. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 1835–1842.
- Awasthi, A.; Singh, S.K.; Kumar, B.; Gulati, M.; Kumar, R.; Wadhwa, S.; Khursheed, R.; Corrie, L.; Kr, A.; Kumar, R.; et al. Treatment Strategies Against Diabetic Foot Ulcer: Success so Far and the Road Ahead. Curr. Diabetes Rev. 2021, 17, 421–436.
- Rosinha, P.; Saraiva, M.; Ferreira, L.; Garrido, S.; Carvalho, A.; Freitas, C.; Amaral, C.; Costa, L.; Loureiro, L.; Carvalho, R. A Retrospective Cohort Study on Diabetic Foot Disease: Ascertainment of Ulcer Locations by Age Group. Cureus 2022, 14, e28189.
- Roglic WHO Global Report on Diabetes: A Summary. Available online: https://www.ijncd.org/article.asp?issn=2468-8827;year=2016;volume=1;issue=1;spage=3;epage=8;aulast=Roglic (accessed on 20 December 2022).
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res. Clin. Pract. 2019, 157, 107843.
- Shrestha, N.; Karki, K.; Poudyal, A.; Aryal, K.K.; Mahato, N.K.; Gautam, N.; Kc, D.; Gyanwali, P.; Dhimal, M.; Jha, A.K. Prevalence of Diabetes Mellitus and Associated Risk Factors in Nepal: Findings from a Nationwide Population-Based Survey. BMJ Open 2022, 12, e060750.
- Costa, D.; Ielapi, N.; Caprino, F.; Giannotta, N.; Sisinni, A.; Abramo, A.; Ssempijja, L.; Andreucci, M.; Bracale, U.M.; Serra, R. Social Aspects of Diabetic Foot: A Scoping Review. Soc. Sci. 2022, 11, 149.
- Yan, R.; Yu, F.; Strandlund, K.; Han, J.; Lei, N.; Song, Y. Analyzing Factors Affecting Quality of Life in Patients Hospitalized with Chronic Wound. Wound Repair Regen. 2021, 29, 70–78.
- Shankar, P.; Grewal, V.S.; Agrawal, S.; Nair, S.V. A Study on Quality of Life among Lower Limb Amputees at a Tertiary Prosthetic Rehabilitation Center. Med. J. Armed Forces India 2020, 76, 89–94.
- Pedras, S.; Vilhena, E.; Carvalho, R.; Pereira, M.G. Quality of Life Following a Lower Limb Amputation in Diabetic Patients: A Longitudinal and Multicenter Study. Psychiatry 2020, 83, 47–57.
- Tuttolomondo, A.; Maida, C.; Pinto, A. Diabetic Foot Syndrome as a Possible Cardiovascular Marker in Diabetic Patients. J. Diabetes Res. 2015, 2015, 268390.
- Dietrich, I.; Braga, G.A.; de Melo, F.G.; da Costa Silva Silva, A.C.C. The Diabetic Foot as a Proxy for Cardiovascular Events and Mortality Review. Curr. Atheroscler. Rep. 2017, 19, 44.
- Rani, V.; Deep, G.; Singh, R.K.; Palle, K.; Yadav, U.C.S. Oxidative Stress and Metabolic Disorders: Pathogenesis and Therapeutic Strategies. Life Sci. 2016, 148, 183–193.
- Pop-Busui, R.; Ang, L.; Holmes, C.; Gallagher, K.; Feldman, E.L. Inflammation as a Therapeutic Target for Diabetic Neuropathies. Curr. Diabetes Rep. 2016, 16, 29.
- Gómez-Marcos, M.Á.; Recio-Rodríguez, J.I.; Patino-Alonso, M.C.; Agudo-Conde, C.; Rodríguez-Sanchez, E.; Maderuelo-Fernandez, J.A.; Gómez-Sánchez, L.; Gomez-Sanchez, M.; García-Ortiz, L.; LOD-DIABETES Group. Evolution of Target Organ Damage and Haemodynamic Parameters over 4 Years in Patients with Increased Insulin Resistance: The LOD-DIABETES Prospective Observational Study. BMJ Open 2016, 6, e010400.
- De Favari Signini, É.; Castro, A.; Rehder-Santos, P.; Cristina Millan-Mattos, J.; Magalhães de Oliveira, J.; Minatel, V.; Bianca Falasco Pantoni, C.; Sobreiro Selistre de Araújo, H.; Fabrizzi, F.; Porta, A.; et al. Integrative Perspective of the Healthy Aging Process Considering the Metabolome, Cardiac Autonomic Modulation and Cardiorespiratory Fitness Evaluated in Age Groups. Sci. Rep. 2022, 12, 21314.
- Lanting, S.M.; Twigg, S.M.; Johnson, N.A.; Baker, M.K.; Caterson, I.D.; Chuter, V.H. Non-Invasive Lower Limb Small Arterial Measures Co-Segregate Strongly with Foot Complications in People with Diabetes. J. Diabetes Its Complicat. 2017, 31, 589–593.
- Tun, H.N. Cardio-Diabetology: New Subspecialty and Collaborative Work to Defeat the Burden of Deadly Duo. J. Cardiovasc. Med. Cardiol. 2018, 5, 081–084.
- Deedwania, P.; Kosiborod, M.; Barrett, E.; Ceriello, A.; Isley, W.; Mazzone, T.; Raskin, P. Hyperglycemia and Acute Coronary Syndrome: A Scientific Statement from the American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2008, 117, 1610–1619.
- Miric, D.J.; Kisic, B.M.; Filipovic-Danic, S.; Grbic, R.; Dragojevic, I.; Miric, M.B.; Puhalo-Sladoje, D. Xanthine Oxidase Activity in Type 2 Diabetes Mellitus Patients with and without Diabetic Peripheral Neuropathy. J. Diabetes Res. 2016, 2016, 4370490.
- Razzaghi, R.; Pourbagheri, H.; Momen-Heravi, M.; Bahmani, F.; Shadi, J.; Soleimani, Z.; Asemi, Z. The Effects of Vitamin D Supplementation on Wound Healing and Metabolic Status in Patients with Diabetic Foot Ulcer: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Diabetes Its Complicat. 2017, 31, 766–772.
- Baltzis, D.; Roustit, M.; Grammatikopoulou, M.G.; Katsaboukas, D.; Athanasiou, V.; Iakovou, I.; Veves, A.; Manes, C.; Trakatelli, M.-C. Diabetic Peripheral Neuropathy as a Predictor of Asymptomatic Myocardial Ischemia in Type 2 Diabetes Mellitus: A Cross-Sectional Study. Adv. Ther. 2016, 33, 1840–1847.
- Begun, A.; Morbach, S.; Rümenapf, G.; Icks, A. Study of Disease Progression and Relevant Risk Factors in Diabetic Foot Patients Using a Multistate Continuous-Time Markov Chain Model. PLoS ONE 2016, 11, e0147533.
- Callaghan, B.C.; Xia, R.; Banerjee, M.; de Rekeneire, N.; Harris, T.B.; Newman, A.B.; Satterfield, S.; Schwartz, A.V.; Vinik, A.I.; Feldman, E.L.; et al. Metabolic Syndrome Components Are Associated with Symptomatic Polyneuropathy Independent of Glycemic Status. Diabetes Care 2016, 39, 801–807.
- Smith, S.; Normahani, P.; Lane, T.; Hohenschurz-Schmidt, D.; Oliver, N.; Davies, A.H. Prevention and Management Strategies for Diabetic Neuropathy. Life 2022, 12, 1185.
- Afshinnia, F.; Reynolds, E.L.; Rajendiran, T.M.; Soni, T.; Byun, J.; Savelieff, M.G.; Looker, H.C.; Nelson, R.G.; Michailidis, G.; Callaghan, B.C.; et al. Serum Lipidomic Determinants of Human Diabetic Neuropathy in Type 2 Diabetes. Ann. Clin. Transl. Neurol. 2022, 9, 1392–1404.
- Ziegler, D.; Strom, A.; Straßburger, K.; Knebel, B.; Bönhof, G.J.; Kotzka, J.; Szendroedi, J.; Roden, M.; German Diabetes Study Group. Association of Cardiac Autonomic Dysfunction with Higher Levels of Plasma Lipid Metabolites in Recent-Onset Type 2 Diabetes. Diabetologia 2021, 64, 458–468.
- Semba, R.D.; Gonzalez-Freire, M.; Moaddel, R.; Sun, K.; Fabbri, E.; Zhang, P.; Carlson, O.D.; Khadeer, M.; Chia, C.W.; Salem, N.; et al. Altered Plasma Amino Acids and Lipids Associated with Abnormal Glucose Metabolism and Insulin Resistance in Older Adults. J. Clin. Endocrinol. Metab. 2018, 103, 3331–3339.
- Zhao, J.; Deng, W.; Zhang, Y.; Zheng, Y.; Zhou, L.; Boey, J.; Armstrong, D.G.; Yang, G.; Liang, Z.; Chen, B. Association between Serum Cystatin C and Diabetic Foot Ulceration in Patients with Type 2 Diabetes: A Cross-Sectional Study. J. Diabetes Res. 2016, 2016, e8029340.
- Wargny, M.; Croyal, M.; Ragot, S.; Gand, E.; Jacobi, D.; Trochu, J.-N.; Prieur, X.; Le May, C.; Goronflot, T.; Cariou, B.; et al. Nutritional Biomarkers and Heart Failure Requiring Hospitalization in Patients with Type 2 Diabetes: The SURDIAGENE Cohort. Cardiovasc. Diabetol. 2022, 21, 101.
- Herder, C.; Schamarek, I.; Nowotny, B.; Carstensen-Kirberg, M.; Straßburger, K.; Nowotny, P.; Kannenberg, J.M.; Strom, A.; Püttgen, S.; Müssig, K.; et al. Inflammatory Markers Are Associated with Cardiac Autonomic Dysfunction in Recent-Onset Type 2 Diabetes. Heart Br. Card. Soc. 2017, 103, 63–70.
- Herder, C.; Færch, K.; Carstensen-Kirberg, M.; Lowe, G.D.; Haapakoski, R.; Witte, D.R.; Brunner, E.J.; Roden, M.; Tabák, A.G.; Kivimäki, M.; et al. Biomarkers of Subclinical Inflammation and Increases in Glycaemia, Insulin Resistance and Beta-Cell Function in Non-Diabetic Individuals: The Whitehall II Study. Eur. J. Endocrinol. 2016, 175, 367–377.
- Sudo, S.Z.; Montagnoli, T.L.; Rocha, B.D.S.; Santos, A.D.; de Sá, M.P.L.; Zapata-Sudo, G. Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis. Biomedicines 2022, 10, 3258.
- Shah, A.S.; El Ghormli, L.; Vajravelu, M.E.; Bacha, F.; Farrell, R.M.; Gidding, S.S.; Levitt Katz, L.E.; Tryggestad, J.B.; White, N.H.; Urbina, E.M. Heart Rate Variability and Cardiac Autonomic Dysfunction: Prevalence, Risk Factors, and Relationship to Arterial Stiffness in the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) Study. Diabetes Care 2019, 42, 2143–2150.
- Benichou, T.; Pereira, B.; Mermillod, M.; Tauveron, I.; Pfabigan, D.; Maqdasy, S.; Dutheil, F. Heart Rate Variability in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0195166.
- Hansen, C.S.; Vistisen, D.; Jørgensen, M.E.; Witte, D.R.; Brunner, E.J.; Tabák, A.G.; Kivimäki, M.; Roden, M.; Malik, M.; Herder, C. Adiponectin, Biomarkers of Inflammation and Changes in Cardiac Autonomic Function: Whitehall II Study. Cardiovasc. Diabetol. 2017, 16, 153.
- Aljafary, M.A.; Al-Suhaimi, E.A. Adiponectin System (Rescue Hormone): The Missing Link between Metabolic and Cardiovascular Diseases. Pharmaceutics 2022, 14, 1430.
- Menzaghi, C.; Trischitta, V. The Adiponectin Paradox for All-Cause and Cardiovascular Mortality. Diabetes 2018, 67, 12–22.
- Zhou, Z.; Liu, C.; Xu, S.; Wang, J.; Guo, F.; Duan, S.; Deng, Q.; Sun, J.; Yu, F.; Zhou, Y.; et al. Metabolism Regulator Adiponectin Prevents Cardiac Remodeling and Ventricular Arrhythmias via Sympathetic Modulation in a Myocardial Infarction Model. Basic Res. Cardiol. 2022, 117, 34.
- Zhu, T.; Wang, Z.; Wang, S.; Hu, W.; Chen, H.; Xie, J.; Wang, M.; Ma, K.; Jiang, H. Association between Serum Adiponectin and Atrial Fibrillation: A Case-Control Study Stratified by Age and Gender. Cardiol. Res. Pract. 2021, 2021, 6633948.
- Jeffcoate, W.J.; Rasmussen, L.M.; Hofbauer, L.C.; Game, F.L. Medial Arterial Calcification in Diabetes and Its Relationship to Neuropathy. Diabetologia 2009, 52, 2478–2488.
- Jhamb, S.; Vangaveti, V.N.; Malabu, U.H. Genetic and Molecular Basis of Diabetic Foot Ulcers: Clinical Review. J. Tissue Viability 2016, 25, 229–236.
- Wang, Z.; Li, L.; Du, R.; Yan, J.; Liu, N.; Yuan, W.; Jiang, Y.; Xu, S.; Ye, F.; Yuan, G.; et al. CML/RAGE Signal Induces Calcification Cascade in Diabetes. Diabetol. Metab. Syndr. 2016, 8, 83.
- Allman, K.C.; Stevens, M.J.; Wieland, D.M.; Hutchins, G.D.; Wolfe, E.R.; Greene, D.A.; Schwaiger, M. Noninvasive Assessment of Cardiac Diabetic Neuropathy by Carbon-11 Hydroxyephedrine and Positron Emission Tomography. J. Am. Coll. Cardiol. 1993, 22, 1425–1432.
- Hamano, K.; Nakadaira, I.; Suzuki, J.; Gonai, M. N-Terminal Fragment of Probrain Natriuretic Peptide Is Associated with Diabetes Microvascular Complications in Type 2 Diabetes. Vasc. Health Risk Manag. 2014, 10, 585–589.
- Jouni, H.; Rodeheffer, R.J.; Kullo, I.J. Increased Serum N-Terminal Pro–B-Type Natriuretic Peptide Levels in Patients with Medial Arterial Calcification and Poorly Compressible Leg Arteries. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 197–202.
- Yan, P.; Wan, Q.; Zhang, Z.; Xu, Y.; Miao, Y.; Chen, P.; Gao, C. Association between Circulating B-Type Natriuretic Peptide and Diabetic Peripheral Neuropathy: A Cross-Sectional Study of a Chinese Type 2 Diabetic Population. J. Diabetes Res. 2020, 2020, 3436549.
- Ramzi, Z.S. N-Terminal Prohormone Brain Natriuretic Peptide as a Prognostic Biomarker for the Risk of Complications in Type 2 Diabetes: A Systematic Review and Meta-Analysis. Lab. Med. 2022, lmac119.
- Ghanem, S.E.; Abdel-Samiee, M.; Torky, M.H.; Gaafar, A.; Mohamed, S.M.; Eldin, G.M.M.S.; Awad, S.M.; Diab, K.A.; ELsabaawy, D.M.; Yehia, S.A.; et al. Role of Resistin, IL-6 and NH2-Terminal Portion ProBNP in the Pathogenesis of Cardiac Disease in Type 2 Diabetes Mellitus. BMJ Open Diabetes Res. Care 2020, 8, e001206.
- Truslow, J.G.; Goto, S.; Homilius, M.; Mow, C.; Higgins, J.M.; MacRae, C.A.; Deo, R.C. Cardiovascular Risk Assessment Using Artificial Intelligence-Enabled Event Adjudication and Hematologic Predictors. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e008007.
- Saba, L.; Biswas, M.; Kuppili, V.; Cuadrado Godia, E.; Suri, H.S.; Edla, D.R.; Omerzu, T.; Laird, J.R.; Khanna, N.N.; Mavrogeni, S.; et al. The Present and Future of Deep Learning in Radiology. Eur. J. Radiol. 2019, 114, 14–24.
- Anaya-Isaza, A.; Zequera-Diaz, M. Fourier Transform-Based Data Augmentation in Deep Learning for Diabetic Foot Thermograph Classification. Biocybern. Biomed. Eng. 2022, 42, 437–452.
- Goyal, M.; Reeves, N.D.; Davison, A.K.; Rajbhandari, S.; Spragg, J.; Yap, M.H. DFUNet: Convolutional Neural Networks for Diabetic Foot Ulcer Classification. IEEE Trans. Emerg. Top. Comput. Intell. 2020, 4, 728–739.
- Mishra, S.C.; Chhatbar, K.C.; Kashikar, A.; Mehndiratta, A. Diabetic Foot. BMJ 2017, 359, j5064.
- Maniruzzaman, M.; Kumar, N.; Menhazul Abedin, M.; Shaykhul Islam, M.; Suri, H.S.; El-Baz, A.S.; Suri, J.S. Comparative Approaches for Classification of Diabetes Mellitus Data: Machine Learning Paradigm. Comput. Methods Programs Biomed. 2017, 152, 23–34.
- Maniruzzaman, M.; Rahman, M.J.; Al-MehediHasan, M.; Suri, H.S.; Abedin, M.M.; El-Baz, A.; Suri, J.S. Accurate Diabetes Risk Stratification Using Machine Learning: Role of Missing Value and Outliers. J. Med. Syst. 2018, 42, 92.
- Khanna, N.N.; Maindarkar, M.A.; Viswanathan, V.; Puvvula, A.; Paul, S.; Bhagawati, M.; Ahluwalia, P.; Ruzsa, Z.; Sharma, A.; Kolluri, R.; et al. Cardiovascular/Stroke Risk Stratification in Diabetic Foot Infection Patients Using Deep Learning-Based Artificial Intelligence: An Investigative Study. J. Clin. Med. 2022, 11, 6844.
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358.
- El-Baz, A.; Suri, J.S. Big Data in Multimodal Medical Imaging; CRC Press: Boca Raton, FL, USA, 2019; ISBN 978-1-351-38073-7.
- Goldstein, B.A.; Navar, A.M.; Carter, R.E. Moving beyond Regression Techniques in Cardiovascular Risk Prediction: Applying Machine Learning to Address Analytic Challenges. Eur. Heart J. 2017, 38, 1805–1814.
- Ming, C.; Viassolo, V.; Probst-Hensch, N.; Chappuis, P.O.; Dinov, I.D.; Katapodi, M.C. Machine Learning Techniques for Personalized Breast Cancer Risk Prediction: Comparison with the BCRAT and BOADICEA Models. Breast Cancer Res. 2019, 21, 75.
- Khanna, N.N.; Maindarkar, M.; Puvvula, A.; Paul, S.; Bhagawati, M.; Ahluwalia, P.; Ruzsa, Z.; Sharma, A.; Munjral, S.; Kolluri, R.; et al. Vascular Implications of COVID-19: Role of Radiological Imaging, Artificial Intelligence, and Tissue Characterization: A Special Report. J. Cardiovasc. Dev. Dis. 2022, 9, 268.
- Jamthikar, A.; Gupta, D.; Khanna, N.N.; Saba, L.; Laird, J.R.; Suri, J.S. Cardiovascular/Stroke Risk Prevention: A New Machine Learning Framework Integrating Carotid Ultrasound Image-Based Phenotypes and Its Harmonics with Conventional Risk Factors. Indian Heart J. 2020, 72, 258–264.
- Jamthikar, A.D.; Gupta, D.; Saba, L.; Khanna, N.N.; Viskovic, K.; Mavrogeni, S.; Laird, J.R.; Sattar, N.; Johri, A.M.; Pareek, G.; et al. Artificial Intelligence Framework for Predictive Cardiovascular and Stroke Risk Assessment Models: A Narrative Review of Integrated Approaches Using Carotid Ultrasound. Comput. Biol. Med. 2020, 126, 104043.
- Derevitskii, I.V.; Kovalchuk, S.V. Machine Learning-Based Predictive Modeling of Complications of Chronic Diabetes. Procedia Comput. Sci. 2020, 178, 274–283.
- Jamthikar, A.D.; Gupta, D.; Mantella, L.E.; Saba, L.; Laird, J.R.; Johri, A.M.; Suri, J.S. Multiclass Machine Learning vs. Conventional Calculators for Stroke/CVD Risk Assessment Using Carotid Plaque Predictors with Coronary Angiography Scores as Gold Standard: A 500 Participants Study. Int. J. Cardiovasc. Imaging 2021, 37, 1171–1187.
- Chemello, G.; Salvatori, B.; Morettini, M.; Tura, A. Artificial Intelligence Methodologies Applied to Technologies for Screening, Diagnosis and Care of the Diabetic Foot: A Narrative Review. Biosensors 2022, 12, 985.
- Howard, T.; Ahluwalia, R.; Papanas, N. The Advent of Artificial Intelligence in Diabetic Foot Medicine: A New Horizon, a New Order, or a False Dawn? Int. J. Low. Extrem. Wounds 2021.
- Kaselimi, M.; Protopapadakis, E.; Doulamis, A.; Doulamis, N. A Review of Non-Invasive Sensors and Artificial Intelligence Models for Diabetic Foot Monitoring. Front. Physiol. 2022, 13, 924546.
- Yap, M.H.; Hachiuma, R.; Alavi, A.; Brüngel, R.; Cassidy, B.; Goyal, M.; Zhu, H.; Rückert, J.; Olshansky, M.; Huang, X.; et al. Deep Learning in Diabetic Foot Ulcers Detection: A Comprehensive Evaluation. Comput. Biol. Med. 2021, 135, 104596.
- Young, J.B.; Gauthier-Loiselle, M.; Bailey, R.A.; Manceur, A.M.; Lefebvre, P.; Greenberg, M.; Lafeuille, M.-H.; Duh, M.S.; Bookhart, B.; Wysham, C.H. Development of Predictive Risk Models for Major Adverse Cardiovascular Events among Patients with Type 2 Diabetes Mellitus Using Health Insurance Claims Data. Cardiovasc. Diabetol. 2018, 17, 118.
- Wilson, P.W.F.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847.
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–753.
- Coleman, R.L.; Stevens, R.J.; Retnakaran, R.; Holman, R.R. Framingham, SCORE, and DECODE Risk Equations Do Not Provide Reliable Cardiovascular Risk Estimates in Type 2 Diabetes. Diabetes Care 2007, 30, 1292–1293.
- Kengne, A.P.; Patel, A.; Colagiuri, S.; Heller, S.; Hamet, P.; Marre, M.; Pan, C.Y.; Zoungas, S.; Grobbee, D.E.; Neal, B.; et al. The Framingham and UK Prospective Diabetes Study (UKPDS) Risk Equations Do Not Reliably Estimate the Probability of Cardiovascular Events in a Large Ethnically Diverse Sample of Patients with Diabetes: The Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation (ADVANCE) Study. Diabetologia 2010, 53, 821–831.
- Kothari, V.; Stevens, R.J.; Adler, A.I.; Stratton, I.M.; Manley, S.E.; Neil, H.A.; Holman, R.R. UKPDS 60: Risk of Stroke in Type 2 Diabetes Estimated by the UK Prospective Diabetes Study Risk Engine. Stroke 2002, 33, 1776–1781.
- Stevens, R.J.; Kothari, V.; Adler, A.I.; Stratton, I.M.; United Kingdom Prospective Diabetes Study (UKPDS) Group. The UKPDS Risk Engine: A Model for the Risk of Coronary Heart Disease in Type II Diabetes (UKPDS 56). Clin. Sci. 2001, 101, 671–679.
- Mu, X.; Wu, A.; Hu, H.; Zhou, H.; Yang, M. Assessment of QRISK3 as a Predictor of Cardiovascular Disease Events in Type 2 Diabetes Mellitus. Front. Endocrinol. 2022, 13, 1077632.
- Hippisley-Cox, J.; Coupland, C.; Brindle, P. Development and Validation of QRISK3 Risk Prediction Algorithms to Estimate Future Risk of Cardiovascular Disease: Prospective Cohort Study. BMJ 2017, 357, j2099.
- Livingstone, S.J.; Guthrie, B.; Donnan, P.T.; Thompson, A.; Morales, D.R. Predictive Performance of a Competing Risk Cardiovascular Prediction Tool CRISK Compared to QRISK3 in Older People and Those with Comorbidity: Population Cohort Study. BMC Med. 2022, 20, 152.
- Khera, A.V.; Chaffin, M.; Aragam, K.G.; Haas, M.E.; Roselli, C.; Choi, S.H.; Natarajan, P.; Lander, E.S.; Lubitz, S.A.; Ellinor, P.T.; et al. Genome-Wide Polygenic Scores for Common Diseases Identify Individuals with Risk Equivalent to Monogenic Mutations. Nat. Genet. 2018, 50, 1219–1224.
- Khera, A.V.; Emdin, C.A.; Drake, I.; Natarajan, P.; Bick, A.G.; Cook, N.R.; Chasman, D.I.; Baber, U.; Mehran, R.; Rader, D.J.; et al. Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease. N. Engl. J. Med. 2016, 375, 2349–2358.
- Rezaee, M.; Putrenko, I.; Takeh, A.; Ganna, A.; Ingelsson, E. Development and Validation of Risk Prediction Models for Multiple Cardiovascular Diseases and Type 2 Diabetes. PLoS ONE 2020, 15, e0235758.
- Ruiz-Canela, M.; Hruby, A.; Clish, C.B.; Liang, L.; Martínez-González, M.A.; Hu, F.B. Comprehensive Metabolomic Profiling and Incident Cardiovascular Disease: A Systematic Review. J. Am. Heart Assoc. 2017, 6, e005705.
- Ganna, A.; Salihovic, S.; Sundström, J.; Broeckling, C.D.; Hedman, A.K.; Magnusson, P.K.E.; Pedersen, N.L.; Larsson, A.; Siegbahn, A.; Zilmer, M.; et al. Large-Scale Metabolomic Profiling Identifies Novel Biomarkers for Incident Coronary Heart Disease. PLoS Genet. 2014, 10, e1004801.
- Galbete, A.; Tamayo, I.; Librero, J.; Enguita-Germán, M.; Cambra, K.; Ibáñez-Beroiz, B. Cardiovascular Risk in Patients with Type 2 Diabetes: A Systematic Review of Prediction Models. Diabetes Res. Clin. Pract. 2022, 184, 109089.
- Grubić Rotkvić, P.; Planinić, Z.; Liberati Pršo, A.-M.; Šikić, J.; Galić, E.; Rotkvić, L. The Mystery of Diabetic Cardiomyopathy: From Early Concepts and Underlying Mechanisms to Novel Therapeutic Possibilities. Int. J. Mol. Sci. 2021, 22, 5973.
- Westermann, D.; Rutschow, S.; Van Linthout, S.; Linderer, A.; Bücker-Gärtner, C.; Sobirey, M.; Riad, A.; Pauschinger, M.; Schultheiss, H.-P.; Tschöpe, C. Inhibition of P38 Mitogen-Activated Protein Kinase Attenuates Left Ventricular Dysfunction by Mediating pro-Inflammatory Cardiac Cytokine Levels in a Mouse Model of Diabetes Mellitus. Diabetologia 2006, 49, 2507–2513.
- Barbati, S.A.; Colussi, C.; Bacci, L.; Aiello, A.; Re, A.; Stigliano, E.; Isidori, A.M.; Grassi, C.; Pontecorvi, A.; Farsetti, A.; et al. Transcription Factor CREM Mediates High Glucose Response in Cardiomyocytes and in a Male Mouse Model of Prolonged Hyperglycemia. Endocrinology 2017, 158, 2391–2405.
- Zhang, Z.; Wang, S.; Zhou, S.; Yan, X.; Wang, Y.; Chen, J.; Mellen, N.; Kong, M.; Gu, J.; Tan, Y.; et al. Sulforaphane Prevents the Development of Cardiomyopathy in Type 2 Diabetic Mice Probably by Reversing Oxidative Stress-Induced Inhibition of LKB1/AMPK Pathway. J. Mol. Cell. Cardiol. 2014, 77, 42–52.
- Wang, X.; Gu, H.; Huang, W.; Peng, J.; Li, Y.; Yang, L.; Qin, D.; Essandoh, K.; Wang, Y.; Peng, T.; et al. Hsp20-Mediated Activation of Exosome Biogenesis in Cardiomyocytes Improves Cardiac Function and Angiogenesis in Diabetic Mice. Diabetes 2016, 65, 3111–3128.
- Bastin, M.; Andreelli, F. The Gut Microbiota and Diabetic Cardiomyopathy in Humans. Diabetes Metab. 2020, 46, 197–202.
- Katare, R.; Caporali, A.; Zentilin, L.; Avolio, E.; Sala-Newby, G.; Oikawa, A.; Cesselli, D.; Beltrami, A.P.; Giacca, M.; Emanueli, C.; et al. Intravenous Gene Therapy with PIM-1 Via a Cardiotropic Viral Vector Halts the Progression of Diabetic Cardiomyopathy Through Promotion of Prosurvival Signaling. Circ. Res. 2011, 108, 1238–1251.
- Levelt, E.; Gulsin, G.; Neubauer, S.; McCann, G.P. MECHANISMS IN ENDOCRINOLOGY: Diabetic Cardiomyopathy: Pathophysiology and Potential Metabolic Interventions State of the Art Review. Eur. J. Endocrinol. 2018, 178, R127–R139.
- Huynh, K.; Bernardo, B.C.; McMullen, J.R.; Ritchie, R.H. Diabetic Cardiomyopathy: Mechanisms and New Treatment Strategies Targeting Antioxidant Signaling Pathways. Pharmacol. Ther. 2014, 142, 375–415.
- Jeffcoate, W.J.; Game, F.; Cavanagh, P.R. The Role of Proinflammatory Cytokines in the Cause of Neuropathic Osteoarthropathy (Acute Charcot Foot) in Diabetes. Lancet 2005, 366, 2058–2061.
- Marmolejo, V.S.; Arnold, J.F.; Ponticello, M.; Andersen, C.A. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am. Fam. Physician 2018, 97, 594–599.
- Schweitzer, M.; Rockhill, S. Conservative Management of Charcot Neuroarthropathy. Clin. Podiatr. Med. Surg. 2022, 39, 585–594.
- Greco, T.; Mascio, A.; Comisi, C.; Polichetti, C.; Caravelli, S.; Mosca, M.; Mondanelli, N.; Troiano, E.; Maccauro, G.; Perisano, C. RANKL-RANK-OPG Pathway in Charcot Diabetic Foot: Pathophysiology and Clinical-Therapeutic Implications. Int. J. Mol. Sci. 2023, 24, 3014.
- Carvès, S.; Bourgeon-Ghittori, M.; Henry, J.; Belkhir, R.; Besson, F.L.; Levante, S.; Mariette, X.; Seror, R. Denosumab in Active Charcot Neuro-Osteoarthropathy of the Foot. Jt. Bone Spine 2021, 88, 105241.
- Busch-Westbroek, T.E.; Delpeut, K.; Balm, R.; Bus, S.A.; Schepers, T.; Peters, E.J.; Smithuis, F.F.; Maas, M.; Nieuwdorp, M. Effect of Single Dose of RANKL Antibody Treatment on Acute Charcot Neuro-Osteoarthropathy of the Foot. Diabetes Care 2018, 41, e21–e22.
- Shofler, D.; Hamedani, E.; Seun, J.; Sathananthan, A.; Katsaros, E.; Liggan, L.; Kang, S.; Pham, C. Investigating the Use of Denosumab in the Treatment of Acute Charcot Neuroarthropathy. J. Foot Ankle Surg. 2021, 60, 354–357.
- Golledge, J.; Thanigaimani, S. Novel Therapeutic Targets for Diabetes-Related Wounds or Ulcers: An Update on Preclinical and Clinical Research. Expert Opin. Ther. Targets 2021, 25, 1061–1075.
- Serban, D.; Papanas, N.; Dascalu, A.M.; Kempler, P.; Raz, I.; Rizvi, A.A.; Rizzo, M.; Tudor, C.; Silviu Tudosie, M.; Tanasescu, D.; et al. Significance of Neutrophil to Lymphocyte Ratio (NLR) and Platelet Lymphocyte Ratio (PLR) in Diabetic Foot Ulcer and Potential New Therapeutic Targets. Int. J. Low. Extrem. Wounds 2021.
- Chen, W.; Chen, K.; Xu, Z.; Hu, Y.; Liu, Y.; Liu, W.; Hu, X.; Ye, T.; Hong, J.; Zhu, H.; et al. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Predict Mortality in Patients with Diabetic Foot Ulcers Undergoing Amputations. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 821–829.
This entry is offline, you can click here to edit this entry!
