Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 1 by Christina Barja-Fidalgo.
Bone is a mineralized connective tissue that is constantly renewed to maintain its mechanical properties. Osteoblasts are responsible for extracellular matrix synthesis, while osteoclasts resorb damaged bone, and the osteocytes have a regulatory role in this process, releasing growth factors and other proteins. A balanced activity among these actors is necessary for healthy bone remodeling. In obesity, several mechanisms may trigger incorrect remodeling, increasing bone resorption to the detriment of bone formation rates.
- obesity
- inflammation
- adipose tissue
- extracellular vesicles
- adipokines
- osteoblast
- osteoclast
- osteocyte
- Nc-RNAS
1. Introduction
Bone is a dynamic calcified tissue involved in physical support, visceral protection, mineral storage, hematopoiesis, and endocrine activity [28,29,30][1][2][3]. Bone tissue renewal is a very balanced process where hormones, cytokines, and growth factors regulate bone formation and bone resorption [31,32][4][5]. Osteoblasts are bone-forming cells derived from mesenchymal stem cells (MSCs). They produce organic extracellular matrix elements and promote their further mineralization [33,34][6][7]. On counterbalance, osteoclasts are multinucleated cells derived from the monocyte/macrophage lineage, able to resorb bone by enzymatic digestion. Bone resorption occurs predominantly by cathepsin-K and MMP-9 actions in an acidic microenvironment [35,36][8][9]. A fine balance between osteoclast and osteoblast activities controls healthy bone remodeling [37][10]. Additionally, osteocytes are bone cells sensitive to mechanical loads that orchestrate regulatory mechanisms to enable bone turnover. The process involves the activation of signaling routes, such as WNT, and the release of mediators, such as bone morphogenetic proteins (BMP), nitric oxide (NO), prostaglandin E2 (PGE2), sclerostatin, FGF-23 and RANKL [38,39][11][12].
Due to the systemic inflammatory condition, obesity can disrupt the balance of bone remodeling, dysregulating bone homeostasis and allowing bone loss. Two main pathways drive this condition: (i) the release of proinflammatory mediators from obese adipose tissue that reduces osteoblast activity while increasing osteoclast differentiation and resorption; and (ii) the differentiation of MSCs towards osteogenic lineage is reduced during obesity, while adipogenic differentiation is enhanced [40,41,42][13][14][15]. Nevertheless, other systemic alterations may also have relevance in this process, including oxidative stress, gut and microbiota physiology, vesiculated or free Nc-RNA, and hormonal changes.
2. Proinflammatory Cytokines in Bone Metabolism
Adipose tissue expansion increases pro-inflammatory cytokine expression and secretion by hypertrophic adipocytes and infiltration of M1-like macrophages and other immune cells (Figure 1). Cytokines, such as TNF-α, IL-1β, and IL-6 released by obese adipose tissue can interfere with bone cell homeostasis. Acting in isolation or in concert, they trigger intracellular signaling pathways that may lead to bone loss.
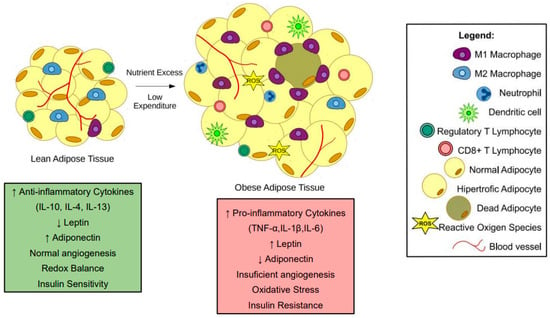
Figure 1. Changes in adipose tissue during obesity. In lean subjects, adipose tissue presents an anti-inflammatory state. Moreover, adipocytes present average triglyceride storage. During obesity, nutrient excess and low expenditure promote a hypertrophic state in adipocytes. The hypertrophic adipocytes and pro-inflammatory immune cells, such as M1-like macrophages, neutrophils, and CD8+ T cells, contribute to a low-grade inflammatory state in subjects with obesity. Most of the pro-inflammatory factors released by obese adipose tissue interfere with bone cells leading to bone loss.
TNF-α is a well know enhancer of osteoclastogenesis [43][16]. In vitro experiments showed that stimulation of osteoclast precursors with TNF-α and RANKL increased the number of multinucleated TRAP-positive cells [44,45][17][18]. Additionally, in vivo treatment with TNF-α increased the osteoclast numbers in mice calvaria [46][19]. In this context, Shinohara and collaborators (2015) demonstrated that TNF-α-induced osteoclast formation depends on double-stranded RNA-dependent protein kinase [44][17]. Other studies showed that TNF-α increased c-kit+/c-fms+ osteoclast precursors in high-fat diet (HFD) fed obese mice and augmented RANK expression in bone marrow macrophages [47,48][20][21]. Increased RANKL expression in TNF-α stimulated osteocytes contributed to osteoclast differentiation in vitro and in vivo [43][16].
In parallel, TNF-α can also modify osteoblast activity: In MC3T3-E1, osteoblasts or MSCs induced osteogenic differentiation, TNF-α decreased the expression of osteogenic transcription factors RUNX2 and Osterix, reducing the mineralization and expression of bone markers, osteocalcin (OCN), alkaline phosphatase (ALP), and bone sialoprotein (BSP) [49,50,51,52,53][22][23][24][25][26]. These effects are mediated by the inflammatory transcription factors ATF3 [51][24] and Nf-κB [53][26]. TNF-α upregulated miR-150-3p in osteoblasts, decreasing β-catenin expression, a key transcription factor for osteogenesis [52][25]. This cytokine can affect osteoblast viability, promoting apoptosis [54][27] and increasing MMP-9 expression [55][28]. TNF-β, another TNF family member, also showed deleterious impacts on bones, reducing RUNX2, Type I collagen (Col1A), OCN, and integrin β1 expression and decreasing mineralization in MSCs cultured in the osteogenic medium [56][29].
In vivo studies have demonstrated TNF-α-related bone loss in obese mice [57,58][30][31]. A palmitic acid-enriched HFD enhanced TNF-α serum levels in obese mice, parallel with a decrease in bone turnover markers, P1NP e CTX1 [57][30]. Furthermore, mice fed with a HFD presented lower trabeculae numbers and thickness and reduced trabecular bone volume, compared to lean controls. Obese TNF-α knockout mice showed less bone loss, a reduced number of femoral osteoclasts, and enhanced RUNX2 expression in MSCs, compared to HFD wildtype [58][31].
Increased circulating levels of IL-1β are a hallmark of the chronic, low-grade inflammation associated with obesity and related diseases [59][32]. IL-1β is a known inducer of osteoclast migration and resorption [60,61,62][33][34][35]. Combined with RANKL, IL-1β significantly increased osteoclast formation in vitro, enhancing TRAP staining and the expression of osteoclast markers, cathepsin K, OSCAR, NFATC1, Cfos, and DC-STAMP [61,62,63,64,65][34][35][36][37][38]. Though IL-1β increases osteoclast formation, its effect depends on the precursor subsets. Comparing the early myeloid blasts and monocytes, IL-1β increased osteoclast formation and cell diameter, mostly in myeloid blasts [61][34]. IL-1β can also harm other bone cells, inducing apoptosis in the MLO-Y4 osteocytic cell line [66][39] and MC3T3-E1 osteoblasts [67][40]. Osteoblasts stimulated with IL-1β exhibited a lower migration capacity [68][41] and released more IL-6 [69][42]. Indirectly, IL-1β promoted an osteoclastic supportive phenotype in osteocytes, enhancing RANKL expression [67][40]. Apart from triggering specific mechanisms, IL-1β also shares some signaling mechanisms with TNF-α. Lee and collaborators (2017) have shown that treatment with IL-1β and TNF-α raised CCR7 expression in both precursors and differentiated osteoclasts, increasing their migratory activity toward CCL19 and CCL21 chemokines upregulated in rheumatoid arthritis [60][33]. Adseverin, an actin-binding protein that regulates cell differentiation and fusion, modulates IL-1β- and TNF-α-induced osteoclastogenesis [63][36]. Nevertheless, Hah and collaborators (2013) showed that both IL-1β and TNF-α increased ALP activity and mineralization of periosteal osteoblasts without modifying RUNX2 and OCN expression [70][43].
Although osteoblasts are characterized by their activity of extracellular matrix synthesis, IL-1β enhanced metalloprotease production by osteoblasts. Ozeki and collaborators (2014) demonstrated that this cytokine potentiated MMP13 expression through ADAM28 upregulation in osteoblast-like cells [67][40]. Yang and collaborators (2011) have shown that IL-1β amplified the expression of MMP-9 and MMP-13 in osteoblasts [71][44], further contributing to bone destruction in inflammatory diseases. IL-1β may also interfere with hormonal factors produced by bone tissue, such as FGF23, which orchestrates vitamin D and phosphate serum levels [72,73][45][46]. An imbalance in FGF23 regulation, mainly due to its exceeding action, leads to a pathological mineralization process that weakens bones [74][47]. Corroborating in vivo studies that described greater serum levels of FGF23 in IL-1β treated mice [73][46], the treatment of bone slices in vitro increased hormone secretion [72][45]. Additionally, He and collaborators (2020) demonstrated an association between IL-1β genetic variants and osteoporosis predisposition [75][48]. IL-1β variants rs1143627, rs16944, and rs1143623 are related to elevated susceptibility to osteoporosis, especially in women older than 60 or with a BMI greater than 24 kg/m2 [75][48]. In obese mice fed a 10% corn oil-based diet, Halade and colleagues (2011) observed that bone marrow adipose tissue secreted higher concentrations of IL-1β, TNF-A, and IL-6, which increased the expression of RANK-L in stromal cells favoring osteoclast formation [76][49].
IL-6 is a cytokine with pleiotropic actions secreted by several cell types, including adipocytes, and its plasma levels are significantly upregulated during obesity [77][50]. In bone tissue, such as IL-1β and TNF-α, IL-6 indirectly stimulated osteoclastogenesis, increasing RANKL expression in osteocytes and osteoblasts [78,79,80][51][52][53]. Using an in vitro model of bone loss, neutralizing IL-6 antibodies had protective effects against osteoporosis, enhancing bone mineral density, trabecular number, and thickness [81][54]. IL-6 inhibition decreased osteoblasts’ RANKL/OPG ratio and osteoclast differentiation in a microgravity model [81][54]. IL-6 also inhibited osteoblast activity by downregulating the expression of the osteogenic transcription factor RUNX2 [79,81,82][52][54][55]. IL-6 knockout osteoblasts presented higher ALP activity and RUNX2 expression than wild-type ones. Moreover, obese IL-6 knockout mice exhibited increased trabecular bone volume, number, and thickness than HFD wild-type mice [82][55].
Few publications have described a combined effect of proinflammatory cytokines on bone cells. Stimulation with IL-1β, TNF-α, and IL-6 together in bone chips enhanced IL- 1β, IL-6, IL-8, TNF- α, FGF23, SOST, and OPG expression by bone cells [83][56]. Yokota and collaborators (2013) showed that TNF-α and IL-6 supracalvarial injections in mice raised osteoclast formation, compared to isolated injections of both cytokines [84][57]. Together, these data suggest the pro-osteoclastic and anti-osteoblastic effects of proinflammatory cytokines and their importance in obesity-associated bone loss (Figure 2).
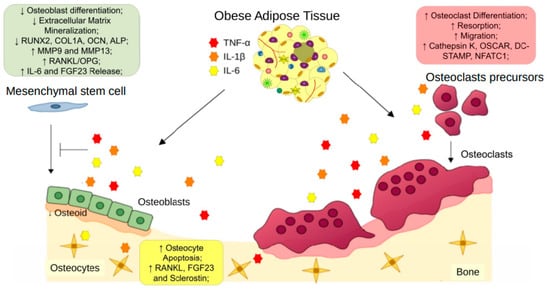
Figure 2. Obese adipose tissue-derived proinflammatory cytokines on bone remodeling. Pro-inflammatory cytokines, such as TNF-α, IL-6, and IL-1β, released by obese adipose tissue, exert effects on osteoclast precursors, increasing osteoclast differentiation and resorption. Moreover, these cytokines reduce the osteogenic differentiation of mesenchymal stem cells and compromise osteoblast bone formation. TNF-α, IL-6, and IL-1β also promote apoptosis and increased expression of osteoclast stimulation factors by osteocytes. The unbalanced activities between osteoblasts and osteoclasts induce osteoporosis.
References
- Florencio-Silva, R.; da Silva Sasso, G.R.; Sasso-Cerri, E.; Simões, M.J.; Cerri, P.S. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed. Res. Int. 2015, 2015, 421746.
- Czekanska, E.; Stoddart, M.; Richards, R.; Hayes, J. In search of an osteoblast cell model for in vitro research. Eur. Cells Mater. 2012, 24, 1–17.
- Guntur, A.R.; Rosen, C.J. Bone As An Endocrine Organ. Endocr. Pr. 2012, 18, 758–762.
- Xiao, W.; Wang, Y.; Pacios, S.; Li, S.; Graves, D.T. Cellular and Molecular Aspects of Bone Remodeling. Front. Oral. Biol. 2016, 18, 9–16.
- Buck, D.W.; Dumanian, G.A. Bone Biology and Physiology. Plast. Reconstr. Surg. 2012, 129, 1314–1320.
- Roeder, E.; Matthews, B.G.; Kalajzic, I. Visual reporters for study of the osteoblast lineage. Bone 2016, 92, 189–195.
- Hou, Z.; Wang, Z.; Tao, Y.; Bai, J.; Yu, B.; Shen, J.; Sun, H.; Xiao, L.; Xu, Y.; Zhou, J.; et al. KLF2 regulates osteoblast differentiation by targeting of Runx2. Lab. Investig. 2019, 99, 271–280.
- Gu, J.; Tong, X.-S.; Chen, G.-H.; Wang, D.; Chen, Y.; Yuan, Y.; Liu, X.-Z.; Bian, J.-C.; Liu, Z.-P. Effects of 1α,25-(OH)2D3 on the formation and activity of osteoclasts in RAW264.7 cells. J. Steroid Biochem. Mol. Biol. 2015, 152, 25–33.
- Chiu, Y.-H.; Ritchlin, C.T. DC-STAMP: A Key Regulator in Osteoclast Differentiation. J. Cell. Physiol. 2016, 231, 2402–2407.
- Chen, X.; Wang, Z.; Duan, N.; Zhu, G.; Schwarz, E.M.; Xie, C. Osteoblast–osteoclast interactions. Connect. Tissue Res. 2017, 59, 99–107.
- Hemmatian, H.; Bakker, A.D.; Klein-Nulend, J.; Van Lenthe, G.H. Aging, Osteocytes, and Mechanotransduction. Curr. Osteoporos. Rep. 2017, 15, 401–411.
- Tresguerres, F.; Torres, J.; López-Quiles, J.; Hernández, G.; Vega, J.; Tresguerres, I. The osteocyte: A multifunctional cell within the bone. Ann. Anat.-Anat. Anz. 2019, 227, 151422.
- Shapses, S.A.; Pop, L.C.; Wang, Y. Obesity is a concern for bone health with aging. Nutr. Res. 2017, 39, 1–13.
- Cao, J.J. Effects of obesity on bone metabolism. J. Orthop. Surg. Res. 2011, 6, 30.
- Fintini, D.; Cianfarani, S.; Cofini, M.; Andreoletti, A.; Ubertini, G.M.; Cappa, M.; Manco, M. The Bones of Children with Obesity. Front. Endocrinol. 2020, 11, 200.
- Marahleh, A.; Kitaura, H.; Ohori, F.; Kishikawa, A.; Ogawa, S.; Shen, W.-R.; Qi, J.; Noguchi, T.; Nara, Y.; Mizoguchi, I. TNF-α Directly Enhances Osteocyte RANKL Expression and Promotes Osteoclast Formation. Front. Immunol. 2019, 10, 2925.
- Shinohara, H.; Teramachi, J.; Okamura, H.; Yang, D.; Nagata, T.; Haneji, T. Double Stranded RNA-Dependent Protein Kinase is Necessary for TNF-α-Induced Osteoclast Formation In Vitro and In Vivo. J. Cell. Biochem. 2015, 116, 1957–1967.
- Luo, G.; Li, F.; Li, X.; Wang, Z.-G.; Zhang, B. TNF-α and RANKL promote osteoclastogenesis by upregulating RANK via the NF-κB pathway. Mol. Med. Rep. 2018, 17, 6605–6611.
- Ohori, F.; Kitaura, H.; Ogawa, S.; Shen, W.-R.; Qi, J.; Noguchi, T.; Marahleh, A.; Nara, Y.; Pramusita, A.; Mizoguchi, I. IL-33 Inhibits TNF-α-Induced Osteoclastogenesis and Bone Resorption. Int. J. Mol. Sci. 2020, 21, 1130.
- Shu, L.; Beier, E.; Sheu, T.; Zhang, H.; Zuscik, M.J.; Puzas, E.J.; Boyce, B.F.; Mooney, R.A.; Xing, L. High-Fat Diet Causes Bone Loss in Young Mice by Promoting Osteoclastogenesis Through Alteration of the Bone Marrow Environment. Calcif. Tissue Int. 2015, 96, 313–323.
- Noguchi, T.; Kitaura, H.; Ogawa, S.; Qi, J.; Shen, W.-R.; Ohori, F.; Marahleh, A.; Nara, Y.; Pramusita, A.; Mizoguchi, I. TNF-α stimulates the expression of RANK during orthodontic tooth movement. Arch. Oral Biol. 2020, 117, 104796.
- Min, H.-Y.; Son, H.-E.; Jang, W.-G. Alpha-pinene promotes osteoblast differentiation and attenuates TNFα-induced inhibition of differentiation in MC3T3-E1 pre-osteoblasts. Clin. Exp. Pharmacol. Physiol. 2019, 47, 831–837.
- Abuna, R.P.; De Oliveira, F.S.; Santos, T.D.S.; Guerra, T.R.; Rosa, A.L.; Beloti, M.M. Participation of TNF-α in Inhibitory Effects of Adipocytes on Osteoblast Differentiation. J. Cell. Physiol. 2015, 231, 204–214.
- Jeong, B.-C. ATF3 mediates the inhibitory action of TNF-α on osteoblast differentiation through the JNK signaling pathway. Biochem. Biophys. Res. Commun. 2018, 499, 696–701.
- Wang, N.; Zhou, Z.; Wu, T.; Liu, W.; Yin, P.; Pan, C.; Yu, X. TNF-α-induced NF-κB activation upregulates microRNA-150-3p and inhibits osteogenesis of mesenchymal stem cells by targeting β-catenin. Open Biol. 2016, 6, 150258.
- Ye, X.; Huang, H.; Zhao, N.; Zhang, J.; Yang, P. Inhibition of Runx2 signaling by TNF-α in ST2 murine bone marrow stromal cells undergoing osteogenic differentiation. Vitr. Cell. Dev. Biol.-Anim. 2016, 52, 1026–1033.
- Bin, G.; Cuifang, W.; Bo, Z.; Jing, W.; Jin, J.; Xiaoyi, T.; Cong, C.; Yonggang, C.; Liping, A.; Jinglin, M.; et al. Fluid shear stress inhibits TNF-α-induced osteoblast apoptosis via ERK5 signaling pathway. Biochem. Biophys. Res. Commun. 2015, 466, 117–123.
- Tsai, C.-L.; Chen, W.-C.; Hsieh, H.-L.; Chi, P.-L.; Hsiao, L.-D.; Yang, C.-M. TNF-α induces matrix metalloproteinase-9-dependent soluble intercellular adhesion molecule-1 release via TRAF2-mediated MAPKs and NF-κB activation in osteoblast-like MC3T3-E1 cells. J. Biomed. Sci. 2014, 21, 12.
- Constanze, B.; Popper, B.; Aggarwal, B.B.; Shakibaei, M. Evidence that TNF-β suppresses osteoblast differentiation of mesenchymal stem cells and resveratrol reverses it through modulation of NF-κB, Sirt1 and Runx2. Cell Tissue Res. 2020, 381, 83–98.
- Muluke, M.; Gold, T.; Kiefhaber, K.; Al-Sahli, A.; Celenti, R.; Jiang, H.; Cremers, S.; Van Dyke, T.; Schulze-Späte, U. Diet-Induced Obesity and Its Differential Impact on Periodontal Bone Loss. J. Dent. Res. 2015, 95, 223–229.
- Zhang, K.; Wang, C.; Chen, Y.; Ji, X.; Chen, X.; Tian, L.; Yu, X. Preservation of high-fat diet-induced femoral trabecular bone loss through genetic target of TNF-α. Endocrine 2015, 50, 239–249.
- Galozzi, P.; Bindoli, S.; Doria, A.; Sfriso, P. The revisited role of interleukin-1 alpha and beta in autoimmune and inflammatory disorders and in comorbidities. Autoimmun. Rev. 2021, 20, 102785.
- Lee, J.; Park, C.; Kim, H.J.; Lee, Y.D.; Lee, Z.H.; Song, Y.W.; Kim, H.-H. Stimulation of osteoclast migration and bone resorption by C–C chemokine ligands 19 and 21. Exp. Mol. Med. 2017, 49, e358.
- Cao, Y.; Jansen, I.D.C.; Sprangers, S.; Stap, J.; Leenen, P.J.; Everts, V.; de Vries, T.J. IL-1β differently stimulates proliferation and multinucleation of distinct mouse bone marrow osteoclast precursor subsets. J. Leukoc. Biol. 2016, 100, 513–523.
- Son, H.S.; Lee, J.; Lee, H.I.; Kim, N.; Jo, Y.-J.; Lee, G.-R.; Hong, S.-E.; Kwon, M.; Kim, N.Y.; Kim, H.J.; et al. Benzydamine inhibits osteoclast differentiation and bone resorption via down-regulation of interleukin-1 expression. Acta Pharm. Sin. B 2019, 10, 462–474.
- Wang, Y.; Galli, M.; Silver, A.S.; Lee, W.; Song, Y.; Mei, Y.M.; Bachus, C.; Glogauer, M.; McCulloch, C.A. IL1β and TNFα promote RANKL-dependent adseverin expression and osteoclastogenesis. J. Cell Sci. 2018, 131, jcs213967.
- Lee, W.-S.; Lee, E.-G.; Sung, M.-S.; Choi, Y.-J.; Yoo, W.-H. Atorvastatin inhibits osteoclast differentiation by suppressing NF-κB and MAPK signaling during IL-1β-induced osteoclastogenesis. Korean J. Intern. Med. 2018, 33, 397–406.
- Moon, S.-J.; Ahn, I.E.; Jung, H.; Yi, H.; Kim, J.; Kim, Y.; Kwok, S.-K.; Park, K.-S.; Min, J.-K.; Park, S.-H.; et al. Temporal differential effects of proinflammatory cytokines on osteoclastogenesis. Int. J. Mol. Med. 2013, 31, 769–777.
- Qu, X.; Mei, J.; Yu, Z.; Zhai, Z.; Qiao, H.; Dai, K. Lenalidomide regulates osteocytes fate and related osteoclastogenesis via IL-1β/NF-κB/RANKL signaling. Biochem. Biophys. Res. Commun. 2018, 501, 547–555.
- Ozeki, N.; Kawai, R.; Yamaguchi, H.; Hiyama, T.; Kinoshita, K.; Hase, N.; Nakata, K.; Kondo, A.; Mogi, M.; Nakamura, H. RETRACTED: IL-1β-induced matrix metalloproteinase-13 is activated by a disintegrin and metalloprotease-28-regulated proliferation of human osteoblast-like cells. Exp. Cell Res. 2014, 323, 165–177.
- Hengartner, N.-E.; Fiedler, J.; Ignatius, A.; Brenner, R.E. IL-1β Inhibits Human Osteoblast Migration. Mol. Med. 2013, 19, 36–42.
- Lazzerini, P.E.; Capperucci, C.; Spreafico, A.; Capecchi, P.L.; Niccolini, S.; Ferrata, P.; Frediani, B.; Galeazzi, M.; Laghi-Pasini, F. Rosuvastatin inhibits spontaneous and IL-1β-induced interleukin-6 production from human cultured osteoblastic cells. Jt. Bone Spine 2013, 80, 195–200.
- Hah, Y.-S.; Kang, H.-G.; Cho, H.-Y.; Shin, S.-H.; Kim, U.-K.; Park, B.-W.; Lee, S.-I.; Rho, G.-J.; Kim, J.-R.; Byun, J.-H. JNK signaling plays an important role in the effects of TNF-α and IL-1β on in vitro osteoblastic differentiation of cultured human periosteal-derived cells. Mol. Biol. Rep. 2013, 40, 4869–4881.
- Yang, H.; Liu, Q.; Ahn, J.H.; Kim, S.B.; Kim, Y.C.; Sung, S.H.; Hwang, B.Y.; Lee, M.K. Luteolin downregulates IL-1β-induced MMP-9 and -13 expressions in osteoblasts via inhibition of ERK signalling pathway. J. Enzym. Inhib. Med. Chem. 2011, 27, 261–266.
- McKnight, Q.; Jenkins, S.; Li, X.; Nelson, T.; Marlier, A.; Cantley, L.G.; Finberg, K.E.; Fretz, J.A. IL-1β Drives Production of FGF-23 at the Onset of Chronic Kidney Disease in Mice. J. Bone Miner. Res. 2020, 35, 1352–1362.
- Yamazaki, M.; Kawai, M.; Miyagawa, K.; Ohata, Y.; Tachikawa, K.; Kinoshita, S.; Nishino, J.; Ozono, K.; Michigami, T. Interleukin-1-induced acute bone resorption facilitates the secretion of fibroblast growth factor 23 into the circulation. J. Bone Miner. Metab. 2014, 33, 342–354.
- Rupp, T.; Butscheidt, S.; Vettorazzi, E.; Oheim, R.; Barvencik, F.; Amling, M.; Rolvien, T. High FGF23 levels are associated with impaired trabecular bone microarchitecture in patients with osteoporosis. Osteoporos. Int. 2019, 30, 1655–1662.
- He, Z.; Sun, Y.; Wu, J.; Xiong, Z.; Zhang, S.; Liu, J.; Liu, Y.; Li, H.; Jin, T.; Yang, Y.; et al. Evaluation of genetic variants in IL-1B and its interaction with the predisposition of osteoporosis in the northwestern Chinese Han population. J. Gene Med. 2020, 22, e3214.
- Halade, G.V.; El Jamali, A.; Williams, P.J.; Fajardo, R.J.; Fernandes, G. Obesity-mediated inflammatory microenvironment stimulates osteoclastogenesis and bone loss in mice. Exp. Gerontol. 2011, 46, 43–52.
- Hirano, T. IL-6 in inflammation, autoimmunity and cancer. Int. Immunol. 2020, 33, 127–148.
- Wu, Q.; Zhou, X.; Huang, D.; Ji, Y.; Kang, F. IL-6 Enhances Osteocyte-Mediated Osteoclastogenesis by Promoting JAK2 and RANKL Activity In Vitro. Cell. Physiol. Biochem. 2017, 41, 1360–1369.
- Bakker, A.; Kulkarni, R.; Klein-Nulend, J.; Lems, W. IL-6 Alters Osteocyte Signaling toward Osteoblasts but Not Osteoclasts. J. Dent. Res. 2014, 93, 394–399.
- McGregor, N.E.; Murat, M.; Elango, J.; Poulton, I.J.; Walker, E.C.; Crimeen-Irwin, B.; Ho, P.W.M.; Gooi, J.H.; Martin, T.J.; Sims, N.A. IL-6 exhibits both cis- and trans-signaling in osteocytes and osteoblasts, but only trans-signaling promotes bone formation and osteoclastogenesis. J. Biol. Chem. 2019, 294, 7850–7863.
- He, B.; Yin, X.; Hao, D.; Zhang, X.; Zhang, Z.; Zhang, K.; Yang, X. Blockade of IL-6 alleviates bone loss induced by modeled microgravity in mice. Can. J. Physiol. Pharmacol. 2020, 98, 678–683.
- Wang, C.; Tian, L.; Zhang, K.; Chen, Y.; Chen, X.; Xie, Y.; Zhao, Q.; Yu, X. Interleukin-6 gene knockout antagonizes high-fat-induced trabecular bone loss. J. Mol. Endocrinol. 2016, 57, 161–170.
- Pathak, J.L.; Bakker, A.D.; Luyten, F.P.; Verschueren, P.; Lems, W.F.; Klein-Nulend, J.; Bravenboer, N. Systemic Inflammation Affects Human Osteocyte-Specific Protein and Cytokine Expression. Calcif. Tissue Int. 2016, 98, 596–608.
- Yokota, K.; Sato, K.; Miyazaki, T.; Kitaura, H.; Kayama, H.; Miyoshi, F.; Araki, Y.; Akiyama, Y.; Takeda, K.; Mimura, T. Combination of Tumor Necrosis Factor α and Interleukin-6 Induces Mouse Osteoclast-like Cells with Bone Resorption Activity Both In Vitro and In Vivo. Arthritis Rheumatol. 2013, 66, 121–129.
More
