Essential oils (EOs) are mixtures of volatile molecules endowed with health-promoting biological activities that go beyond their role as aromas and natural preservatives and can be exploited to develop functional foods and diet supplements. Some of the potential health benefit of human diet supplementation with EOs are in the area of: (1) irritable bowel syndrome; (2) inflammatory bowel disease; (3) regulation of microbiota; (4) gastroprotection; (5) hepatoprotection; (6) protection of the urinary tract and diuresis; (7) management of metabolic disorders including hyperglycemia and hyperlipidemia; (8) anti-inflammatory and pain control; (9) immunomodulation and protection from influenza; and (10) neuroprotection and modulation of mood and cognitive performance.
- essential oils
- health
- diet supplements
- nutraceutical
- functional food
1. Introduction
2. Composition of Essential Oils
Essential oils are—sometimes complex—mixtures of volatile apolar or moderately polar molecules comprising heterogenous structures that can, nonetheless, be clustered in classes of components bearing internal structural similarity and a common biosynthetic route. Many such components are hydrocarbons; i.e., they contain only C and H elements, while others also contain O (often referred to as oxygenated compounds) and more rarely N or S. Classification on the basis of the elemental composition is, however, less useful than following their biosynthetic route that dictates the overall structure. Along this line, most of the typical EO components belong to one of the two main families: terpenoids and phenylpropanoids [5]. Terpenoids (Figure 1) are biosynthesized though the mevalonate pathway and are built by formally connecting isoprene units as C5 building blocks. (The actual building blocks are isopentenyl pyrophosphate and dimethylallyl pyrophosphate.) The majority of compounds contain two or three isoprene units and are called terpenes or sesquiterpenes, respectively. They owe their name to the wrong initial identification of the C10 unit as the recurrent building block, which was called terpene; therefore, the C15 molecules were identified as containing one and a half terpenes (from the Latin “semis” = half + “atque” = and, contracted to “sesqui”) (Figure 1) [5]. Although the plant contains components up to C30 (6 isoprene units), those larger than C15 (i.e., diterpenes and triterpenes) are rarely present in the EO since they are not sufficiently volatile to pass into the distillate. Formally, the term “terpene” refers only to hydrocarbons, i.e., those components having no heteroatoms, while the term “terpenoids” broadens to include oxygenated or heteroatoms-containing compounds although in common practice, this distinction is normally overlooked. A selection of common terpenoid components found in EOs is shown in Figure 2.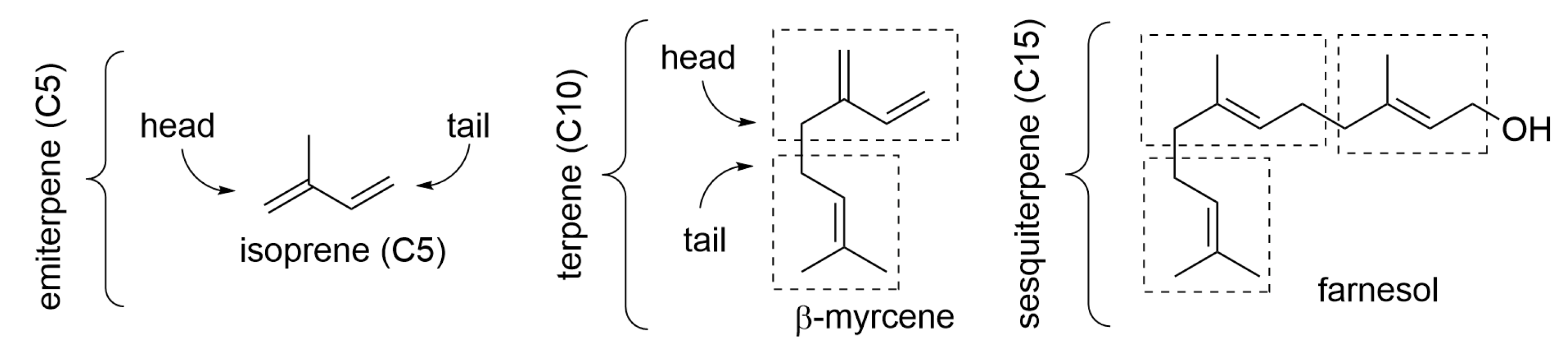

3. Essential Oils Helpful in the Irritable Bowel Syndrome (IBS)
4. Essential Oils Helpful in Inflammatory Bowel Disease (IBD) and in the Prevention of Colorectal Cancer (CRC)
Inflammatory bowel disease (IBD) is a chronic inflammatory disease of the gastrointestinal tract that comprises two phenotypical conditions, namely ulcerative colitis (UC) and Crohn’s disease (CD). It affects approximately 1.6 million individuals in USA (0.5% of population, with a growth of 70,000 new cases every year) and 0.2% of the European population [51][17], with a growing number of cases in South America, the Middle East, and Asia. IBD is distinct from IBS, and it is characterized by GI symptoms such as rectal bleeding and diarrhea, bloating, abdominal cramping, pain, reduced appetite, unintended weight loss, and fatigue. Although causes are incompletely understood, IBD is normally associated with an over-reactive immune system and is related to genetic and environmental factors. IBD is also associated with a 30-fold higher risk of developing colorectal cancer (CRC) owing to the massive proliferation required to repair the intestinal tissue injury [52][18]. Diet and diet supplements are actively investigated as complementary therapeutic approaches to reduce the need for pharmacotherapy or surgery. Several dietary medicinal plants and essential oils have shown promising results; however, no dietary intervention has been clinically validated yet. Animal studies can offer a meaningful insight using well-established translational models in rats or mice, such as treatment with acetic acid (AA) or dextran sulfate sodium (DSS) or oxazolone (OZ) to induce ulcerative colitis (UC) or with trinitrobenzenesulfonic acid (TNBS) to model Crohn’s disease (CD) [52][18]. A recent review analyzed the intestinal anti-inflammatory and antioxidant activity (modulation of markers TNF-α, IL-1, IL-7, IL-10, IL-11, IL-12, and mRNA of NF-kβ, MPO, COX-2, and PPARγ) of several essential oils orally administered in the rat translational model for ulcerative colitis (UC) or for Crohn’s disease (CD), finding that Zanthoxylum bungeanum (rich in terpinen-4-ol, eucalyptol, xanthoxylin); Zanthoxylum myriacanthum (limonene, α- and β-phellandrene, α-pinene, o-cymene); and Curcuma longa (curcumin) where effective on UC at doses in the range 20–80 mg/Kg b.w, while Foeniculum vulgare (trans-anethole, fenchone, methyl chavicol, limonene); Zingiber officinale (zingiberene, α-curcumene, β-bisabolene, α-sesquiphellandrene); Ocimum basilicum (linalool, β-pinene, trans-verbenol, α-terpinolene); and Cymbopogon martini (geraniol) required a minimal dose of 200, 100, 160, and 120 mg/Kg b.w, respectively [52][18].5. Essential Oils in Probiotic Food and Supplements for Regulation of Gut Microflora
According to the World Health Organization, probiotics are living strains of microorganisms to be consumed in suitable amounts in order to provide health benefits to the host by modulating activity and composition of gut microbiota [71][19]. These types of microorganisms consist mainly of bacteria but also include yeasts, which are naturally present in fermented foods, may be added to other food products, and are available as dietary supplements. Probiotics act usually in the gastrointestinal tract, and their viability depends on the baseline microbiota, probiotic strain, and gastrointestinal tract region [72][20]. They may influence the intestinal microbiota during their temporary colonization in the gut mucosa so that they must be consumed nearly on a daily basis to provide a real positive impact [73][21]. For this reason, food represents a preferred way to administer probiotics, followed by enriched dietary supplements. Probiotics should not be confused with prebiotics, which are typically complex carbohydrates (such as inulin and other fructo-oligosaccharides) that microorganisms in the gastrointestinal tract use as metabolic fuel [74][22]. Commercial products containing both prebiotic sugars and probiotic organisms are often called “synbiotics”. Some essential oils have greater minimum inhibitory concentration (MIC) values for probiotics compared to pathogens. Such a phenomenon makes it possible that both probiotics and essential oil are administered together to treat pathogenic infection in the human gut [75][23]. They can be combined to form essential oil-flavored fermented milk products, such as flavored curd beverages or flavored yogurt. Among fermented foods, yogurt represents a key example of source of probiotic microorganisms such as Lactobacillus delbrueckii subsp. bulgaricus and Streptococcus thermophiles, which should survive intestinal transit in order to be claimed as probiotic. Yogurt consumption promotes probiotic bacterial growth by changing the gastrointestinal tract bacteria and also supports immune system contributing to the overall health and preventing age-related weight gain [76][24]. Other fermented foods that contain probiotic microorganisms include beverages such as fermented milk. In an independent study, three beverages were prepared with probiotic curd with varying concentration of essential oils of Coleus aromaticus, Rama tulasi, and Shyama tulasi [83][25]. These beverages were then grown with common enteric pathogens in equal concentration, measured by CFU count. The sample beverages were found to be highly effective in inhibiting the growth of the pathogen. The shelf life of the beverages was also found to be significantly higher than for normal probiotics. The test results can be interpreted as the beverage’s capacity for prevention of enteric pathogens [83][25]. The above examples clearly show that both probiotics and essential oils have a great potential in terms of their beneficial effect against microbial gut infection, and their combined use can afford even more beneficial functional food [75][23].6. Essential Oils for Gastric Protection and to Alleviate Peptic Ulcer
Peptic ulcer is a chronic pathology affecting a relevant portion of the population worldwide (as much as 10% for at least some time). Based on the main localization of lesions, it is often classified into gastric ulcer or duodenal ulcer. It is a multifactor condition that can be triggered by several causes, including the use of anti-inflammatory drugs, abuse of alcohol, inappropriate diet, and emotional stress. There is strong association between gastric and duodenal ulcers and the infection by Helicobacter pylori, which causes inflammation of the mucosa [84][26]. Studies have shown that pro-inflammatory cytokines and oxidative homeostasis have a key influence in the onset of gastric ulcer, which sees an overboost of oxidative stress counterbalanced by activation of the nuclear factor-erythroid-2-related factor 2 (Nrf2) signaling pathway, which upregulates the biosynthesis of endogenous antioxidant enzymes [85][27]. The EO of Thymus hirtus ssp. algeriensis Boiss, a thyme species distributed in North Africa and locally used as culinary herb, was shown to express relevant healing of HCl/ethanol-induced ulcers in rats [89][28]. Oral administration at doses of 54, 117, and 180 mg/kg b.w. showed marked decrease in the number of ulcer lesions and of the ulcer index, accompanied by higher pH and mucus production. Biochemical analysis also revealed increased antioxidant defenses in the treated vs. control groups, as witnessed by increased levels of GSH, SOD, CAT, and GPx, accompanied by a decrease in TBARS. While these findings are somewhat different from those recorded with other Thymus species, they are explained by a markedly different composition of the EO, which contained linalool, 1,8-cyneol, camphor, and viridiflorol as the main components and conceivably acted with an anti-inflammatory [55][29] via the induction of antioxidant enzymes as well as by increased secretion of mucus, i.e., by the increasing of gastric mucosal defensive mechanisms [68][30].7. Essential Oils Useful in the Management of Metabolic Disorders
Inhibition of carbohydrate hydrolyzing enzymes α-amilase and α-glucosidase is a key target for oral hypoglycemic treatments for type 2 diabetes mellitus (T2DM). While pancreatic α-amylase hydrolyzes starch into oligosaccharides, these are further hydrolyzed by intestinal α-glucosidase into glucose, which is finally absorbed into systemic circulation, raising the plasma glucose level. In T2DM subjects with reduced glucose tolerance, postprandial plasma glucose rise can be smoothed by enzyme inhibitors, which slow down carbohydrate digestion, ameliorating their condition. In a comparative study on several terpenoid EO components, citral was the only one that showed mild inhibition of α-amilase compared to the reference drug acarbose. Instead, several monoterpenes (10 mM) showed inhibition of α-glucosidase with the following order of potency: (R)-(+)-limonene = (S)-(−)-perillyl alcohol > α-terpineol, while (R)-(+)-β-citronellol, terpinolene, citral, (R)-(−)-linalool, nerol, geraniol, and (S)-(−)-β-citronellol exerted weaker inhibition, and (L)-menthol and γ-terpinene did not show any significant α-glucosidase-inhibitory activity [107][31]. The same terpenes were tested for stimulation of glucose uptake in 3T3-L1 adipocytes, which represents another strategy to reduce glucose plasma levels. Geraniol, citral, limonene, and (R)-(+)-β-citronellol (1 μM) had the highest activity, while nerol, (S)-(−)-perillyl alcohol, γ-terpinene, and α-terpineol were weaker stimulants; and (S)-(−)-b-citronellol, terpinolene, and linalool did not affect the glucose uptake [86][32]. Thus, to a different degree, several terpenes of widespread presence in EOs, such as limonene, citral, and citronellol, have hypoglycemic activity, which helps rationalize the efficacy recorded for the whole oils.
High levels of circulating total cholesterol (TC), of low-density lipoprotein-cholesterol (LDL-C), and of plasma triglycerides along with low levels of high-density lipoprotein-cholesterol represent well-established risk factors for cardiovascular disease and might be associated with diabetes or dysregulated glycemic parameters in metabolic syndrome. Treating these unbalances with suitable dietary approaches is not less important than addressing hyperglycemia alone. Some EOs, most notably green and black cumin, show parallel reduction of lipidemic factors along with glycemic.
8. Essential Oils to Protect Liver Function and Stimulate Digestion
In classical aromatherapy several essential oils are used to stimulate digestion, among them clary sage (Salvia sclarea L.) lemon (Citrus limon L.), coriander (Coriandrum sativum L.), ginger (Zingiber officinalis L.), and, most notably, rosemary (Rosmarinus officinalis L.). This has been attributed at least in part to interaction of EO components with receptors for specific types of “taste” in the gastrointestinal tract, such as bitter taste TAS2R receptors and pungent taste transient receptor potential vanilloid receptors TRPV1 or others, such as ankyrin subtype 1 TRPA1 or TRPM8 [130][33]. Such interaction would activate digestive functions such as bile secretion, gastric motility and secretions, secretion of gastric protective mucus, pancreatic digestive enzymes, etc., thereby promoting all digestive functions by activating the neuroendocrine machinery [130][33]. Besides stimulating digestion, EOs have been recently fount to protect digestive functions and organs from inflammatory and oxidative-stress-related damage. In particular, the liver is subject to major metabolic attack by radicals produced as a consequence of phase-1 detoxifying enzymes activation by pollutants, toxins, and xenobiotics.9. Essential Oils for Diuresis and Protection of the Urinary Tract
Fennel (Foeniculum vulgare Mill.) has a longstanding tradition as a diuretic, anti-inflammatory, and antimicrobial aid to protect the urinary tract. The diuretic effect of the EO and particularly the anti-inflammatory effect has been documented in animal studies, while several microbiological studies highlighted its activity against S. aureus and C. albicans [135][34]. The combination of these bioactivities makes it particularly suited for the health of the urinary tract. Juniper (Juniperus spp.) is often used as adjuvant in the protection of urinary tract because of its anti-inflammatory activity associated with selective antimicrobial activity on the pathogen strains that colonize the tract. The recent investigation of the EOs from three Juniperus species (J. communis, J. horizontalis, and J. chinensis) indicated that J. horizontalis oil has the highest activity against E. coli, while J. communis has the highest activity against S. aureus. The three oils were found to significantly decrease the production of the pro-inflammatory cytokines tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and gamma interferon (INF-γ) in lipopolysaccharide-activated white blood cells. J. chinensis oil possessed the highest potency against IL-1β. Analysis afforded the identification of 45 components, and it was assessed that that 1-terpineol, 4-terpineol, bornyl acetate, limonene, and α-pinene are the positive contributors to both bioactivities (antimicrobial and anti-inflammatory), while β-thujone, 3-carene, and γ-muurolene contributed to IL-1β inhibitory activity [136][35].10. Essential Oils to Reduce Inflammation and Pain
Inflammation is part of our immune response, and it is actually necessary to trigger it. It is a complex regulated process, and in principle, it should terminate when the cause, e.g., the invasion by a pathogen, has been eliminated. However, loss of regulation occurs not infrequently, leading perhaps to more danger than that which triggered it. It can lead to the development of chronic disease such as asthma, atherosclerosis, inflammatory bowel disease, cardiovascular diseases, neurological disorders, and cancer [138,139][36][37]. Inflammation is usually classified into two categories according to its time course and intensity: acute inflammation and chronic inflammation. The two types are characterized by different involvement of immune cells: Acute inflammation of a tissue is often associated with infiltration by innate lymphoid cells such as macrophages and neutrophils, while chronic inflammation is instead often associated with tissue infiltration by more specialized T cells and plasma cells [139][37]. Although both steroidal drugs (e.g., cortisol and mimics) and non-steroidal anti-inflammatory drugs (NSAID) are abundantly available, they are not free from side effects, and their long-term administration, e.g., in chronic inflammation, may not be the best solution. Many plant essential oils have shown excellent efficacy in this regard, with a generally safer profile, which makes them ideal candidates for alternative therapeutic approaches such as dietary interventions enriched by EO-based nutraceuticals [139][37]. EO components such as thymol, thymoquinone, 1,8-cineol, fenchone, α-pinene, β-pinene, citronellol, linalool, myrcene, carvacrol, limonene, menthol, p-cymene, α-phellandrene, α-terpineol, terpinen-4-ol, caryophyllene, bisabolol, chamazulene, δ-3-carene, cinnamaldehyde, eugenol, methyleugenol, and anethole were shown effective in reducing paw edema in rats or were active in other in vivo inflammation models at doses equal to or lower than 25 mg/kg b.w. Particularly noteworthy are 1,8-cineol, fenchone, β-pinene, and thymoquinone, which were active at doses equal or lower than 1 mg/Kg b.w., i.e., showing efficacy of the same magnitude as NSAID drugs such as diclofenac [140,141,144][38][39][40]. The mechanism of anti-inflammatory action is often related to a decrease of the level of pro-inflammatory cytokines such as TNF-α, IL-1β, IL-4, IL-5, IL-6, and IL-8; to the decreased expression of lipoxygenase (LOX) and cyclooxygenase (COX); or to inhibition of their activity, with reduction of pro-inflammatory leukotrienes and prostaglandins formed by these two enzyme systems from arachidonic acid to inhibition of myeloperoxidase (MPO) and with reduction of oxidative stress to the induction of antioxidant enzymes (e.g., CAT, SOD, GPx, GR) that counteract inflammation-related oxidative stress and tissue damage, thereby blocking the vicious circle of radical production–tissue damage–inflammation [139,140,141,142,144][37][38][39][40][41].11. Essential Oils with Immunomodulatory and Anti-Influenza Activity
A recent literature survey concerning the immunostimulant activity of EOs pointed out some differences among studies depending on their type, distinguishing in vitro, pre-clinical, clinical, or those based on diet supplementation of animals. It suggested that further studies are needed to clarity the matter although a few EOs were found to stand out in all families of studies: eucalypt and ginger [148][42]. However, other EOs have accumulated evidence for their efficacy in many studies, including human; these are thyme, lavender, clove, tea tree, and citruses (lemon, orange, and bergamot) [138][36]. The mechanism of immune stimulation is often complex to rationalize, as the same EO typically also expresses anti-inflammatory activity through the down-regulation of pro-inflammatory cytokines, and these, in principle, should stimulate immune response. Although the modulation varies with the actual EO and, even within the same botanical species, with the actual composition of the EO used in the study (i.e., with the chemotype), often, immune stimulation is linked to boosting innate immune response, and it is associated with interfering with the NFkB, p38, or ERK/MAPK signaling pathways [138][36]. Eucalyptus EO, with prevalent 1,8-cyneole content, was found to increase phagocytosis by inducing monocyte-derived macrophages with increased phagocytic activity. The activity of tea tree oil rich in tepinen-4-ol was attributed to activation of NF-kB factor, which increases phagocytic activity. Both tea tree oil and terpinen-4-ol induce the differentiation of immature myelocytes into active phagocytizing monocytes and increase the expression of CD11b, a receptor that is partially responsible for the phagocytosis of opsonized bacteria and fungi by leukocytes [138][36].
12. Essential Oils for Neuroprotection and Modulation of Mood and Cognitive Function
With the global increase of life expectancy, the prevalence of age-related diseases is also increasing, particularly including neurodegenerative conditions such as Alzheimer’s disease (AD). Neurodegenerative diseases and other chronic inflammatory conditions characterized by cognitive impairment are related to lifestyle and to the diet; hence, a dietary intervention can help their course and patients’ quality of life. In AD, the two main microscopic hallmarks of disease, the abnormal accumulation of extracellular protein material in the amyloid–beta plaques and the formation of intracellular neurofibrillary tangles, are associated with abnormal expression of acetylcholinesterase (AChE), which leads to decreased levels of neurotransmitter acetylcholine (ACh), synaptic alteration, and impaired memory and learning [152][43]. Increased AChE expression appears to be related both to the formation of plaques and to the impaired cognitive function; hence, inhibiting AChE is currently the main pharmacological strategy to treat AD [152,153][43][44]. On the other hand, research efforts are clarifying the association between AD, inflammation, and oxidative stress, outlining that antioxidants are key to effective AD treatment strategies [153,154,155][44][45][46]. One additional point is the association between AD and impaired glycemic control, with increased incidence of T2DM in patients with dementia [152][43]. The above constitutes a solid rational basis to understand the potential of dietary EO supplementation in protecting from neurodegenerative conditions such as AD because (1) many EOs have excellent anti-inflammatory activity with low incidence of side effects; (2) many EOs have good antioxidant activity; (3) many EOs are effective in improving glycemic control and T2DM parameters; and (4) EOs are small, lipophilic molecules with high diffusivity, and hence, they have excellent ability to cross the blood–brain barrier and reach the central nervous system. A fifth reason is that some EOs [156,157][47][48] and EO components [156,157,158][47][48][49] have been demonstrated to possess good inhibition activity toward AChE, thereby representing a promising aid to tread AD and other cognitive-impairment conditions [158][49]. Therefore, several essential oils have the potential to ameliorate the cognitive function and protect from AD; these include thyme, sage, eucalypt, lemon balm, peppermint, oregano, rosemary, lavender, basil, and citrus EOs (rich in limonene and citral) owing to the combination of glucose-lowering, anti-inflammatory, antioxidant, and anti-AChE activities [152,156,157,158][43][47][48][49].
Modern aromatherapy is using essential oils to treat anxiety, stress, panic and phobia, and other forms of emotional discomfort. Building on evidence in animal studies, a significant body of research is now being dedicated to unambiguously prove with controlled, randomized clinical trials the efficacy of EOs to treat such mood disorders [183][50]. For instance, Melissa officinalis L. (lemon balm) EO was tested in acute coronary syndrome (ACS) patients, resulting in significantly reduced scores of stress and anxiety, with reduced heart rate (p < 0.001) along with remarkable decrease in the mean arterial pressure in the Melissa group compared to the placebo group (p < 0.001) [176][51]. Lavandula angustifolia L. (lavender) EO was tested for 4 weeks on patients with insomnia, showing significantly improved sleep quality and duration, improved quality of life, and improved overall mood [178][52], while the combination of lavender with chamomile (Matricaria recutita) showed statistically significant improvement in depression, anxiety, and stress levels immediately and one month after the intervention in the lavender and chamomile group compared to the control group (p < 0.01) [171][53]. Similarly, lavender combined with Roman chamomile (Anthemis nobilis) and neroli (Citrus aurantium flowers EO) showed reduced anxiety and improved sleep quality [181][54].References
- Marongiu, B.; Porceddu, S.; Piras, A.; Falconieri, D. Traditional and modern methods for the preparation of essential oils. In Essential Oils and Natural Food Additives: Composition, Applications, Antioxidant and Antimicrobial Properties; Valgimigli, L., Ed.; Nova Science Publishing: New York, NY, USA, 2012; pp. 25–46. ISBN 978-1-62100-241-3.
- Zhang, J.; Zhang, M.; Ju, R.; Chen, K.; Bhandari, B.; Wang, H. Advances in efficient extraction of essential oils from spices and its application in food industry: A critical review. Crit. Rev. Food Sci. Nutr. 2022, 2092834.
- Mancianti, F.; Ebani, V.V. Biological Activity of Essential Oils. Molecules 2020, 25, 678.
- Dhifi, W.; Bellili, S.; Jazi, S.; Bahloul, N.; Mnif, W. Essential Oils’ Chemical Characterization and Investigation of Some Biological Activities: A Critical Review. Medicines 2016, 3, 25.
- Valgimigli, L. Essential oils: An overview on origins, chemistry, properties and uses. In Essential Oils and Natural Food Additives: Composition, Applications, Antioxidant and Antimicrobial Properties; Valgimigli, L., Ed.; Nova Science Publishing: New York, NY, USA, 2012; pp. 1–24. ISBN 978-1-62100-241-3.
- Valnet, J. The Practice of Aromatherapy. A Classic Compendium of Plant Medicines and Their Healing Properties; Tisserand, R.B., Ed.; Healing Arts Press: Rochester, NY, USA, 1982; ISBN 0-89281-398-9.
- Price, S.; Price, L. Aromatherapy for Health Professionals, 4th ed.; Elsevier: London, UK, 2012; ISBN 978-0-7020-3564-7.
- Farrar, A.J.; Farrar, F.C. Clinical Aromatherapy. Nurs. Clin. N. Am. 2020, 55, 489–504.
- Ali, B.; Al-Wabel, N.A.; Shams, S.; Ahamad, A.; Khan, S.A.; Anwar, F. Essential oils used in aromatherapy: A systemic review. Asian Pac. J. Trop. Biomed. 2015, 5, 601–611.
- Rahimi, R. Herbal medicines for the management of irritable bowel syndrome: A comprehensive review. World J. Gastroenterol. 2012, 18, 589–600.
- Balakrishnan, A. Therapeutic Uses of Peppermint—A Review. J. Pharm. Sci. Res. 2015, 7, 474.
- Hawthorn, M.; Ferrante, J.; Luchowski, E.; Rutledge, A.; Wei, X.Y.; Triggle, D.J. The actions of peppermint oil and menthol on calcium channel dependent processes in intestinal, neuronal and cardiac preparations. Aliment. Pharmacol. Ther. 1988, 2, 101–118.
- Amorati, R.; Foti, M.C.; Valgimigli, L. Antioxidant Activity of Essential Oils. J. Agric. Food Chem. 2013, 61, 10835–10847.
- Gabbai-Armelin, P.R.; Sales, L.S.; Ferrisse, T.M.; De Oliveira, A.B.; De Oliveira, J.R.; Giro, E.M.A.; Brighenti, F.L. A systematic review and meta-analysis of the effect of thymol as an anti-inflammatory and wound healing agent. Phytother. Res. 2022, 36, 3415–3443.
- Subramaniyam, S.; Yang, S.; Diallo, B.N.; Fanshu, X.; Lei, L.; Li, C.; Bishop, O.T.; Bhattacharyya, S. Oral Phyto-thymol ameliorates the stress induced IBS symptoms. Sci. Rep. 2020, 10, 13900.
- Toschi, A.; Tugnoli, B.; Rossi, B.; Piva, A.; Grilli, E. Thymol modulates the endocannabinoid system and gut chemosensing of weaning pigs. BMC Vet. Res. 2020, 16, 289.
- Zhao, M.; Gönczi, L.; Lakatos, P.L.; Burisch, J. The Burden of Inflammatory Bowel Disease in Europe in 2020. J. Crohn’s Colitis 2021, 15, 1573–1587.
- Spisni, E.; Petrocelli, G.; Imbesi, V.; Spigarelli, R.; Azzinnari, D.; Sarti, M.D.; Campieri, M.; Valerii, M.C. Antioxidant, Anti-Inflammatory, and Microbial-Modulating Activities of Essential Oils: Implications in Colonic Pathophysiology. Int. J. Mol. Sci. 2020, 21, 4152.
- Nutrition Division, FAO/WHO. Probiotics in food. Health and nutritional properties and guidelines for evaluation. FAO Food Nutr. Pap. (FAO) 2006, 85, 1–56. Available online: https://www.fao.org/publications/card/en/c/7c102d95-2fd5-5b22-8faf-f0b2e68dfbb6/ (accessed on 1 December 2022).
- Zmora, N.; Zilberman-Schapira, G.; Suez, J.; Mor, U.; Dori-Bachash, M.; Bashiardes, S.; Kotler, E.; Zur, M.; Regev-Lehavi, D.; Brik, R.B.-Z.; et al. Personalized Gut Mucosal Colonization Resistance to Empiric Probiotics Is Associated with Unique Host and Microbiome Features. Cell 2018, 174, 1388–1405.e21.
- Probiotics. Fact Sheet for Health Professionals. Available online: https://ods.od.nih.gov/factsheets/Probiotics-HealthProfessional/ (accessed on 1 December 2022).
- Gibson, G.R.; Hutkins, R.; Sanders, M.E.; Prescott, S.L.; Reimer, R.A.; Salminen, S.J.; Scott, K.; Stanton, C.; Swanson, K.S.; Cani, P.D.; et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 491–502.
- Deep, S.; Karmakar, S.; Khare, R.S.; Ojha, S.; Kundu, K.; Kundu, S. Development of Probiotic Candidate in Combination with Essential Oils from Medicinal Plant and Their Effect on Enteric Pathogens: A Review. Gastroenterol. Res. Pract. 2012, 2012, 457150.
- Unusan, N. Essential oils and microbiota: Implications for diet and weight control. Trends Food Sci. Technol. 2020, 104, 60–71.
- Jaiswal, S.; Kundu, K.; Karmakar, S.; Kundu, S. Bacterial strains from local curd, ice-cream and natural milk cultures as po-tential probiotic candidate: Isolation, characterization and in vitro analysis. Int. J. Probiotics Prebiotics 2009, 4, 187–194.
- Oliveira, F.D.A.; Andrade, L.N.; De Sousa, B.V.; de Sousa, D. Anti-Ulcer Activity of Essential Oil Constituents. Molecules 2014, 19, 5717–5747.
- Alomair, M.K.; Alabduladheem, L.S.; Almajed, M.A.; Alobaid, A.A.; Alkhalifah, E.A.R.; Younis, N.S.; Mohamed, M.E. Achillea millefolium Essential Oil Mitigates Peptic Ulcer in Rats through Nrf2/HO-1 Pathway. Molecules 2022, 27, 7908.
- Guesmi, F.; Ali, M.B.; Barkaoui, T.; Tahri, W.; Mejri, M.; Ben-Attia, M.; Bellamine, H.; Landoulsi, A. Effects of Thymus hirtus sp. algeriensis Boiss. Et Reut. (Lamiaceae) essential oil on healing gastric ulcers according to sex. Lipids Health Dis. 2014, 13, 138. Available online: http://www.lipidworld.com/content/13/1/138 (accessed on 3 January 2023).
- De Cássia da Silveira e Sá, R.; Andrade, L.N.; de Sousa, D.P. A Review on Anti-Inflammatory Activity of Monoterpenes. Molecules 2013, 18, 1227–1254.
- Khosropour, P.; Sajjadi, S.-E.; Talebi, A.; Minaiyan, M. Anti-inflammatory effect of Myrtus communis hydroalcoholic extract and essential oil on acetic acid-induced colitis in rats. J. Rep. Pharm. Sci. 2019, 8, 204.
- De Blasio, A.; D’Anneo, A.; Lauricella, M.; Emanuele, S.; Giuliano, M.; Pratelli, G.; Calvaruso, G.; Carlisi, D. The Beneficial Effects of Essential Oils in Anti-Obesity Treatment. Int. J. Mol. Sci. 2021, 22, 11832.
- Pramanik, K.C.; Biswas, R.; Bandyopadhyay, D.; Mishra, M.; Ghosh, C.; Chatterjee, T.K. Evaluation of anti-ulcer properties of the leaf extract of Juniperus communis L. in animals. J. Nat. Remedies 2007, 7, 207–213.
- Valussi, M. Functional foods with digestion-enhancing properties. Int. J. Food Sci. Nutr. 2012, 63, 82–89.
- Saddiqi, H.A.; Iqbal, Z. Usage and Significance of Fennel (Foeniculum vulgare Mill.) Seeds in Eastern Medicine. In Nuts and Seeds in Health and Disease Prevention; Preedy, V.R., Watson, R.R., Patel, V.B., Eds.; Elsevier: London, UK, 2011; pp. 461–467.
- Darwish, R.S.; Hammoda, H.M.; Ghareeb, D.A.; Abdelhamid, A.S.; El Naggar, E.M.B.; Harraz, F.M.; Shawky, E. Efficacy-directed discrimination of the essential oils of three Juniperus species based on their in-vitro antimicrobial and anti-inflammatory activities. J. Ethnopharmacol. 2020, 259, 112971.
- Sandner, G.; Heckmann, M.; Weghuber, J. Immunomodulatory Activities of Selected Essential Oils. Biomolecules 2020, 10, 1139.
- Zuo, X.; Gu, Y.; Wang, C.; Zhang, J.; Zhang, J.; Wang, G.; Wang, F. A Systematic Review of the Anti-Inflammatory and Immunomodulatory Properties of 16 Essential Oils of Herbs. Evid. Based Complement. Altern. Med. 2020, 2020, 2020–8878927.
- Guimarães, A.G.; Quintans, J.S.S.; Quintans-Júnior, L.J. Monoterpenes with Analgesic Activity—A Systematic Review. Phytother. Res. 2013, 27, 1–15.
- de Cássia Da Silveira e Sá, R.; Andrade, L.N.; De Sousa, D.P. Sesquiterpenes from Essential Oils and Anti-Inflammatory Activity. Nat. Prod. Commun. 2015, 10, 1767–1774.
- Sá, R.D.C.D.S.E.; Andrade, L.N.; Oliveira, R.D.R.B.D.; De Sousa, D.P. A Review on Anti-Inflammatory Activity of Phenylpropanoids Found in Essential Oils. Molecules 2014, 19, 1459–1480.
- Matos, M.S.; Anastácio, J.D.; Nunes dos Santos, C. Sesquiterpene Lactones: Promising Natural Compounds to Fight Inflammation. Pharmaceutics 2021, 13, 991.
- Peterfalvi, A.; Miko, E.; Nagy, T.; Reger, B.; Simon, D.; Miseta, A.; Czéh, B.; Szereday, L. Much More Than a Pleasant Scent: A Review on Essential Oils Supporting the Immune System. Molecules 2019, 24, 4530.
- Agatonovic-Kustrin, S.; Kustrin, E.; Morton, D.W. Essential oils and functional herbs for healthy aging. Neural Regen. Res. 2019, 14, 441–445.
- De Simone, A.; Bartolini, M.; Baschieri, A.; Apperley, K.Y.; Chen, H.H.; Guardigni, M.; Montanari, S.; Kobrlova, T.; Soukup, O.; Valgimigli, L.; et al. Hydroxy-substituted trans-cinnamoyl derivatives as multifunctional tools in the context of Alzheimer’s disease. Eur. J. Med. Chem. 2017, 139, 378–389.
- Sinyor, B.; Mineo, J.; Ochner, C. Alzheimer’s Disease, Inflammation, and the Role of Antioxidants. J. Alzheimer’s Dis. Rep. 2020, 4, 175–183.
- Tarozzi, A.; Bartolini, M.; Piazzi, L.; Valgimigli, L.; Amorati, R.; Bolondi, C.; Djemil, A.; Mancini, F.; Andrisano, V.; Rampa, A. From the dual function lead AP2238 to AP2469, a multi-target-directed ligand for the treatment of Alzheimer’s disease. Pharmacol. Res. Perspect. 2014, 2, e00023.
- Farag, M.A.; Ezzat, S.M.; Salama, M.M.; Tadros, M.G.; Serya, R.A. Anti-acetylcholinesterase activity of essential oils and their major constituents from four Ocimum species. Z. Für Nat. C 2016, 71, 393–402.
- Aazza, S.; Lyoussi, B.; Miguel, M.G. Antioxidant and Antiacetylcholinesterase Activities of Some Commercial Essential Oils and Their Major Compounds. Molecules 2011, 16, 7672–7690.
- Min, S.L.S.; Liew, S.Y.; Chear, N.J.Y.; Goh, B.H.; Tan, W.-N.; Khaw, K.Y. Plant Terpenoids as the Promising Source of Cholinesterase Inhibitors for Anti-AD Therapy. Biology 2022, 11, 307.
- Zhang, N.; Yao, L. Anxiolytic Effect of Essential Oils and Their Constituents: A Review. J. Agric. Food Chem. 2019, 67, 13790–13808.
- Veiskaramian, A.; Gholami, M.; Yarahmadi, S.; Baharvand, P.A.; Birjandi, M. Effect of aromatherapy with Melissa essential oil on stress and hemodynamic parameters in acute coronary syndrome patients: A clinical trial in the emergency department. Complement. Ther. Clin. Pract. 2021, 44, 101436.
- Lari, Z.N.; Hajimonfarednejad, M.; Riasatian, M.; Abolhassanzadeh, Z.; Iraji, A.; Vojoud, M.; Heydari, M.; Shams, M. Efficacy of inhaled Lavandula angustifolia Mill. Essential oil on sleep quality, quality of life and metabolic control in patients with diabetes mellitus type II and insomnia. J. Ethnopharmacol. 2020, 251, 112560.
- Zamanifar, S.; Bagheri-Saveh, M.I.; Nezakati, A.; Mohammadi, R.; Seidi, J. The Effect of Music Therapy and Aromatherapy with Chamomile-Lavender Essential Oil on the Anxiety of Clinical Nurses: A Randomized and Double-Blind Clinical Trial. J. Med. Life 2020, 13, 87–93.
- Cho, M.-Y.; Min, E.S.; Hur, M.-H.; Lee, M.S. Effects of Aromatherapy on the Anxiety, Vital Signs, and Sleep Quality of Percutaneous Coronary Intervention Patients in Intensive Care Units. Evid. Based Complement. Altern. Med. 2013, 2013, 381381.
