Triple-negative breast cancer (TNBC) accounts for 15–20% of all breast cancers and is characterized by an aggressive nature and a high rate of recurrence despite neoadjuvant and adjuvant chemotherapy. Although novel agents are constantly being introduced for the treatment of breast cancer, conventional cytotoxic chemotherapy based on anthracyclines and taxanes is the mainstay treatment option for TNBC. Based on CTNeoBC pooled analysis data, the achievement of pathologic CR (pCR) in TNBC is directly linked to improved survival outcomes. Therefore, the treatment paradigm for early TNBC has shifted to neoadjuvant treatment, and the escalation of neoadjuvant chemotherapy to improve the pCR rate and the addition of post-neoadjuvant chemotherapy to control the residual disease have been investigated.
- triple-negative breast cancer
- neoadjuvant chemotherapy
- immune checkpoint inhibitor
1. Classical Adjuvant Treatment for Triple-Negative Breast Cancer (TNBC)
1. Classical Adjuvant Treatment for TNBC
2. The Role of Platinum in Adjuvant Treatment for TNBC
Platinum agents inhibit DNA synthesis by forming cross-links with DNA, leading to cancer cell apoptosis in malignancies that harbor defective DNA repair mechanisms [10][26]. Patients harboring BRCA1/2 mutations show homologous recombination deficiency (HRD) and are susceptible to DNA repair damage when platinum agents are used [11][27]. Some patients with sporadic TNBC who do not harbor BRCA1/2 mutations show similar defects in the DNA repair mechanism, similar to BRCA1/2 mutant TNBC, called BRCAness [12][28]. Although not all patients with TNBC harbor HRD, there is a certain chance of BRCAness in sporadic TNBC. Based on the probability of BRCAness, platinum agents are preferred for the treatment of TNBC.3. Neoadjuvant Treatment for TNBC
In stage II or III TNBC, neoadjuvant chemotherapy is preferred based on various treatment guidelines [1][13][6,17]. The survival outcomes of patients receiving neoadjuvant or adjuvant chemotherapy after surgical resection are not statistically different, and neoadjuvant treatment is traditionally associated with an increased rate of local control, thereby guiding breast-conserving surgery with organ preservation [14][15][11,33]. As the development of neoadjuvant treatment is rapidly progressing, pathologic complete response (pCR), defined as the absence of malignant tumor cells in the breast and axillary lymph nodes, is frequently observed after surgical resection. Based on CTNeoBC pooled analysis, achievement of pCR is associated with improved survival outcomes, and neoadjuvant chemotherapy has evolved with the incorporation of novel regimens [16][12]. Similar to standard adjuvant treatment, traditional neoadjuvant chemotherapy is also based on anthracyclines and taxanes, and a dose-dense regimen is preferred in neoadjuvant settings based on improved DFS and OS proven in a meta-analysis [4][20].4. Addition of Platinum during Neoadjuvant Chemotherapy
To increase the pCR rate during neoadjuvant chemotherapy, the escalation of neoadjuvant treatment based on a combination regimen with platinum has been the focus in recent years. The combination of platinum and conventional taxane and anthracycline regimens has improved the pCR rate from approximately 35% to over 50% in TNBC [17][18][19][35,36,37]. The meta-analysis also revealed a similar survival benefit of combining platinum with taxane and anthracycline in patients with TNBC. The combination of platinum for neoadjuvant chemotherapy was based on the rationale that sporadic TNBC may show BRCAness and a good response to platinum [11][12][27,28]. Contrary to expectations, the combination of platinum showed the greatest benefit in sporadic TNBC patients who were gBRCA wild type, and the gBRCA mutant patient subgroup showed only a marginal benefit [19][20][21][37,38,39]. Previous clinical trials have focused on increasing the pCR rate, but the prolongation of survival is not fully validated, and a longer follow-up is warranted at present.5. Role of an Immune Checkpoint Inhibitor in Neoadjuvant Setting
As pembrolizumab and atezolizumab have shown PFS benefits in phase III trials [22][23][40,41], the role of immune checkpoint inhibitors (ICI) has expanded into neoadjuvant settings. Although atezolizumab showed conflicting or disappointing results in advanced or early TNBC [24][25][42,43], pembrolizumab showed consistent PFS and OS benefits in advanced TNBC [22][26][40,44]. Furthermore, a combination of pembrolizumab with paclitaxel–carboplatin followed by anthracycline showed an increase in the pCR rate and also improved event-free survival rate [27][28][29][45,46,47]. The pivotal KEYNOTE-522 trial has changed the treatment paradigm for stage II and III TNBC by introducing pembrolizumab as a standard treatment during neoadjuvant treatment. The KEYNOTE-522 trial evaluated the role of pembrolizumab (18 cycles, 200 mg every 3 weeks) combined with four cycles of carboplatin (3 weekly) and paclitaxel (weekly or 3 weekly), followed by anthracycline plus cyclophosphamide (3 weekly), which powered the co-primary endpoint of increased pCR and EFS compared to placebo with chemotherapy. The addition of pembrolizumab showed a 13.6% improvement in pCR (64.8% (95% confidence interval; CI = 59.9–69.5%) vs. 51.2% (95% CI = 44.1–58.3%)) and a 7.7% improvement in the 36-month EFS rate (84.5% (95% CI = 81.7–86.9%) vs. 76.8% (95% CI = 72.2–80.7%)), meeting the primary endpoint of the study [28][29][46,47]. The combination of pembrolizumab showed a benefit irrespective of PD-L1 status evaluated by the 22C3 pharmDx assay or lymph node involvement status. Although the follow-up duration was immature, there were trends toward superior OS in the pembrolizumab-treated population, and further follow-up of the data is warranted [28][46]. Positive data from KEYNOTE-522 have changed the standard treatment guidelines for neoadjuvant treatment in stage II-III TNBC [1][17]. However, there are some open questions when applying pembrolizumab for neoadjuvant treatment in the clinic. First, further studies are warranted to select patients who may benefit the most from the addition of pembrolizumab. Fatal immune-related adverse events may occur during neoadjuvant pembrolizumab treatment plus chemotherapy. Therefore, it is necessary to choose patients who may benefit most from pembrolizumab, but there is no established biomarker for selecting appropriate patients. Unlike advanced or metastatic TNBC [22][40], PD-L1 expression was not associated with an improved pCR rate or EFS in the KEYNOTE-522 trial. Other immune-related markers, such as tumor-infiltrating lymphocytes (TIL), are currently being investigated [30][31][48,49], and follow-up of these results is needed. Second, the backbone chemotherapy regimen of the KEYNOTE-522 trial consisted of three weekly paclitaxel–carboplatin cycles followed by anthracycline and cyclophosphamide. Considering that dose-dense neoadjuvant regimens show superior OS benefits in TNBC [32][50], the incorporation of a dose-dense regimen with pembrolizumab needs to be evaluated based on a prospective randomized trial.6. Post-Neoadjuvant Treatment for TNBC
6.1. Post-Neoadjuvant Treatment in Patients with Residual Disease
As neoadjuvant treatment has become a standard treatment, clinicians have focused on patients who do not achieve pCR. Non-pCR patients show poor survival outcomes compared to pCR patients [16][12], and post-neoadjuvant treatment has been applied to non-pCR patients to achieve prolonged survival outcomes. The escalation of treatment in non-pCR patients has effectively prolonged survival outcomes, and there has been great success in this patient subgroup.
The phase III CREATE-X trial enrolled patients who showed residual disease after neoadjuvant anthracycline and taxane treatments [33][51]. Among the total patient population, 32.2% of patients were classified as TNBC, and approximately 40% of patients were clinically diagnosed with stage IIIA or IIIB TNBC. Patients who received 6–8 cycles of adjuvant capecitabine showed superior DFS, fulfilling the primary endpoint (HR = 0.70, 95% CI = 0.53–0.92, p = 0.01). At the time of data analysis, the median OS was not reached, and capecitabine-treated patients showed better OS compared to the control arm (HR = 0.59, 95% CI = 0.39–0.90, p = 0.01). In the prespecified subgroup analysis, TNBC patients still showed superior DFS and OS (HR for recurrence = 0.58, 95% CI = 0.39–0.87; HR for death = 0.52, 95% CI = 0.30–0.90). Although capecitabine-treated patients showed a higher rate of adverse events (AEs), such as hand-foot syndrome, AEs were generally well manageable with the maintenance of relative dose intensity in more than 80% of enrolled patients. Trials conducted prior to CREATE-X failed to prove the positive survival benefit of capecitabine [34][35][52,53], but these conflicting data may result from the small number of TNBC patients enrolled in the study [33][51]. In the Finland Capecitabine Trial (FinXX), although the prolongation of DFS was not validated, there were significant improvements in OS in the capecitabine and docetaxel combination group [35][53]. Although the administration schedule of capecitabine was different, the SYSUCC-001 trial showed prolongation of DFS in patients who received 1 year of metronomic capecitabine after completion of adjuvant treatment [36][54], and the CBCSG010 trial showed that the combination of capecitabine with standard adjuvant treatment improved DFS and OS, meeting the primary endpoint [37][55]. At present, the CREATE-X trial is the first phase III trial validating the positive role of capecitabine in post-neoadjuvant treatment and is accepted as the standard treatment for TNBC patients who show residual disease after neoadjuvant chemotherapy [1][13][6,17]. Recently, a phase III ECOG-ACRIN EA1131 trial was conducted comparing four cycles of post-neoadjuvant platinum to the standard six cycles of post-neoadjuvant capecitabine in basal subtype TNBC patients presenting with residual disease after neoadjuvant chemotherapy [38][56]. After a median follow-up of 20 months, platinum showed inferior 3-year invasive DFS (iDFS) compared to capecitabine-treated patients (3-year iDFS, 42% vs. 49%, HR = 1.06, 95% CI = 0.62–1.81), and the trial was terminated early. This trial further strengthens the role of post-neoadjuvant capecitabine therapy in patients with non-pCR TNBC.6.2. Post-Neoadjuvant Treatment in Pembrolizumab-Treated Patients with pCR
Patients who achieved pCR after neoadjuvant chemotherapy showed a good prognosis in a meta-analysis [16][12], and this was also verified in the KEYNOTE-522 trial. Patients who achieved pCR showed favorable outcomes, irrespective of pembrolizumab administration. The 3-year EFS rate was 94.4% in the pembrolizumab arm and 92.5% in the control arm (HR = 0.73, 95% CI = 0.39–1.36), with no statistical difference [29][47]. Considering that ICI administration infrequently results in the development of autoimmune-related AEs and also causes financial toxicities in certain circumstances, de-escalation of ICI can be considered in this subgroup of patients. In the phase II GeparNuevo trial, durvalumab was administered as part of neoadjuvant chemotherapy with nab-paclitaxel and dose-dense epirubicin or cyclophosphamide. Although durvalumab was not administered after surgery, patients who achieved pCR showed excellent survival outcomes (3-year iDFS rate, 95.5%) [39][59].6.3. Adjuvant Treatment in a Special Population: The gBRCA Mutant Patient Subgroup
gBRCA mutations have been detected in 10–15% of unselected TNBC patients [40][62]. Germline BRCA1 and BRCA2 mutant carriers have a 65% and 45% risk of developing breast cancer at the age of 70, respectively [41][63]. In metastatic gBRCA1/2 mutant breast cancer, olaparib and talazoparib have shown benefits for prolonging PFS [42][43][64,65] and are currently approved by the FDA. The phase III OLYMPIA trial verified the role of adjuvant olaparib in HER2-negative gBRCA1/2 mutant high-risk breast cancer [44][66]. Enrolled TNBC patients who underwent upfront surgery were eligible if they were diagnosed with stage II disease or above. If a patient receives neoadjuvant chemotherapy, the residual disease should be confirmed in the surgical pathology specimens. ER-positive gBRCA1/2 mutations who underwent upfront surgery should present with at least four positive lymph node involvements. If neoadjuvant chemotherapy is administered, patients should have a residual disease with clinical and pathological staging (CPS) ER status and a histologic grade (EG) score of 3 or higher [45][67]. Patients were randomly assigned in a 1:1 ratio to receive adjuvant olaparib or placebo for 1 year. The olaparib arm showed excellent improvement in 3-year iDFS compared to the placebo arm (85.9% vs. 77.1%, HR = 0.58, 99.5% CI = 0.41–0.82, p < 0.001). Subsequent follow-up data demonstrated that 1 year of adjuvant olaparib also prolonged the 4-year OS rate to 89.8% compared to 86.4% in the control arm, with an absolute difference of 3.4% (HR = 0.68, 98.5% CI = 0.47–0.97, p = 0.009) [46][68]. During 3.5 years of median follow-up, two acute myeloid leukemia (AML) cases were diagnosed in the olaparib arm and three patients in the control arm, demonstrating no new safety signal of hematologic disorders. This absolute benefit of adjuvant olaparib in gBRCA1/2 mutant early breast cancer (EBC) has been reflected in treatment guidelines, and adjuvant olaparib is currently the standard treatment in gBRCA1/2 mutant EBC patients [1][17]. Considering this definite survival benefit of olaparib, gBRCA1/2 testing should be actively considered in TNBC patients regardless of a patient’s age. The CREATE-X, KEYNOTE-522, and OLYMPIA trials have all changed the treatment paradigm in early TNBC, and prior trials should be fully considered when choosing adjuvant treatment in gBRCA1/2 mutant patients. Careful decision-making is warranted, considering that the CREATE-X and KEYNOTE-522 trials did not consider gBRCA1/2 mutation status during the study. In gBRCA1/2 mutant patients who were pretreated with neoadjuvant chemotherapy without pembrolizumab, olaparib and capecitabine can both be options for adjuvant treatment for patients presenting with residual disease, considering that the survival benefit was proven in previous pivotal trials. Among these two agents, olaparib can be carefully considered over capecitabine for several reasons. First, an adjuvant PARP inhibitor for gBRCA1/2 mutant TNBC directly targets the DNA damage repair pathway and may show high sensitivity and act as a targeting agent in this population of patients [47][69]. Second, the adjuvant capecitabine trials did not consider BRCA mutations during the analysis. In addition to CREATE-X, the SYSUCC-001 and CBCSG010 trials did not consider gBRCA1/2 status during analysis, and the lack of sufficient data to consider capecitabine can have a role in gBRCA1/2 mutant patients [33][36][37][51,54,55]. Post hoc analysis of the FinXX trial demonstrated that combining capecitabine may be more beneficial in non-BRCA-like tumors than in BRCA-like tumors [48][70], and these data may also support the use of olaparib in gBRCA1/2 mutant TNBC patients showing residual disease after neoadjuvant chemotherapy.7. Conclusions
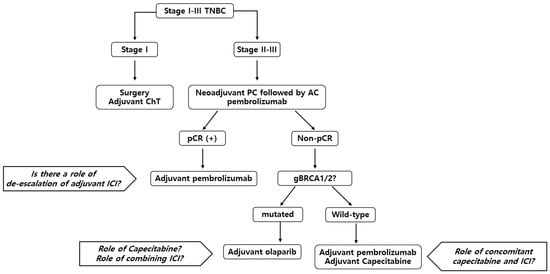
The standard treatment for early TNBC is neoadjuvant chemotherapy, followed by surgery. Based on the survival benefit of the KEYNOTE-522 trial, a combination of pembrolizumab with anthracycline, taxane, and carboplatin is currently the treatment of choice. After completion of neoadjuvant treatment, adjuvant treatment options can vary based on the presence of residual disease and gBRCA1/2 mutation status. In patients who present with pCR, completion of pembrolizumab treatment for a total of 1 year can be considered. However, several options can be considered for patients with residual disease. Other than the completion of pembrolizumab, capecitabine and olaparib should be considered according to the patient’s status. Currently, there is no evidence of a combination of ICI with capecitabine or olaparib, but there are ongoing clinical trials to determine the best treatment strategy for this patient population. The suggested treatment flow is described in Figure 1.