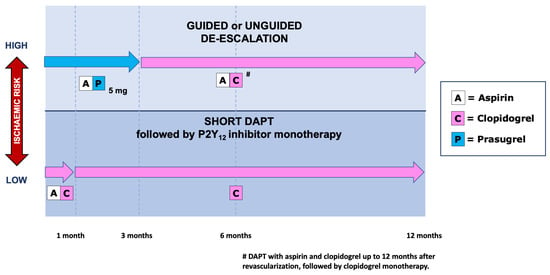
Patients ≥ 75 years of age account for about one third of hospitalizations for acute coronary syndromes (ACS). Since the European Society of Cardiology guidelines recommend that older ACS patients use the same diagnostic and interventional strategies used by the younger ones, most elderly patients are currently treated invasively. Therefore, an appropriate dual antiplatelet therapy (DAPT) is indicated as part of the secondary prevention strategy to be implemented in such patients. The choice of the composition and duration of DAPT should be tailored on an individual basis, after careful assessment of the thrombotic and bleeding risk of each patient. Advanced age is a main risk factor for bleeding. DRecent data show that in patients of high bleeding risk short DAPT (1 to 3 months) is associated with decreased bleeding complications and similar thrombotic events, as compared to standard 12-month DAPT. Clopidogrel seems the preferable P2Y12 inhibitor, due to a better safety profile than ticagrelor. When the bleeding risk is associated with a high thrombotic risk (a circumstance present in about two thirds of older ACS patients) it is important to tailor the treatment by taking into account the fact that the thrombotic risk is high during the first months after the index event and then wanes gradually over time, whereas the bleeding risk remains constant.
- elderly patients
- acute coronary syndrome
- anti-platelet therapy
1. Introduction
2. Invasive versus Conservative Strategy
Although the European Society of Cardiology (ESC) STEMI guidelines state that “there is no upper age limit with respect to reperfusion, especially with primary PCI” [21][23], there is relatively little information regarding the outcomes of elderly patients undergoing primary PCI, due to the low representation of elderly patients in clinical trials assessing the effects of mechanical reperfusion for STEMI. A pooled analysis [22][24] including 834 patients enrolled in three randomized trials (Zwolle [23][25], SENIOR PAMI [24][26], and TRIANA [22][24]) showed that the overall risk of death, re-infarction, or disabling stroke was substantially lower for patients allocated to primary PCI compared with those treated with fibrinolysis (14.9% vs. 21.5%; odds ratio [OR], 0.64; 95% confidence interval [CI] 0.45–0.91; p = 0.013), and s only a trend toward reduction of death was found (10.7% versus 13.8%, hazard ratio [HR] 0.74, 95% CI 0.49–1.13), although the effect size was superimposable to that of the largest metanalysis comparing fibrinolysis and primary PCI in younger patients. Septuagenarians and octogenarians undergoing primary PCI show higher mortality rates, both at short-term and mid-term follow-up than younger patients. In dedicated randomized trials in NSTE-ACS patients, the Italian Elderly ACS trial [13][25][13,31], which enrolled 313 patients with NSTE-ACS aged ≥75 years; the After Eighty trial [26][32], which randomized 557 patients with NSTE-ACS aged ≥80 years; and the RINCAL trial [27][33] that included 251 patients, the results went in the same direction: older patients allocated to the routine invasive strategy had a lower risk of death and MI, as shown by a meta-analysis (OR 0.65, 95% CI 0.51–0.83; p < 0.001) at a median follow-up of 36 months. This result was mostly driven by a statistically significant reduction in MI with a trend towards a lower mortality rate, without heterogeneity among the studies [28][34]. A significant reduction in mortality was, however, found in the observational SENIOR NSTEMI cohort study that included patients aged >80 years: applying a propensity-score model, theis study showed that at 5 years the adjusted risk of dying was 44% lower with early invasive treatment, with the difference emerging from 1 year onwards [29][35]. The ongoing SENIOR-RITA trial is randomizing a large series of NSTEMI patients aged ≥75 years to determine the impact of a routine invasive strategy on cardiovascular death and non-fatal MI, compared with a conservative treatment strategy [30][36].3. Dual Antiplatelet Therapy in Elderly ACS Patients: Comparative Efficacy and Safety among Different P2Y12 Inhibitors
Data on optimal platelet inhibition in older adults is limited [31][41], because elderly patients were underrepresented in the pivotal trials: they accounted for only 13% of patients in the TRITON-TIMI 38 trial (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel—Thrombolysis in Myocardial Infarction study) [32][42] and for 15% in the PLATO (The Study of Platelet Inhibition and Patient Outcomes) trial [33][43]. Dual antiplatelet therapy (DAPT) with prasugrel at 10 mg daily dose associated with aspirin significantly increased bleeding in the TRITON-TIMI 38 trial as compared to DAPT with clopidogrel [32][42], so that its use in elderly patients was not recommended by the Food and Drug Administration, whereas the European Medicines Agency indicated a 5 mg/day maintenance dose [34][44]. On the contrary, an analysis of the PLATO trial showed that the superiority of DAPT with ticagrelor over DAPT with clopidogrel (including a reduction in cardiovascular mortality) was confirmed also in the elderly population [35][45]. These indications were issued despite the fact that the differences in the primary endpoint of death, MI and stroke between clopidogrel and prasugrel in the TRITON-TIMI 38 trial (18.3% vs. 17.2%) [32][42] and those between clopidogrel and ticagrelor in the PLATO trial (18.3% vs. 17.2%) [35][45] were exactly the same. Specific trials have been conducted in older ACS patients, comparing different P2Y12 inhibitors in association with aspirin. The ELDERLY ACS 2 trial randomized 1443 ACS patients aged ≥75 years who underwent PCI and showed similar combined thrombotic and bleeding events in patients assigned to 12-month DAPT with a prasugrel 5 mg maintenance dose and in those assigned to 12-month DAPT with clopidogrel 75mg [36][49]. In a post hoc analysis, DAPT with prasugrel 5 mg, as compared to DAPT with clopidogrel, reduced thrombotic events in the first month after the index event, but increased late bleeding (31–365 days) [37][50]. DAPT with low-dose prasugrel and clopidogrel also had similar efficacy and safety in medically treated elderly patients enrolled in the TRILOGY ACS (Targeted Platelet Inhibition to Clarify the Optimal Strategy to Medically Manage Acute Coronary Syndromes) study [38][51]. At odds with the results of the post hoc analysis of the PLATO trial, the POPular AGE (Ticagrelor or Prasugrel Versus Clopidogrel in Elderly Patients With an Acute Coronary Syndrome and a High Bleeding Risk: Optimization of Antiplatelet Treatment in High-Risk Elderly) trial showed that DAPT with clopidogrel had significantly lower bleeding rates (including fatal bleeding) compared with DAPT with ticagrelor (17.6% vs. 23.1%; OR 0.74; 95% CI 0.56–0.97), without any difference in thrombotic events (12.8% vs. 12.5%; OR 1.02, 95% CI 0.72–1.45) [39][53]. Notably, ticagrelor was prematurely discontinued in about half of the patients randomly allocated to that drug, a finding that could have hampered its potential benefits, but that also indicates that side effects induced by that drug affect a large part of older adults.4. Bleeding and Thrombotic Risk in Elderly ACS Patients
The goal of the antiplatelet therapy after ACS is to reduce the risk of recurrence of ischemic events, likewise attenuating the bleeding risk [40][60]. The choice of the composition and optimal duration of DAPT [41][42][61,62] should be made on an individual basis, and its effects repeatedly verified throughout the follow-up period. Therefore, cardiologists should assess the thrombotic and bleeding risk of each patient by considering clinical, anatomical, procedural and laboratory data. To this purpose, risk scores, especially for the measurement of the bleeding risk such as the PRECISE DAPT score [43][63] and the Academic Research Consortium High Bleeding Risk (ARC-HBR) criteria [44][45][64,65], may be helpful, and are recommended by guidelines [46][66]. Although almost all elderly patients satisfy the criteria for the definition of HBR, high thrombotic risk is also concomitant in many patients. This issue is well outlined in the ARC-HBR trade-off model proposed by Urban et al., who reported the results of 1-year clinical outcome of 6641 patients (26% with STEMI or NSTEMI) who underwent PCI with stent implantation and were categorized as HBR according to ARC criteria [47][71]. Prior MI, the presence of diabetes, STEMI presentation and bare-metal-stent implantation were predictors of MI and stent thrombosis in this HBR population. At the 1-year follow-up, slightly less than half of the patients (44.1%) had a greater risk of thrombotic events than major bleeding, and one third of patients faced a comparable risk of either type of adverse events. Of the 1.445 patients included in the ELDERLY-ACS 2 trial, more than two thirds (68%) had prior MI, diabetes or STEMI presentation, thus carrying a high thrombotic risk according to the ARC-HBR trade-off model [48][72]. These data show how HBR and high thrombotic risk coexist in a large number of elderly patients with ACS.5. Antiplatelet Strategies in Elderly ACS Patients
In a recent review on antiplatelet therapy in ACS [49][73], scholars propose different DAPT strategies according to the presence or absence of HBR and high thrombotic risk. As discussed above, in elderly patients only two conditions are to be considered: (1) isolated HBR, and (2) HBR associated with high thrombotic risk. For patients with isolated HBR, short DAPT is likely to be the best strategy. In the MASTER DAPT trial [50][74] that selectively randomized HBR patients (69% aged ≥75 years, 48% with ACS) to 1-month DAPT versus standard DAPT (median 157 days) followed by single antiplatelet agent (mostly clopidogrel in both groups), the abbreviated DAPT strategy was non-inferior to standard therapy for net adverse clinical events (NACE) and for ischemic events, but significantly reduced for major or clinically relevant non-major bleeding. This trial, however, also included patients taking anticoagulants (39%), for whom guidelines recommend an early DAPT cessation (1 week). The 1-month DAPT trial showed similar data [51][75]; that is, non-inferiority of short DAPT versus standard (6- to 12-month) DAPT followed by aspirin monotherapy for the 1-year composite of cardiovascular events or major bleeding in patients undergoing PCI for non-complex lesions [51][75]. However, in that trial a significant interaction was observed between treatment strategy and clinical presentation: ACS patients randomized to 1-month DAPT, contrary to stable ones, showed a numerical increase in cardiovascular events with no difference in bleeding as compared to standard-DAPT patients. These data caution against very short (1-month) DAPT periods followed by aspirin monotherapy in ACS patients [52][76].