Macroion assemblies form an efficient scaffold for GF adsorption. Such assemblies enable the targeted delivery of these proteins without losing their activity. Specific attention is given to three types of growth factors: vascular endothelial growth factors, human fibroblast growth factors, and neurotrophins, as well as selected biocompatible synthetic macroions (obtained through standard polymerization techniques) and polysaccharides (natural macroions composed of repeating monomeric units of monosaccharides). Understanding the mechanisms by which growth factors bind to potential carriers could lead to more effective delivery methods for these proteins, which are of significant interest in the diagnosis and treatment of neurodegenerative and civilization diseases, as well as in the healing of chronic wounds.
1. PAH-Based Assemblies
PAH-based assemblies were applied for rapid tissue integration and to avoid prosthetic rejection stimulation of transprosthetic vascularization. For this purpose, the surface of porous titanium implants was modified by PAH/PSS (poly(sodium-4-styrenesulfonate) films functionalized with VEGF
[1][336]. The VEGF adsorbed on the (PAH/PSS)
4 multilayers maintained its bioactivity in vitro and stimulated endothelial cell proliferation. NTs such as BDNF incorporated into the PAH/PSS films remained functional forming functionalized nanofilms
[2][337].
2. BPEI-Based Assemblies
BPEI was successfully applied as a carrier for delivering VEGF isoforms. An increasing factor transfection efficiency without a lowering of cell viability was observed
[3][338]. Using bPEI as a carrier revealed the possible application of VEGF in gene therapy for the treatment of wounds and cardiovascular diseases. The same complex type can be applied as a potential agent for the treatment of myocardial ischemia. The efficacy of that complex was compared with PAMAM-VEGF. However, the bPEI complex induced lower relative viabilities of cells by half compared to that formed by PAMAM-VEGF (95%)
[4][339].
Interesting results based on the coacervation of VEGF with PEI and CS were reported by Huang et al.
[5][340]. VEGF encapsulation efficiency (∼85%) and GF release (10 days) depended on polycation type and were the highest for the complexes based on CS. However, both VEGF-based coacervates effectively stimulated endothelial cell proliferation.
3. PAMAM Dendrimer-Based Assemblies
PAMAM dendrimer-covered surfaces have shown to be a suitable platform for the grafting of VEGF, FGFs and NTs
[4][6][7][8][9][10][11][12][13][58,126,128,266,270,339,341,342,343]. VEGF-PAMAM complexes were successfully applied in theranostics for inducing the apoptosis of cancer cells as well as the inhibition of tumour cell growth
[12][13][342,343]. It was found that the bioconjugates were effective in cardiovascular disease treatment
[4][339] and wound treatment
[8][128]. Furthermore, the VEGF-PAMAM assemblies were successfully used in the boron neutron capture therapy (BNCT) of cancer, as was presented in the pioneering work of Backer et al.
[13][343]. The authors found that fluorescently labelled PAMAM dendrimers, equipped with 102 to 110 decaboranes and VEGF, accumulate in the tumour periphery in vitro where angiogenesis was most active. Thus, these bioconjugates can be effective as a targeting agent for the BNCT of the tumour neovasculature. Arginine (ARG)-grafted PAMAM dendrimers combined with plasmid DNA encoding VEGF led to the development of an effective method to treat diabetic skin wounds, as demonstrated by Kwon et al.
[8][128].
Besides the PAMAM-VEGF coacervates, the complexes based on the FGFs can be applied for wound healing, as reported by Thomas et al.
[7][126]. It was also shown that the PAMAM-FGF1 complexes can serve as a platform for cytosolic and nuclear drug delivery in tumour cells, and as an FGF delivery agent for angiogenesis. The conjugation of PAMAM dendrimers with peptides obtained from FGF3 allowed for the formation of a novel PAMAM-based vector with enhanced gene expression efficiency
[11][341]. The heparin-PAMAM assemblies effectively bind FGF2, which enables the design of new anti-inflammatory drugs with minimal side effects
[6][58].
Dąbkowska et al. applied complexes based on PAMAM dendrimers for the continuous delivery of the NTs for the treatment of neurodegenerative disorder
[9][10][266,270]. The detailed physicochemical characteristics of the assemblies were investigated, and the sizes, zeta potentials, and the stabilities of obtained complexes were determined. They were formed by generation 5.5 PAMAM and BDNF
[9][266], as well as generation 6 PAMAM and NT 4/5
[10][270], respectively. Both were negatively charged in physiological conditions. The obtained results show great potential for the design of stable drug-delivery systems that are crucial for the neuroprotection and treatment of damaged retinal neurons.
4. PAE and PAA-Based Assemblies
MM based on PAE and polyanion PAA allow for the composing of biocompatible and functional nanofilms with high loading efficiency and short buildup times. Such MM were also successfully applied for the loading and releasing of active FGF2
[14][344]. In the follow-up studies, the P.T. Hammond group constructed LbL films with tunable VEGF delivery via degradable PAEs and PAA. It resulted in no burst release of the GF. The release of VEGF was discharged from the MM after just 8 days
[15][249].
5. CS-Based Assemblies
CS-based scaffolds were examined in terms of GF incorporation and delivery
[16][17][345,346]: heparin functionalized CS–alginate scaffolds with FGF2 for tissue regeneration
[18][347], CS/collagen composite scaffold containing recombinant human bone morphogenetic protein-2 (rhBMP-2) for dental implant osseointegration
[19][348], a brushite–CS system, which controls the release kinetics of incorporated VEGF to enhance bone healing
[20][349] as well as in the form of macroion complexes (hydrogel) with negatively charged GAGs
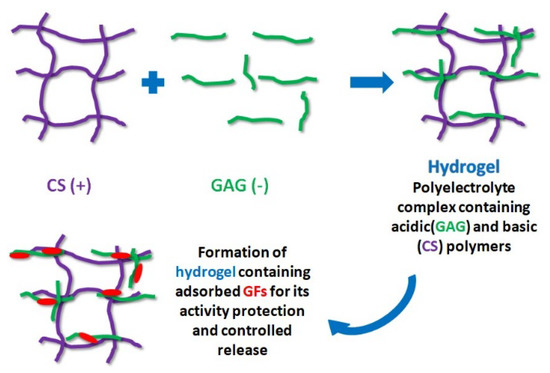
[21][350]. The formation of hydrogel with GAGs is schematically presented in
Figure 1.
Figure 1. Polyelectrolyte complex containing CS (violet chains) and GAG (green chains) as a substrate for adsorption, activity preservation, and the controlled release of GFs (red macromolecules).
CS was also evaluated as local implants in the form of microspheres and fibres for sustained release depots of endothelial growth factors
[17][346].
6. Heparin-Based Assemblies
Heparin is one of the most commonly used macroions for FGF binding. Binding heparin to FGF2 improves the protein bioactivity and stability, highly increases GF mitogenic potential, and preserves FGF2 from heat, pH changes, and proteolysis
[22][13]. Heparin/ChS films also enhanced FGF2 activity. FGF2 released from these MM retained their in vitro activity and promoted the proliferation of preosteoblast cells
[22][13]. When FGF1 is incorporated into the heparin/bPEI multilayers, it enhances the viability and proliferation of the fibroblasts
[23][351].
The effective adsorption of FGF2 on heparin-terminated MM is reported in Refs.
[24][25][352,353], where the adsorption kinetics and the maximum surface concentration (120 ng/cm
2) of the GF were determined in physiological conditions. Furthermore, the FGF2 layer was found to be bioactive, and stimulated both the proliferation and the differentiation of the calf pulmonary arterial endothelial cells
[25][353]. In addition, a greater cell density and a higher proliferation rate of mesenchymal stem cells than any of the other tested conditions were observed when FGF2 was adsorbed onto heparin-terminated multilayers
[26][354]. The biological activities of the FGF2 and heparin released from decellularized porcine aortic heart valve leaflets were confirmed by De Cock et al.
[27][355]. The release of heparin and FGF2 from the scaffold under physiological conditions was sustained over 4 days while preserving the biological activity of the released GF.
The heparin-based MM were also applied for the controlled immobilisation of NTs: NGF and BDNF. Such platforms show enhanced neurite outgrowth in comparison to control surfaces
[28][356]. VEGF is also effectively adsorbed on the top of MM terminated by heparin. When the MM is formed by CS/alginate/carrageenan/heparin, VEGF creates an active layer for human adipose-derived stem cell proliferation
[29][215]. The coacervates based on heparin-binding peptides were applied for providing the prolonged release of NGF, BDNF and NT3 to nerve regeneration by Sakiyama-Elbert
[30][357].
7. ChS-Based Assemblies
The effective adsorption of FGF2 on MM, with ChS as the outer layer, was successfully developed by Tezcaner et al.
[31][358]. The researchers showed that FGF2 deposits on ChS-terminated films can stimulate the attachment of photoreceptor cells and maintain the differentiation of rod and cone cells. The wettability of ChS/FGF2 multilayers was also determined
[32][12]. The measurements revealed that the ChS layer (with a contact angle 55°–60°) is more hydrophilic than the FGF2 layer (with a contact angle 65°–70°). Moreover, the FGF2 layer adsorbed on ChS was stable. Only 30% of the incorporated FGF2 was released within 8 days. Surprisingly, it was found that collagen layer covered ChS/FGF2 films have a better ability to stimulate fibroblast proliferation than FGF2, where it served as an outer layer.
Interesting results relating to the interactions of FGF1 and FGF2 with heparin, ChS and λ-carrageenan were obtained by Sun et al.
[33][59]. Those polysaccharides effectively attached FGF1 and FGF2 and increased their thermal stability for a longer time. Thus, it was confirmed that the polysaccharides bind and stabilize FGFs, and also potentiate their activity and control their delivery.
8. Hydrogel-Based Polysaccharides Containing GFs
Hydrogel formation is a novel strategy in wound dressing, since loading growth factors into a hydrogel to construct a sustained-release system is considered a promising approach to improve wound healing
[34][359]. Such a material not only promotes tissue regeneration but also prevents skin scarring. Hydrogel-based polysaccharides also provide the stability of GFs and their effective delivery. For example, CS, heparin and HA-based hydrogels form assemblies with VEGF, FGFs and NTs
[30][35][36][37][357,360,361,362], where the activity of GFs
[35][36][360,361] is enhanced.
FGF1, FGF2 and VEGF have been incorporated into CS hydrogels, where they induced neovascularization
[35][360] as well as contraction and acceleration of wound closure
[36][361]. Both FGFs and VEGF, trapped in the hydrogel, remained in their active form and accelerated the proliferation of the cells
[35][360]. Hydrogels based on heparin allow for controlled VEGF release and promote the healing of diabetic wounds
[37][362].
ChS, heparin, and HA were applied for the formation of biocompatible hydrogels for wound repair
[38][363]. Those biomaterials controlled the release FGF2 in vivo. It was found that the released amount of FGF2 increases with lower percentages of heparin. In addition, efficient neovascularization was determined for the hydrogel containing ChS, heparin, HA and FGF2. Furthermore, it was found that the release rate of FGF2 from MM increases with decreasing pH
[39][364].
Jha et al.
[40][365] developed a series of hydrogels based on heparin-functionalized HA and investigated the effect of heparin molecular weight as well as its relative concentration on the loading efficiency and retention behaviour of the GF. The results demonstrated that gels based on heparin with high molecular mass facilitated GF loading and retention. Moreover, HA-based hydrogels functionalized with HMW heparin effectively bind GF and induce a more robust differentiation of stem cells into endothelial cells, which further stimulated the vascular-like network formation within the hydrogels.
The coacervates based on HA were successfully applied as VEGF carriers
[41][42][366,367]. Parajó et al. used HA/CS gel nanoparticles for the delivery of VEGF
[41][366]. The obtained HA/CS system, exhibiting good stability and low cytotoxicity, was able to entrap (association value of 94%) and release VEGF within 24 h. VEGF was also attached to nanogels containing HA to induce angiogenesis in order to prevent heart failure
[42][367]. The authors found that the system was biocompatible and significantly improved angiogenesis. HA-heparin conjugate gel, formed by amine-modified HA bound to oxidized heparin, was also applied for the binding and controlled release of FGF2
[43][368]. It is worth noting that released FGF2 was biologically active in stimulating cell growth in vitro. Besides FGFs, HA-based gels were applied for the efficient delivery of NTs, such as BDNF, that demonstrate the utility of HA-based coacervates as a platform for localized gene therapies after spinal cord injury
[44][369].