Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Peter Tang and Version 1 by João C. Silva.
This entry provides a summary of the main features of the periodontium and describes the currently available treatments for periodontal disease.
- periodontium
- periodontitis
- periodontal regeneration
1. Introduction
Periodontitis is a chronic inflammatory infection of the periodontium, the structure responsible for ensuring tooth attachment and stability [1]. Bacterial dental plaque accumulation causes this infection, which can lead to the inflammation and destruction of the periodontium and, ultimately, tooth loss [2]. Advanced stages of the disease require regenerative procedures to restore the lost tissues, which include membranes for guided tissue regeneration (GTR) and bone grafts. However, these current treatments lack effective strategies to induce tissue repair and coordinated regeneration of all periodontal tissues, increasing the demand for alternative solutions to improve clinical outcomes [3].
2. Periodontal Tissue Features and Periodontal Disease
The periodontium is a complex structure composed of hard and soft tissues that support the tooth. It has an important role of ensuring tooth attachment to the bone of the jaw and allowing the teeth to withstand the forces of mastication. The periodontium consists of alveolar bone, root cementum, and periodontal ligament (PDL) [7][4]. The anatomy of the periodontium is illustrated in Figure 1.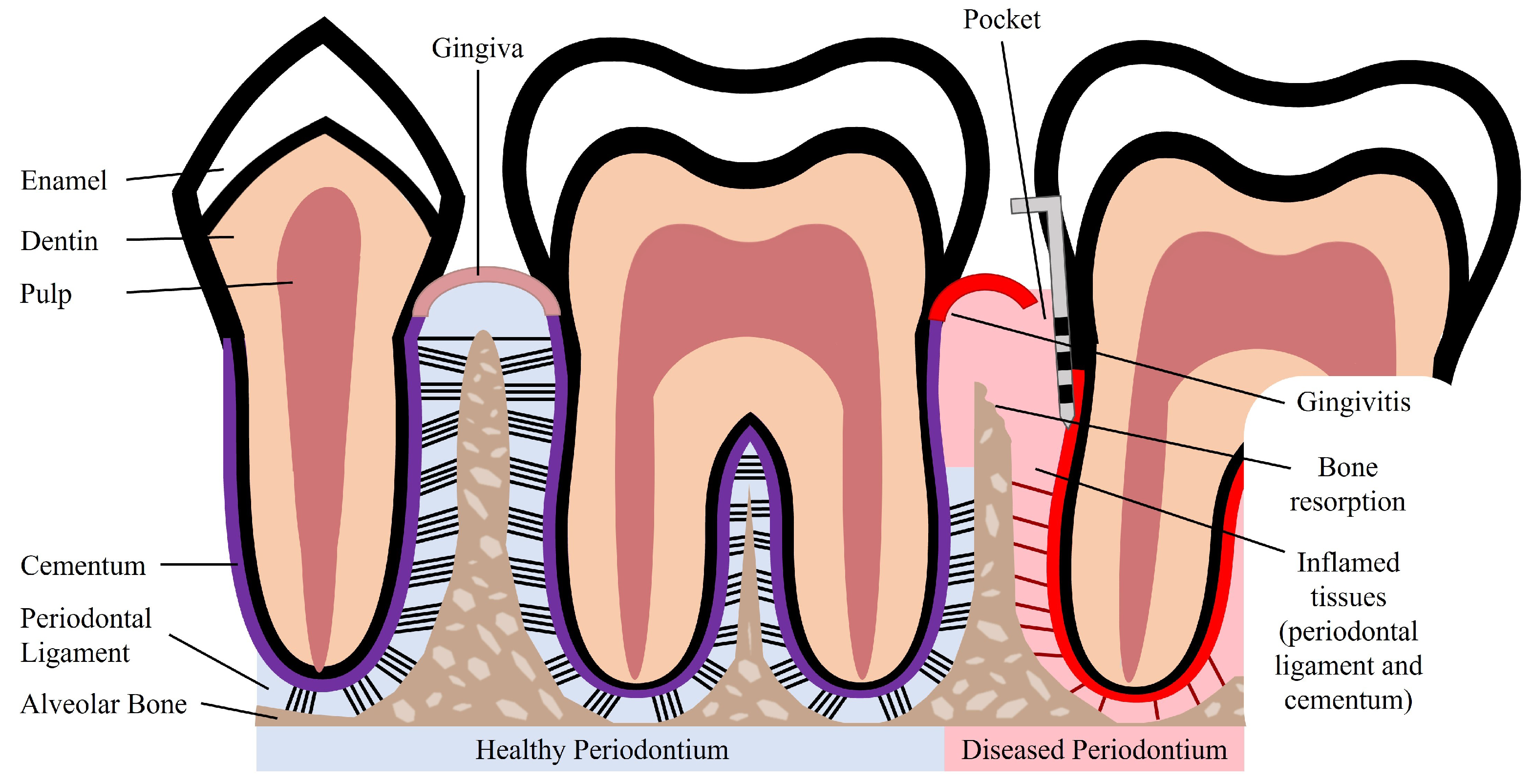
Figure 1.
Schematic illustration of a healthy and diseased periodontium.
3. Currently Available Treatments for Periodontal Disease
Initial stages of periodontitis can be treated with non-surgical procedures such as dental plaque and tartar removal with scaling and root planing [1,18][1][15]. The main goal of these treatments is to control and reduce bacterial plaque accumulation. After the clinical removal of the dental plaque, the patient should practice adequate oral hygiene to achieve a good clinical outcome [18][15]. Non-surgical treatments can be combined with adjunctive therapies, such as local drug delivery, systemic antibiotics, and systemic host response modulation to improve treatment outcomes. Adjunctive drugs include antibiotics and antimicrobials that are directly administered to the periodontal pocket via a gel or fiber delivery system. Examples of systemic antibiotics are amoxicillin and metronidazole, which in combination result in pronounced clinical improvements [18][15]. Host response modulation can be particularly beneficial for patients susceptible to disease development. Host modulatory therapies influence the destructive components of the host response to reduce periodontal tissue destruction. These therapies include non-steroidal anti-inflammatory drugs: doxycycline that downregulates collagenases in inflamed periodontal tissues; and bisphosphonates, which reduce osteoclast activity and bone resorption [1]. Non-surgical treatments have been shown to reduce pocket depth and allow formation of new tooth attachment, which can be sufficient for early to moderate stages of periodontitis. However, in some cases and in advanced stages of the disease, surgical therapy is necessary to access sites deeper in the tooth root to control the inflammation, to fully eliminate bacterial plaque, and to stimulate the regeneration of lost periodontal tissues [18][15]. Pocket reduction surgery is a procedure that involves resecting soft and hard necrotic tissues. Regenerative surgery includes GTR membranes and bone grafts, which are illustrated in Figure 2. An innovative adjuvant is the use of laser treatment in non-surgical or surgical procedures [25][22]. The surgical and non-surgical currently available methods used to treat periodontitis are summarized in Table 1.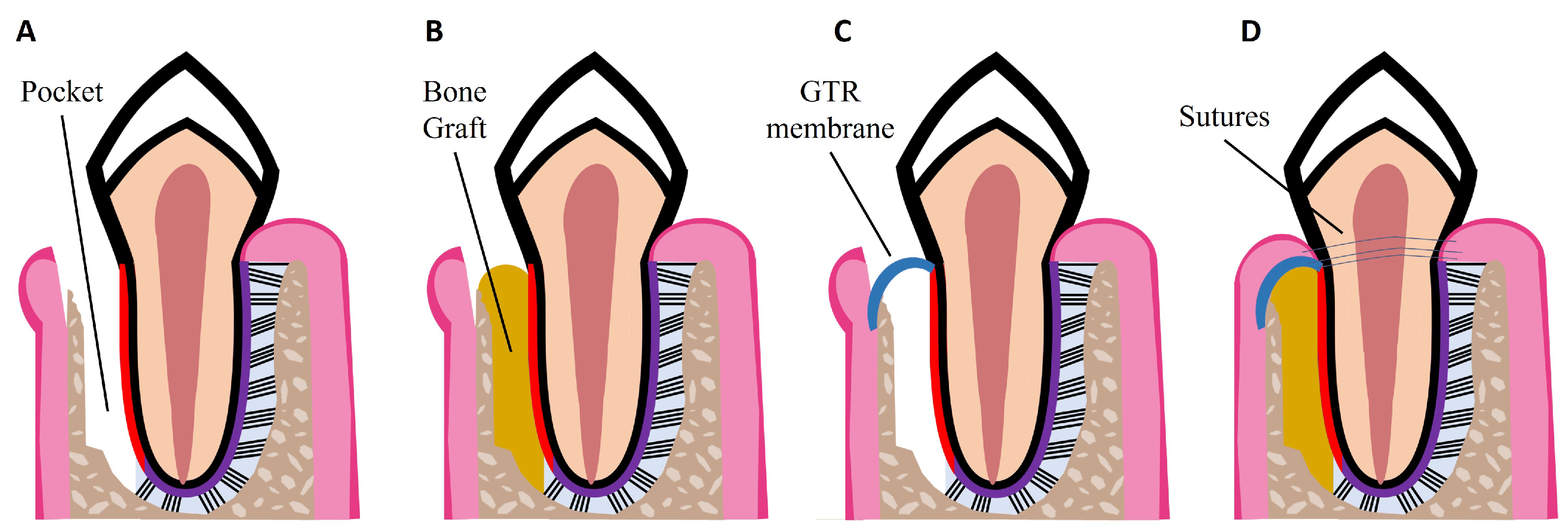
Figure 2. Schematic illustrations of procedures for periodontal regeneration. (A) Loss of PDL and alveolar bone, resulting in periodontal pocket formation. (B) Bone graft placed in the defect site. (C) GTR membrane placed over the defect site. (D) Combination of GTR membrane and bone graft. Wound closure with sutures.
Table 1.
Currently available non-surgical and surgical treatments for periodontal disease.
References
- Preshaw, P.M.; Seymour, R.A.; Heasman, P.A. Current Concepts in Periodontal Pathogenesis. Dent. Update 2004, 31, 570–578.
- Nazir, M.A. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int. J. Health Sci. 2017, 11, 72–80.
- De Jong, T.; Bakker, A.D.; Everts, V.; Smit, T.H. The intricate anatomy of the periodontal ligament and its development: Lessons for periodontal regeneration. J. Periodontal Res. 2017, 52, 965–974.
- Newman, M.G.; Takei, H.H.; Klokkevold, P.R.; Carranza, F.A. Newman and Carranza’s Clinical Periodontology; Elsevier: Amsterdam, The Netherlands, 2019.
- Fehrenbach, M.J.; Popowics, T. Illustrated Dental Embryology, Histology, and Anatomy; Saunders: Maryland Heights, MO, USA, 2015.
- Goudouri, O.M.; Kontonasaki, E.; Boccaccini, A.R. Layered scaffolds for periodontal regeneration. In Biomaterials for Oral and Dental Tissue Engineering; Woodhead Publishing: Sawston, UK, 2017; pp. 279–295.
- Kumar, G.S. Orban’s Oral Histology and Embryology; Elsevier: Haryana, India, 2019.
- Cho, M.I.; Garant, P.R. Development and general structure of the periodontium. Periodontology 2000, 24, 9–27.
- Bosshardt, D. Are Cementoblasts a Subpopulation of Osteoblasts or a Unique Phenotype? J. Dent. Res. 2005, 84, 390–406.
- Jiang, N.; Guo, W.; Chen, M.; Zheng, Y.; Zhou, J.; Kim, S.G.; Embree, M.C.; Song, K.S.; Marao, H.F.; Mao, J.J. Periodontal Ligament and Alveolar Bone in Health and Adaptation: Tooth Movement. Front. Oral Biol. 2015, 18, 1–8.
- Nanci, A.; Bosshardt, D.D. Structure of periodontal tissues in health and disease. Periodontology 2006, 40, 11–28.
- Wu, B.; Fu, Y.; Shi, H.; Yan, B.; Lu, R.; Ma, S.; Markert, B. Tensile testing of the mechanical behavior of the human periodontal ligament. BioMed. Eng. Online 2018, 17, 172.
- Jia, L.N.; Zhang, X.; Xu, H.Y.; Hua, F.; Hu, X.G.; Xie, Q.; Wang, W.; Jia, J. Development of a Doxycycline Hydrochloride-Loaded Electrospun Nanofibrous Membrane for GTR/GBR Applications. J. Nanomater. 2016, 2016, 6507459.
- Sanz, M.; D’aiuto, F.; Deanfield, J.; Fernandez-Avilés, F. European workshop in periodontal health and cardiovascular disease—Scientific evidence on the association between periodontal and cardiovascular diseases: A review of the literature. Eur. Heart J. Suppl. 2010, 12, B3–B12.
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038.
- Botelho, J.; Machado, V.; Leira, Y.; Proença, L.; Chambrone, L.; Mendes, J.J. Economic burden of periodontitis in the United States and Europe: An updated estimation. J. Periodontol. 2022, 93, 373–379.
- Bui, F.Q.; da Silva, C.L.C.A.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35.
- Bhuyan, R.; Bhuyan, S.K.; Mohanty, J.N.; Das, S.; Juliana, N.; Juliana, I.F. Periodontitis and Its Inflammatory Changes Linked to Various Systemic Diseases: A Review of Its Underlying Mechanisms. Biomedicines 2022, 10, 2659.
- Kotronia, E.; Wannamethee, S.G.; Papacosta, A.O.; Whincup, P.H.; Lennon, L.T.; Visser, M.; Weyant, R.J.; Harris, T.B.; Ramsay, S.E. Oral Health, Disability and Physical Function: Results From Studies of Older People in the United Kingdom and United States of America. J. Am. Med. Dir. Assoc. 2019, 20, 1654.e1–1654.e9.
- Wilson, N.J.; Lin, Z.; Villarosa, A.; Lewis, P.; Philip, P.; Sumar, B.; George, A. Countering the poor oral health of people with intellectual and developmental disability: A scoping literature review. BMC Public Health 2019, 19, 1530.
- Carli, E.; Pasini, M.; Pardossi, F.; Capotosti, I.; Narzisi, A.; Lardani, L. Oral Health Preventive Program in Patients with Autism Spectrum Disorder. Children 2022, 9, 535.
- Kwon, T.; Lamster, I.B.; Levin, L. Current Concepts in the Management of Periodontitis. Int. Dent. J. 2021, 71, 462–476.
- Slot, D.E.; Valkenburg, C.; Van der Weijden, G.F. Mechanical plaque removal of periodontal maintenance patients: A systematic review and network meta-analysis. J. Clin. Periodontol. 2020, 47, 107–124.
- Sanz-Sánchez, I.; Montero, E.; Citterio, F.; Romano, F.; Molina, A.; Aimetti, M. Efficacy of access flap procedures compared to subgingival debridement in the treatment of periodontitis. A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 282–302.
- Geisinger, M.L.; Kaur, M.; Basma, H. Nonsurgical Periodontal Therapy: A Review of Current Standards of Care and Innovations to Improve Gingival and Periodontal Health. Curr. Oral Health Rep. 2019, 6, 177–187.
- Polak, D.; Wilensky, A.; Antonoglou, G.N.; Shapira, L.; Goldstein, M.; Martin, C. The efficacy of pocket elimination/reduction compared to access flap surgery: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 303–319.
- Liaw, A.; Miller, C.; Nimmo, A. Comparing the periodontal tissue response to non-surgical scaling and root planing alone, adjunctive azithromycin, or adjunctive amoxicillin plus metronidazole in generalized chronic moderate-to-severe periodontitis: A preliminary randomized controlled trial. Aust. Dent. J. 2019, 64, 145–152.
- Liu, Y.; Guo, L.; Li, X.; Liu, S.; Du, J.; Xu, J.; Hu, J.; Liu, Y. Challenges and Tissue Engineering Strategies of Periodontal-Guided Tissue Regeneration. Tissue Eng. Part C Methods 2022, 28, 405–419.
- Valenti, C.; Pagano, S.; Bozza, S.; Ciurnella, E.; Lomurno, G.; Capobianco, B.; Coniglio, M.; Cianetti, S.; Marinucci, L. Use of the Er:YAG Laser in Conservative Dentistry: Evaluation of the Microbial Population in Carious Lesions. Materials 2021, 14, 2387.
- Baldwin, P.; Li, D.J.; Auston, D.A.; Mir, H.S.; Yoon, R.S.; Koval, K.J. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J. Orthop. Trauma 2019, 33.
- Ren, Y.; Fan, L.; Alkildani, S.; Liu, L.; Emmert, S.; Najman, S.; Rimashevskiy, D.; Schnettler, R.; Jung, O.; Xiong, X.; et al. Barrier Membranes for Guided Bone Regeneration (GBR): A Focus on Recent Advances in Collagen Membranes. Int. J. Mol. Sci. 2022, 23, 14987.
- Mancini, L.; Fratini, A.; Marchetti, E. Periodontal Regeneration. Encyclopedia 2021, 1, 87–98.
- Xu, X.; Ren, S.; Li, L.; Zhou, Y.; Peng, W.; Xu, Y. Biodegradable engineered fiber scaffolds fabricated by electrospinning for periodontal tissue regeneration. J. Biomater. Appl. 2021, 36, 55–75.
- Bhatt, R.A.; Rozental, T.D. Bone Graft Substitutes. Hand Clin. 2012, 28, 457–468.
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone grafts and substitutes in dentistry: A review of current trends and developments. Molecules 2021, 26, 3007.
- Kolk, A.; Handschel, J.; Drescher, W.; Rothamel, D.; Kloss, F.; Blessmann, M.; Heiland, M.; Wolff, K.D.; Smeets, R. Current trends and future perspectives of bone substitute materials—From space holders to innovative biomaterials. J. Cranio-Maxillofac. Surg. 2012, 40, 706–718.
More
