Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Beata Sokołowska and Version 2 by Camila Xu.
The global internet (Internet of Things, IoT) and innovative information and communication technologies (IT/ICT) are already ubiquitous in the social and individual lives of people. Among them, a very significant role is played by Extended Reality (XR) and its classic components such as Virtual (VR), Augmented (AR) and Mixed (MR) Reality. There are many indications that these modern technologies (XR, i.e., VR/AR/MR, and 3D printing/scanning, holography, artificial intelligence and machine learning, robotics or online (VR) tele-medicine) will be the basis and determinants of the organization and functioning of contemporary and future generations.
- virtual reality
- virtual exercise and training
- cognitive and motor functions
- brain
- basic and clinical neuroscience
1. Introduction
The global internet (Internet of Things, IoT) and innovative information and communication technologies (IT/ICT) are already ubiquitous in the social and individual lives of people [1][2][3][4][5][6]. Among them, a very significant role is played by Extended Reality (XR) and its classic components such as Virtual (VR), Augmented (AR) and Mixed (MR) Reality [7][8][9][10][11]. There are many indications that these modern technologies (XR, i.e., VR/AR/MR, and 3D printing/scanning, holography, artificial intelligence and machine learning, robotics or online (VR) tele-medicine) will be the basis and determinants of the organization and functioning of contemporary and future generations [12][13][14][15][16][17]. Most likely, they will increasingly affect everyday life, culture, advertisement, business, military, sports, education, science and medicine [18][19][20][21][22][23][24].
This is because these technologies inspire ideas and the possible development of contemporary advanced algorithmic sciences, models of computation, data mining or big data science, and modern (bio) (medical) (neuro) information and communication technologies tools [25][26][27][28]. The findings of neuroscience research focus on the nervous system, especially the brain, its structure and functions, and its importance in both health and disease, simply enabling the implementation of IT/ICT in, for example, sports, education, or basic/clinical neuroscience and computation medicine [29][30][31][32][33][34][35]. On the other hand, these innovative technologies are becoming an increasingly important element in creating new directions of research, from neurobiology, neurogenetics, neurophysiology, neuropsychology, neuropsychiatry, neuropedagogy, and neurogeriatry, through neurotherapy and neurorehabilitation, to (bio)neuroinformatics [36][37][38][39][40][41].
2. Basic Features, Importance and Possibilities of Virtual Exercise and Training
Modern fast-developed game-based virtual reality technologies offer many VR environments as a very interesting and attractive form of serious games; this applies to both cognitive tasks and the physical engagement of participants in such VR worlds. The difference between these professional systems and other games of this type is that the exerciser’s activity is not random, but designed and adapted to the individual’s abilities or needs, and in addition the user and the researcher or therapist can control and even modify the individual (personal) training, and track the VR scores on/offline. In addition, databases of tasks and exercises are prepared and tested in collaboration with various specialists and experts, therapists and neuroscientists [42], including the consideration of the latest finding in neuroscience, such as those on (meta) neuroplasticity, brain asymmetry or mirror neurons phenomena [43][44][45][46][47][48][49][50].
Computer systems with virtual environments enable the graded difficulty and differentiation of individual tasks, which allows better use of cognitive-motor learning strategies [51][52][53]. Hence, researchers even suggest that these IT/ICT technologies have advantages over the conventional models of improvement in implementing motor learning principles and applying sensory biofeedback [54][55][56][57]. Figure 1 presents an example of a menu for selecting the parameters of the Syllables exercise, such as the number of rounds (repetitions), the difficulty level of the task, and the range of movement. Based on the scores obtained by the trainees, the relevant statistics of the measurement parameters are prepared, as well as on/offline partial and summary reports. It is also possible to record actual sessions, and then all materials can be used for further in-depth mathematical and statistical analysis and evaluation of the results and effects obtained. Subsequent degrees of task difficulty involve, among other things, additional cognitive and/or motor elements, and modification of the exercise/test conditions, as well as the addition of distracting elements (distractors). The presence of distractors is significant because it requires greater concentration on the task. For example, studies by Negut’s or Buxbaum’s teams have shown the negative impact of visual and auditory distractors on attentional performance in children with ADHD in the VC test [58], and USN patients in the VRLAT [59] or AD patients in the VR coffee task [60]. Similarly, in theour modeling studies with healthy adults [61][62][63][64], rwesearchers observed a decrease in performance at the highest difficulty levels of exercise with additional elements such as various distractions or other parameters of training sessions (such as shorter exposure/decision time, the greater number of VR objects or commands/tasks).
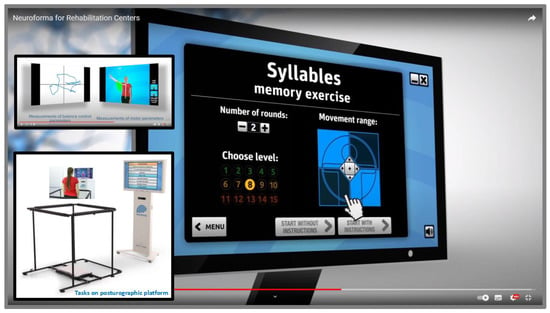
Figure 1. The view of the menu of the Syllables exercise parameters, regarding the selection of the number of rounds, level of difficulty, and range of movement in the VR NEUROFORMA system, and also the view of its version with the posturography platform and safety barriers (materials from ouresearchers' lab repository, with permission of Titanis Ltd.).
Based on the results of a number of neuroscientific studies, researchers and clinicians point out that diagnostic tests using the virtual reality environment have high accuracy, sensitivity and specificity in identifying various dysfunctions and/or deficits in examining subjects with serious illnesses such as neurodevelopmental disorders (e.g., attention-deficit hyperactivity disorder), schizophrenia spectrum (e.g., schizophrenia), mood (e.g., depressive disorders), anxiety (e.g., panic and phobias), trauma- and stressor-related disorders (e.g., post-traumatic stress disorder), neurocognitive (e.g., Alzheimer’s and memory cognitive impairment diseases) and neuromuscular disorders (e.g., multiple sclerosis, amyotrophic lateral sclerosis). Moreover, VR environments can be not only a diagnostics tool, but also an effective (neuro) therapeutic method. In addition, VR systems are increasingly being incorporated into the study of natural aging processes and the estimation of effective support in (neuro) geriatric care (e.g., effective cognitive intervention or prevention of falls in the elderly).
For example, the research group of Msika and co-workers [65], in an interesting study involving healthy young and older adults, proposed using the non-immersive VR REALSoCog task to assess social cognition in normal aging. A total of 27 situations were selected to assess the participants’ social cognitive processes: 11 control/neutral situations and 16 experimental ones. The experimental situations were specifically developed to investigate social norms by displaying conventional and moral transgressions. The researchers found that the REALsoCog task enabled the assessment of several socio-cognitive processes, such as the ability to make moral and conventional judgments, emotional empathy, affective and cognitive ToM (theory of mind), and the propensity to act in a socially appropriate or inappropriate way. The authors noted that the traditional socio-cognitive tasks can evaluate these processes separately and lack ecological validity, and showed that the new virtual approach is an interesting integrative measure of socio-cognitive functioning that better reflects social behavior in daily living.
Equally interesting research is being conducted by the Kourtesis group [66][67] in the immersive environment of the Virtual Reality Everyday Assessment Lab (VR-EAL) using the HTC Vive HMD, which simulates tasks similar to real life to assess prospective memory, episodic memory, executive functions, and selective visual, visuospatial and auditory attention. It is noteworthy that all VR-EAL tasks significantly correlated with relevant ecologically justified paper-and-pencil tests; therefore, performing the VR tasks can be a predictor of the true real-world functioning of individuals. Moreover, the results showed that age and education did not correlate with scores on VR-EAL and paper-and-pencil tests (participants aged 18–45) [66]. The gaming experience was strongly and positively associated with the VR experience, with gamers completing the assessment faster than non-gamers, not only in VR tasks but also in the paper-and-pencil tests. The researchers reported that the VR-EAL is the first immersive VR neuropsychological battery with increased ecological validity for the assessment of everyday cognitive functions, offering an enjoyable testing experience without inducing cybersickness. The authors emphasized that the VR-EAL meets the criteria of the National Academy of Neuropsychology (NAN) and American Academy of Clinical Neuropsychology (AACN), solves some methodological problems and provides benefits in neuropsychological testing. The studies demonstrate that the VR-EAL can be an effective, reliable and ecologically valid tool for assessing (everyday) cognitive function in both research and clinical practice.
In turn, Aubin and colleagues [68] examined how virtual scores of VAP-S relate to the scores of a shopping task in a real-life supermarket. To use VAP-S, participants sat or stood in front of a computer screen and interacted with the virtual environment using a mouse and keyboard. The screen showed instructions and items to buy. During the shopping task, an error was automatically recorded if the participant tried to add an item to the shopping cart that was not on the shopping list or tried to make a purchase more than once. In the next step, the user had to go to checkout and make a payment by clicking on the wallet icon. If the subject did not pay for these purchases, an error was recorded in the test report. The task was completed when the participant left the supermarket with the shopping cart. The authors found that the scores in both environments were generally similar based on the scores of the observational (classical) assessment tool. The researchers noted that when subjects had difficulty with cognitive strategy in the VR supermarket, they also had similar difficulties in the ecological/naturalistic supermarket.
Another team, Zając-Lamparska and colleagues [69], presented the GRANDYS game with the Oculus Rift DK2 and Vbox 6DOF control pad in healthy and MCI older adults. The GRANDYS system is VR-based cognitive training with four modules: attention, memory, language and visuospatial processing. The storyline of each module scenario consists of tasks inspired by daily life. Each module has three levels of difficulty. The game software included a tutorial module to help participants learn how to operate the game interface. In each module, the participants started at the lowest difficulty level and moved up to a higher level in the next session once they had reached 75% accuracy in the previous one. If accuracy fell below 50%, participants returned to a lower difficulty level. Subjects were accompanied by a training assistant throughout the session. This study showed training progress in older adults, larger in the healthy control. Improvements were observed in visuospatial processing, visual aspects of memory and working memory.
The next proposal of the Virtual Reality Lateralized Attention Test (VRLAT) from Buxbaum’s group [59] required participants to navigate a virtual, unbranched path, either propelling themselves using a joystick (the participant condition) or passively viewing the surroundings while the examiner navigated the path at a constant speed (the examiner condition). Participants were asked to identify virtual objects on either side of the path and avoid collisions with them. The software signals collisions with virtual objects, with auditory feedback corresponding to obstructed progress. The VRLAT includes three array conditions (simple, complex, and enhanced), each with 20 target objects (10 on each side of the path). The scoring system adapted in VRLAT awarded points based on the quality of the answers given, e.g., one point for items named specifically and correctly and zero points for any other answer. The maximum possible score for each side at each level would therefore be 20 points (a 20-point scale). These researchers emphasized that patients with a wide range of cognitive and physical ability levels could perform the VRLAT. The authors pointed out that the VRLAT is an easy-to-administer, computerized task that can be run on any standard personal computer without the need for specialized equipment. Moreover, it is not only a diagnostics method but also a useful assessment tool in studies evaluating response to treatment or natural recovery processes after central nervous system injures.
TheOur modeling research focuses on functional brain asymmetry in VR NEUROFORMA [61][62][63][64]. After an initial phase of exercises and learning tasks in this system, healthy subjects practiced the virtual test training sessions at least twice on both hands, the right and left hand, and the same exercises were performed in the full, right and left ranges of motion on a posturographic platform (in random order for each subject). Participants stood in front of a screen with a 3D Kinect camera and saw themselves mirrored among VR objects, and their task was to catch, avoid, track and hit these visuals. The algorithm system awards points for the task performance, estimating scoring distribution as a very good performance in the range of 95–100 points and a good performance in the range of 90–95 points; less than 90 points is not sufficient to advance to a higher level of the exercise. The obtained results indicate that cognitive-motor training in VR with the posturographic platform is a very sensitive and promising tool for recognizing/assessing functional asymmetries of the right-left side of the body, not only in impaired lateralization but also in training sessions of healthy subjects. The primary application of the VR NEUROFORMA system is the role as an innovative and effective therapeutic method that can support conventional (neuro) therapy and/or (neuro) rehabilitation, as demonstrated by Stryla and Banas’ study in ischemic stroke patients [70]. The researchers reported that the VR environment has a motivating effect on patients and allows them to combine an enjoyable time with effective therapeutic exercises/rehabilitation programs. This computer system (similar to others) offers a variety of interesting virtual exercises combining cognitive and motor tasks in a unique dual-task paradigm with the creation of user training in virtual reality, which supports the process of physical and cognitive training/therapy with dynamic biofeedback in the form of attractive serious mini-games (Figure 2).
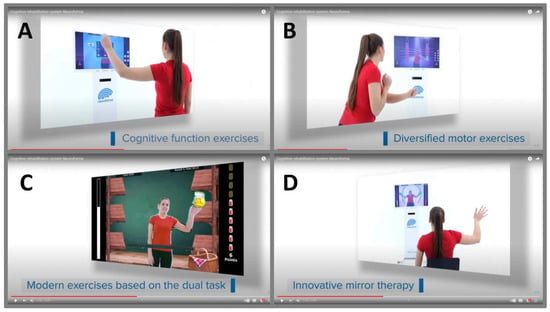
Figure 2. The presentation of examples of various exercises in the VR NEUROFORMA environment, such as (A) the arithmetic operations executive exercise, (B) the opposing boxing motor exercise, (C) the market products cognitive-motor exercise based on the dual task, (D) mirror paths exercise (materials from ouresearchers' lab repository, with the permission of Titanis Ltd.).
Current VR applications indicate an important auxiliary role in improving motor functions, such as joint mobility, muscle strength and endurance, hand-eye coordination, synchronization and control of movement, reaction speed, coordination of opposing movements or balance training with load distribution. Additionally, among the improvements in cognitive functions are effective assistance in focusing attention, inhibiting reflex reactions, exercising memory, improving knowledge management, supporting visual perception, problem-solving, counting and reading, and decision-making processes. In addition, new studies are already emerging showing the beneficial therapeutic effects of not only the classical VR approach, but also the more effective use of mirror VR sessions/training, which are based on the phenomenon of mirror neuron plasticity [71]. Examples of various proposed virtual tasks/exercises that can impact cognitive and motor functions used in the upper limbs and balance control training are shown in Figure 2.
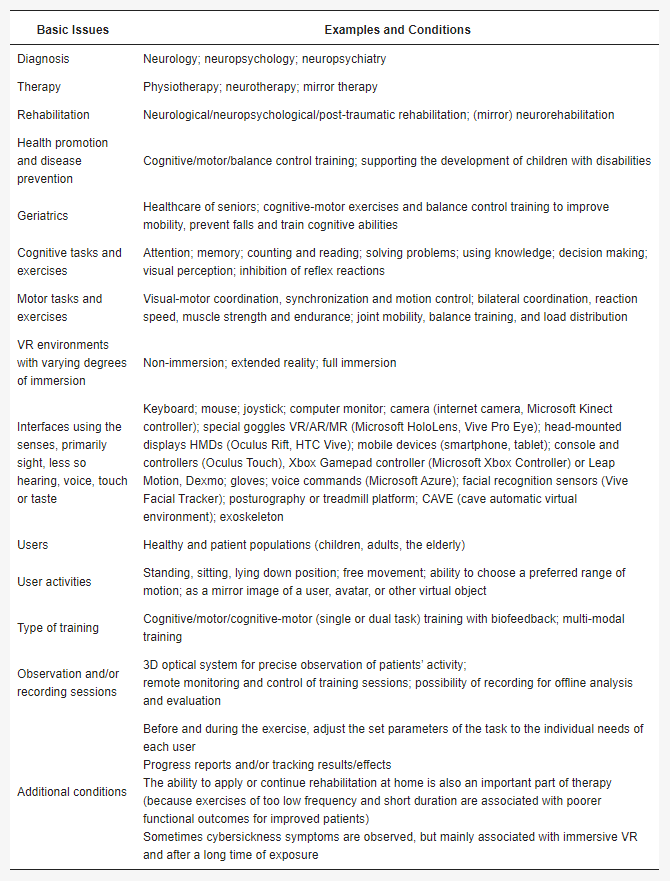
To sum up, new digital technologies are a real hope in view of the prevalence of civilization diseases and the rapid aging of modern societies. As already highlighted, an undoubted benefit of virtual technologies is that they can be used in the home environment. This is particularly evident when opportunities for movement or direct contact with specialists/therapists are limited, e.g., such as during the lockdown caused by the COVID-19 pandemic. Many researchers point to the need to test and validate innovative virtual reality environments and tasks for use in basic and clinical neuroscience [72][73], and thus to formulate recommendations for the design and implementation of VR in clinical screening, diagnosis and therapeutic rehabilitation [74][75][76][77][78]. It should be noted that virtual reality-based assessment can be a good alternative to classical or computer-based neuropsychological assessment due to its greater ecological validity [67][79][80][81]. The basis of physiotherapy is systematic physical exercises adapted to both the severity of the disease and the patient’s effort tolerance. Note that the virtual reality environment allows for safe and systematic exercises, taking into account the capabilities of both healthy individuals and patients. Hence, medical versions of virtual reality are dedicated to a very wide range of users, including different groups of patients. There are a great number of VR interfaces and systems that can be helpful in hospitals, rehabilitation centers and other institutions, providing therapy, rehabilitation or health promotion and disease prevention, especially for the elderly, as shown in Table 1 [18][20][21][22][23][82][83]. Current evidence of the advantages of virtual rehabilitation over traditional exercise is still insufficient, but such training is already a valuable complement to conventional therapy and rehabilitation. Of course, medical applications are of particular importance, raising great hopes in clinical neuroscience, because innovative technologies have huge potential for the unlimited simulation of various situations, individually selected both in terms of exercise/training and the capabilities of each participant.
Table 1.
The summary of VR applications and equipping virtual environments used in basic and clinical neuroscience.
References
- Hennen, L.; Hahn, J.; Ladikas, M.; Lindner, R.; Peissl, W.; van Est, R. Technology Assessment in a Globalized World. Facing the Challenges of Transnational Technology Governance; Springer: Cham, Switzerland, 2023.
- Riva, C.G. Special Topics in Information Technology; Springer: Cham, Switzerland, 2023.
- Werthner, H.; Prem, E.; Lee, E.A.; Ghezzi, C. Perspectives on Digital Humanism; Springer Nature: Cham, Switzerland, 2022.
- Li, H.; Zhang, X.; Wang, H.; Yang, Z.; Liu, H.; Cao, Y.; Zhang, G. Access to Nature via Virtual Reality: A Mini-Review. Front. Psychol. 2021, 12, 725288.
- Sharman, W.R.; Craig, W.R. Understanding Virtual Reality. Interface, Application, and Design, 2nd ed.; Elsevier Science Publisher: New York, NY, USA, 2018.
- Tripathy, B.K.; Anuradha, J. Internet of Things (IoT): Technologies, Applications, Challenges, and Solutions; Taylor & Francis Group: Boca Raton, FL, USA, 2018.
- Suzuki, K.; Mariola, A.; Schwartzman, D.J.; Seth, A.K. Using Extended Reality to Study the Experience of Presence. In Current Topics in Behavioral Neurosciences; Springer: Berlin/Heidelberg, Germany, 2023.
- Skarbez, R.; Smith, M.; Whitton, M.C. Revisiting Milgram and Kishino’s Reality-Virtuality Continuum. Front. Virtual. Real. 2021, 2, 647997.
- Grant, C.; Mairn, C. 3D, virtual, augmented, extended, mixed reality, and extended content forms: The technology and the challenges. Inf. Serv. Use. 2020, 40, 225–230.
- Hudson, S.; Matson-Barkat, S.; Pallamin, N.; Jegou, G. With or without you? Interaction and immersion in a virtual reality experience. J. Bus. Res. 2019, 100, 459–468.
- Milgram, P.; Takemura, H.; Utsumi, A.; Kishino, F. Augmented reality: A class of displays on the reality-virtuality continuum. SPIE Telemanipulator Telepresence Technol. 1995, 2351, 282–292.
- Guerrero, D.T.; Asaad, M.; Rajesh, A.; Hassan, A.; Butler, C.E. Advancing Surgical Education: The Use of Artificial Intelligence in Surgical Training. Am. Surg. 2023, 89, 49–54.
- Curry, E.; Auer, S.; Berre, A.J.; Metzger, A.; Perez, M.S.; Zillner, S. Technologies and Applications for Big Data Value; Springer Nature: Cham, Switzerland, 2022.
- Grassini, S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int. J. Environ. Res. Public. Health 2022, 19, 4071.
- Lai, B.; Davis, D.; Young, R.; Swanson-Kimani, E.; Wozow, C.; Chaviano, K.; Rimmer, J.H. Group Telegaming Through Immersive Virtual Reality to Improve Mental Health Among Adolescents with Physical Disabilities: Pre- and Posttrial Protocol. JMIR Res. Protoc. 2022, 11, e42651.
- Le Noury, P.; Polman, R.; Maloney, M.; Gorman, A. A Narrative Review of the Current State of Extended Reality Technology and How it can be Utilised in Sport. Sport. Med. 2022, 52, 1473–1489.
- Sugimoto, M. Extended Reality (XR:VR/AR/MR), 3D Printing, Holography, A.I., Radiomics, and Online VR Tele-Medicine for Precision Surgery. In Surgery and Operating Room Innovation; Takenoshita, S., Yasuhara, H., Eds.; Springer: Singapore, 2021.
- Palumbo, A. Microsoft HoloLens 2 in Medical and Healthcare Context: State of the Art and Future Prospects. Sensors 2022, 22, 7709.
- van der Putten, K.; Anderson, M.B.; van Geenen, R.C. Looking through the Lens: The Reality of Telesurgical Support with Interactive Technology Using Microsoft’s HoloLens 2. Case Rep. Orthop. 2022, 2022, 5766340.
- Salcedo, D.; Regan, J.; Aebersold, M.; Lee, D.; Darr, A.; Davis, K.; Berrocal, Y. Frequently Used Conceptual Frameworks and Design Principles for Extended Reality in Health Professions Education. Med. Sci. Educ. 2022, 32, 1587–1595.
- Wei, W.; Qin, Z.; Yan, B.; Wang, Q. Application Effect of Motion Capture Technology in Basketball Resistance Training and Shooting Hit Rate in Immersive Virtual Reality Environment. Comput. Intell. Neurosci. 2022, 2022, 4584980.
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080.
- Ibrahim, Z.; Money, A.G. Computer mediated reality technologies: A conceptual framework and survey of the state of the art in healthcare intervention systems. J. Biomed. Inform. 2019, 90, 103102.
- Pennefather, P.; Krebs, C. Exploring the Role of xR in Visualisations for Use in Medical Education. Adv. Exp. Med. Biol. 2019, 1171, 15–23.
- Jackson, K.M.; Shaw, T.H.; Helton, W.S. Evaluating the dual-task decrement within a simulated environment: Word recall and visual search. Appl. Ergon. 2023, 106, 103861.
- Bonkhoff, A.K.; Grefkes, C. Precision medicine in stroke: Towards personalized outcome predictions using artificial intelligence. Brain 2022, 145, 457–475.
- Lyu, L.Q.; Cui, H.Y.; Shao, M.Y.; Fu, Y.; Zhao, R.X.; Chen, Q.P. Computational Medicine: Past, Present and Future. Chin. J. Integr. Med. 2021, 28, 453–462.
- Coscia, M.; Wessel, M.J.; Chaudary, U.; Millán, J.D.R.; Micera, S.; Guggisberg, A.; Vuadens, P.; Donoghue, J.; Birbaumer, N.; Hummel, F.C. Neurotechnology-aided interventions for upper limb motor rehabilitation in severe chronic stroke. Brain 2019, 142, 2182–2197.
- Keawtep, P.; Wichayanrat, W.; Boripuntakul, S.; Chattipakorn, S.C.; Sungkarat, S. Cognitive Benefits of Physical Exercise, Physical–Cognitive Training, and Technology-Based Intervention in Obese Individuals with and without Postmenopausal Condition: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 13364.
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959.
- Palacios-Navarro, G.; Hogan, N. Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis. Sensors 2021, 21, 1111.
- Parr, T.; Limanowski, J.; Rawji, V.; Friston, K. The computational neurology of movement under active inference. Brain 2021, 144, 1799–1818.
- Slutzky, M.W. Brain-Machine Interfaces: Powerful Tools for Clinical Treatment and Neuroscientific Investigations. Neuroscentist 2019, 25, 139–154.
- Diemer, J.; Alpers, G.W.; Peperkorn, H.M.; Shiban, Y.; Mühlberger, A. The impact of perception and presence on emotional reactions: A review of research in virtual reality. Front. Psychol. 2015, 6, 26.
- Burns, A.; Adeli, H.; Buford, J.A. Brain-computer interface after nervous system injury. Neuroscientist 2014, 20, 639–651.
- Khan, A.; Podlasek, A.; Somaa, F. Virtual reality in post-stroke neurorehabilitation—A systematic review and meta-analysis. Top. Stroke Rehabil. 2023, 30, 53–72.
- Chatelain, L.S.; Khalifé, M.; Riouallon, G.; Guigui, P.; Ferrero, E. Pedagogy in spine surgery: Developing a free and open-access virtual simulator for lumbar pedicle screws placement. Eur. Spine J. 2022, 32, 712–717.
- Chaudhary, U.; Mrachacz-Kersting, N.; Birbaumer, N. Neuropsychological and neurophysiological aspects of brain-computer-interface (BCI) control in paralysis. J. Physiol. 2021, 599, 2351–2359.
- Yang, S.; Li, R.; Li, H.; Xu, K.; Shi, Y.; Wang, Q.; Yang, T.; Sun, X. Exploring the Use of Brain-Computer Interfaces in Stroke Neurorehabilitation. Biomed. Res. Int. 2021, 2021, 9967348.
- Rizzo, A.; Bouchard, S. Virtual Reality for Psychological and Neurocognitive Interventions; Springer Science + Business Media: New York, NY, USA, 2019.
- Bassett, D.S.; Gazzaniga, M.S. Understanding complexity in the human brain. Trends Cogn. Sci. 2011, 15, 200–209.
- Website of the ISVR. Available online: https://isvr.org/ (accessed on 24 January 2023).
- Bisiacchi, P.; Cainelli, E. Structural and functional brain asymmetries in the early phases of life: A scoping review. Brain Struct. Funct. 2022, 227, 479–496.
- Bonini, L.; Rotunno, C.; Arcuri, E.; Gallese, V. Mirror neurons 30 years later: Implications and applications. Trends Cogn. Sci. 2022, 26, 767–781.
- Lahuerta-Martín, S.; Llamas-Ramos, R.; Llamas-Ramos, I. Effectiveness of Therapies Based on Mirror Neuron System to Treat Gait in Patients with Parkinson’s Disease-A Systematic Review. J. Clin. Med. 2022, 11, 4236.
- Shimada, S. Multisensory and Sensorimotor Integration in the Embodied Self: Relationship between Self-Body Recognition and the Mirror Neuron System. Sensors 2022, 22, 5059.
- Thiebaut de Schotten, M.; Beckmann, C.F. Asymmetry of brain structure and function: 40 years after Sperry’s Nobel Prize. Brain Struct. Funct. 2022, 227, 421–424.
- Esteves, M.; Ganz, E.; Sousa, N.; Leite-Almeida, H. Asymmetrical Brain Plasticity: Physiology and Pathology. Neuroscience 2021, 454, 3–14.
- Alqadah, A.; Hsieh, Y.W.; Morrissey, Z.D.; Chuang, C.F. Asymmetric development of the nervous system. Dev. Dyn. 2018, 247, 124–137.
- Thieme, H.; Morkisch, N.; Mehrholz, J.; Pohl, M.; Behrens, J.; Borgetto, B.; Dohle, C. Mirror therapy for improving motor function after stroke. CDSR 2018, 7, CD008449.
- Lucena-Anton, D.; Fernandez-Lopez, J.C.; Pacheco-Serrano, A.I.; Garcia-Munoz, C.; Moral-Munoz, J.A. Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1780–1792.
- Keshner, E.A.; Fung, J. The quest to apply VR technology to rehabilitation: Tribulations and treasures. J. Vestib. Res. 2017, 27, 1–5.
- Levin, M.F.; Weiss, P.L.; Keshner, E.A. Emergence of virtual reality as a tool for upper limb rehabilitation: Incorporation of motor control and motor learning principles. Phys. Ther. 2015, 95, 415–425.
- Lee, H.K.; Jin, J. The effect of a virtual reality exergame on motor skills and physical activity levels of children with a developmental disability. Res. Dev. Disabil. 2023, 132, 104386.
- Ferrero, L.; Ortiz, M.; Quiles, V.; Iáñez, E.; Flores, J.A.; Azorín, J.M. Brain Symmetry Analysis during the Use of a BCI Based on Motor Imagery for the Control of a Lower-Limb Exoskeleton. Symmetry 2021, 13, 1746.
- Cano Porras, D.; Siemonsma, P.; Inzelberg, R.; Zeilig, G.; Plotnik, M. Advantages of virtual reality in the rehabilitation of balance and gait. Systematic review. Neurology 2018, 90, 1017–1025.
- Brunner, I.; Skouen, J.S.; Hofstad, H.; Aßmuss, J.; Becker, F.; Pallesen, H.; Thijs, L.; Verheyden, G. Is upper limb virtual reality training more intensive than conventional training for patients in the subacute phase after stroke? An analysis of treatment intensity and content. BMC Neurol. 2016, 16, 219.
- Negut, A.; Jurma, A.M.; David, D. Virtual-reality-based attention assessment of ADHD: ClinicaVR: Classroom-CPT versus a traditional continuous performance test. Child Neuropsychol. 2017, 23, 692–712.
- Buxbaum, L.J.; Dawson, A.M.; Linsley, D. Reliability and validity of the Virtual Reality Lateralized Attention Test in assessing hemispatial neglect in right-hemisphere stroke. Neuropsychology 2012, 26, 430–441.
- Allain, P.; Foloppe, D.A.; Besnard, J.; Yamaguchi, T.; Etcharry-Bouyx, F.; Le Gall, D.; Nolin, P.; Richard, P. Detecting everyday action deficits in Alzheimer’s disease using a nonimmersive virtual reality kitchen. J. Int. Neuropsychol. Soc. 2014, 20, 468–477.
- Sokołowska, B. A Novel Perspective for Examining and Comparing Real and Virtual Test Tasks Performed by the Dominant and Non-Dominant Hand in Healthy Adults. Symmetry 2021, 13, 1810.
- Sokołowska, B. A novel virtual reality approach for functional lateralization in healthy adults. Brain Res. 2021, 1766, 147537.
- Sokołowska, B.; Sokołowska, E. An Example of the Assessment of Human Laterality Using Virtual Reality. IJIRCCE 2019, 7, 3555–3562. Available online: http://ijircce.com/admin/main/storage/app/pdf/KdxZlKhLTCPJ5Fekz5R9wfuhT7qtfDYfS9dn2Atb.pdf (accessed on 24 February 2023).
- Sokołowska, B.; Sokołowska, E. Machine Learning algorithms to study of laterality in Virtual Reality. In Proceedings of the annual INCF Congress of NeuroInformatics 2019, Warsaw, Poland, 1–2 September 2019.
- Msika, E.F.; Ehrlé, N.; Gaston-Bellegarde, A.; Orriols, E.; Piolino, P.; Narme, P. Using a Computer-Based Virtual Environment to Assess Social Cognition in Aging: An Exploratory Study of the REALSoCog Task. Front. Psychol. 2022, 13, 882165.
- Kourtesis, P.; Collina, S.; Doumas, L.A.A.; MacPherson, S.E. Validation of the Virtual Reality Everyday Assessment Lab (VR-EAL): An Immersive Virtual Reality Neuropsychological Battery with Enhanced Ecological Validity. J. Int. Neuropsychol. Soc. 2021, 27, 181–196.
- Kourtesis, P.; MacPherson, S.E. An ecologically valid examination of event-based and time-based prospective memory using immersive virtual reality: The influence of attention, memory, and executive function processes on real-world prospective memory. Neuropsychol. Rehabil. 2021, 29, 486–506.
- Aubin, G.; Béliveau, M.F.; Klinger, E. An exploration of the ecological validity of the Virtual Action Planning-Supermarket (VAP-S) with people with schizophrenia. Neuropsychol. Rehabil. 2018, 28, 689–708.
- Zając-Lamparska, L.; Wiłkość-Dębczyńska, M.; Wojciechowski, A.; Podhorecka, M.; Polak-Szabela, A.; Warchoł, Ł.; Kędziora-Kornatowska, K.; Araszkiewicz, A.; Izdebski, P. Effects of virtual reality-based cognitive training in older adults living without and with mild dementia: A pretest-posttest design pilot study. BMC Res. Notes 2019, 12, 776.
- Stryla, W.; Banas, A. The Use of Virtual Reality Technologies during Physiotherapy of the Paretic Upper Limb in Patients after Ischemic Stroke. J. Neurol. Neurosci. 2015, 6, 33.
- Zhang, Y.; Xing, Y.; Li, C.; Hua, Y.; Hu, J.; Wang, Y.; Ya, R.; Meng, Q.; Bai, Y. Mirror therapy for unilateral neglect after stroke: A systematic review. Eur. J. Neurol. 2022, 29, 358–371.
- Porffy, L.A.; Mehta, M.A.; Patchitt, J.; Boussebaa, C.; Brett, J.; D’Oliveira, T.; Mouchlianitis, E.; Shergill, S.S. A Novel Virtual Reality Assessment of Functional Cognition: Validation Study. J. Med. Internet Res. 2022, 24, e27641.
- Kourtesis, P.; MacPherson, S.E. How immersive virtual reality methods may meet the criteria of the National Academy of Neuropsychology and American Academy of Clinical Neuropsychology: A software review of the Virtual Reality Everyday Assessment Lab (VR-EAL). Comput. Hum. Behav. Rep. 2021, 4, 100151.
- Nath, D.; Singh, N.; Saini, M.; Srivastava, M.V.P.; Mehndiratta, A. Design and Validation of Virtual Reality Task for Neuro-Rehabilitation of Distal Upper Extremities. Int. J. Environ. Res. Public Health 2022, 19, 1442.
- Rey, B.; Oliver, A.; Monzo, J.M.; Riquelme, I. Development and Testing of a Portable Virtual Reality-Based Mirror Visual Feedback System with Behavioral Measures Monitoring. Int. J. Environ. Res. Public Health 2022, 19, 2276.
- Brassel, S.; Power, E.; Campbell, A.; Brunner, M.; Togher, L. Recommendations for the Design and Implementation of Virtual Reality for Acquired Brain Injury Rehabilitation: Systematic Review. J. Med. Internet Res. 2021, 23, e26344.
- Bell, I.H.; Nicholas, J.; Alvarez-Jimenez, M.; Thompson, A.; Valmaggia, L. Virtual reality as a clinical tool in mental health research and practice. Dialogues Clin. Neurosci. 2020, 22, 169–177.
- Kourtesis, P.; Korre, D.; Collina, S.; Doumas, L.A.; Macpherson, S.E. Guidelines for the Development of Immersive Virtual Reality Software for Cognitive Neuroscience and Neuropsychology: The Development of Virtual Reality Everyday Assessment Lab (VR-EAL), a Neuropsychological Test Battery in Immersive Virtual Reality. Front. Comput. Sci. 2020, 1, 12.
- Cavedoni, S.; Cipresso, P.; Mancuso, V.; Bruni, F.; Pedroli, E. Virtual reality for the assessment and rehabilitation of neglect: Where are we now? A 6-year review update. Virtual Real. 2022, 30, 1663–1704.
- Giannakou, I.; Lin, D.; Punt, D. Computer-based assessment of unilateral spatial neglect: A systematic review. Front. Neurosci. 2022, 16, 912626.
- Cogné, M.; Taillade, M.; N’Kaoua, B.; Tarruella, A.; Klinger, E.; Larrue, F.; Sauzéon, H.; Joseph, P.A.; Sorita, E. The contribution of virtual reality to the diagnosis of spatial navigation disorders and to the study of the role of navigational aids: A systematic literature review. Ann. Phys. Rehabil. Med. 2017, 60, 164–176.
- Jonson, M.; Avramescu, S.; Chen, D.; Alam, F. The Role of Virtual Reality in Screening, Diagnosing, and Rehabilitating Spatial Memory Deficits. Front. Hum. Neurosci. 2021, 15, 628818.
- Kaplan, A.D.; Cruit, J.; Endsley, M.; Beers, S.M.; Sawyer, B.D.; Hancock, P.A. The Effects of Virtual Reality, Augmented Reality, and Mixed Reality as Training Enhancement Methods: A Meta-Analysis. Hum. Factors 2021, 63, 706–726.
More
