Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 1 by Elyse M. Cornett.
Exogenous melatonin is commonly used to treat insomnia, other sleep problems, and numerous medical illnesses, including Alzheimer’s disease, autism spectrum disorder, and mild cognitive impairment in adults and children. There is evolving information regarding issues with the use of chronic melatonin.
- melatonin
- insomnia
- sleep
- aging
- dietary supplement
- autistic spectrum disorder
1. Anti-Aging and Oxidation Protection
Mitochondrial dysfunction is related to several age-related diseases, such as AD and cardiovascular disease, caused by oxidative stress induced by the buildup of ROS. The production of melatonin is not only found within the pineal gland. Some studies have found melatonin production within bone marrow, retina, and gastrointestinal tract [38][1]. These extra pineal sources of melatonin are produced within mitochondria of the tissues above, and this production significantly decreases with age, with mitochondrial dysfunction increasing. A thorough review published in 2022 discussed the causative factors of aging and how the decrease in melatonin production may be an important factor in aging [39][2]. Gimenez et al. summarized how exogenous administration of melatonin reduces the oxidation of compounds such as cardiolipin, implicated in cardiovascular disease, and its inhibition in proinflammatory events such as COX-2, amyloid beta toxicity, and mTOR signaling (refer to Figure 1) [39][2]. The reduction of oxidation of compounds related to mitochondrial function may be implicated in an “anti-aging” effect. Essentially, melatonin may preserve mitochondrial function, thus preventing the vicious cycle of oxidative damage that arises in concordance with aging and age-related diseases that have exhibited an ever-increasing incidence within the U.S. population.
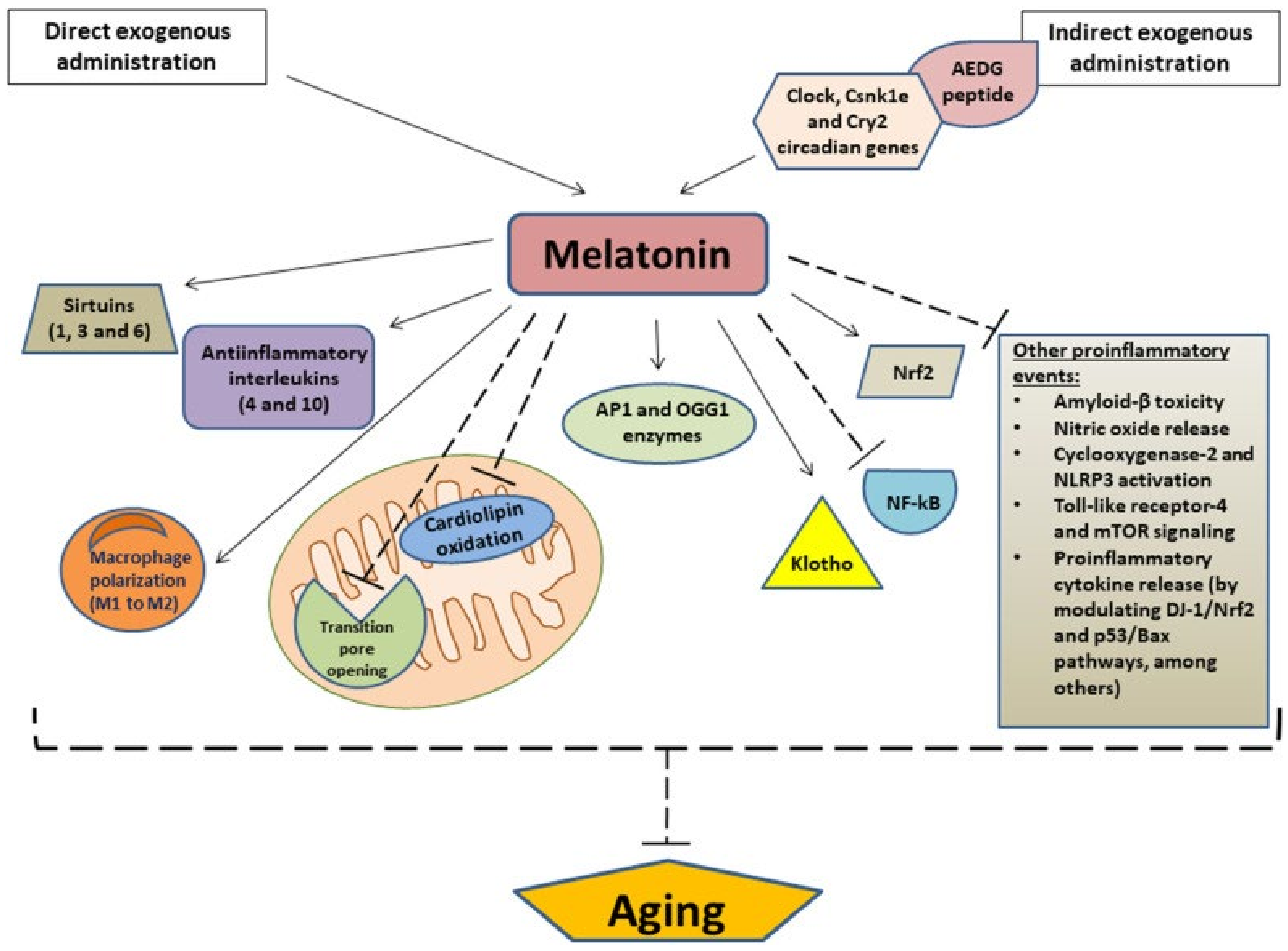
Figure 1. Gimenez et al. details the downstream and potential anti-aging effects of exogenous administration of melatonin. Arrows indicate stimulation, and dashed lines indicate inhibition. AEDG, (Ala-Glu-Asp-Gly) peptide; APE1, Apurinic/apyrimidinic endonuclease 1; OGG1, (8-Oxoguanine glycosylase); Nrf2, nuclear factor erythroid 2-related factor 2; NF-κB, nuclear transcription factor kappa B; NLRP3, NOD-like receptor family pyrin domain-containing 3; mTOR, mammalian target of rapamycin [31][3].
2. Melatonin as a Potential Marker in Alzheimer’s Disease
The diagnosis and determination of progression of AD is obtained via many tests, including PET scanning for the uptake of flurodeoxyglucose indicating the presence of amyloid beta plaques and tau fibers [40][4]. Historically, it has been troublesome to use biomarkers within liquid media to track the progression of AD. A 2021 study found a significant difference in nighttime circulating levels of melatonin in AD and age-matched individuals, suggesting this may be a new biomarker to consider in clinical practice; however, more studies need to be performed in order to further evaluate the use of circulating melatonin as a diagnostic tool for this disease [41][5].
3. Therapeutic for Mild Cognitive Impairment
MCI is a condition that involves impairment of an individual’s memory, reasoning, or perception. This condition is implicated in the progression of AD as an early-stage finding that can be diagnosed with concurrent imaging showing beta-amyloid plaques or tau fibers on a PET scan [42][6]. A systematic review and meta-analysis of over 22 randomized control trials found that melatonin usage significantly increased the Mini-Mental State Examination score in patients suffering from mild AD [43][7]. This finding suggests that melatonin may be an effective adjuvant therapeutic option for improving MCI in patients suffering from mild AD.
4. Delay of Puberty
There has been concern that long-term exogenous melatonin might delay children’s sexual maturation. This stems from the observation that the highest nighttime melatonin levels are found in very young individuals (1–3 years) and that levels drop progressively until adolescence. The drop in nocturnal serum melatonin levels parallels the sexual maturation process. Therefore, it has been hypothesized that artificially keeping melatonin levels high might not allow the triggering of important pubertal developmental steps.
Boafo et al. [44][8] analyzed three human studies that tracked pubertal timing along long-term exogenous melatonin use. The primary focus was melatonin effectiveness or dosing in all three studies, with pubertal timing as a secondary outcome. One study [31][3] showed no effect on pubertal development based on Tanner scores. A second study [25][9] showed “perceived pubertal timing as late” (a subjective delay) in melatonin users compared to controls. In a third study [27][10], out of 44 children with severe neurodevelopmental difficulties, 5 developed precocious puberty before starting melatonin therapy; however, there was no apparent impact on the onset of puberty in the remaining 39 subjects. Boafo et al. [44][8] concluded that the number of patients studied was too small to draw reliable conclusions, patient follow-up was incomplete, and measures of pubertal timing were poor. They concluded that the role of melatonin in sexual maturation and the timing of puberty is understudied, and thus, that additional research is necessary.
5. Effect on Seizures
There has been concern that melatonin may increase the incidence of seizures in those with a seizure disorder [45][11]. However, no effect on seizure activity was observed in a randomized, placebo-controlled trial in children by Wasdell et al. [28][12] or by Carr et al. [27][10]. Another study found a decrease in seizures in children who took exogenous melatonin to improve sleep [46][13]. In patients with epilepsy with idiopathic generalized tonic-clonic seizures, Maghbooli et al. found that the addition of melatonin to patients’ valproic acid treatment was associated with a significant reduction in the severity of epilepsy and improvement in sleep quality [47][14].
6. Increase in Bone Fractures
There have been reports of increased risk of bone fracture associated with exogenous melatonin [45][11]. A study of adults in the United Kingdom by Frisher et al. [48][15] found that adults (average age 65) who received 3 or more melatonin prescriptions (2 mg, extended release) were 44% more likely to suffer a fracture than the control group. Until the association between melatonin and fractures has been clarified, the possibility of increased fracture risk is a reason to use melatonin with caution in older adults and those with previous low-impact fractures.
7. Impairment of Balance or Cognition
There have been concerns that exogenous melatonin could impair balance or cognition. Immediate-release melatonin is cleared quickly from the system. Oral, immediate-release melatonin has a half-life of approximately 45 min and time to peak blood concentration of approximately 30 min. A single oral dose of melatonin will increase blood concentrations for approximately 5 h. A study of men and women aged 60–71 in China found that, compared to placebo, a single 3 mg dose of melatonin significantly impaired balance 1 h after ingestion; however, it did not significantly affect cognitive function [49][16]. A long-term, placebo-controlled study in postmenopausal women found no increase in adverse events, daytime drowsiness, muscle weakness, or impaired balance the day after taking 1–3 mg of immediate-release melatonin; however, higher doses (over 3 mg) of controlled-release melatonin products can potentially cause next-day drowsiness. A study by Gooneratne et al. demonstrated high blood levels of melatonin for an average of 10 h following ingestion of a 4 mg product (3 mg controlled-release + 1 mg immediate-release) compared to 6.4 h following a 0.4 mg product (0.3 mg controlled-release + 0.1 mg immediate-release) [50][17]. For these reasons, caution has been advised when driving or operating heavy machinery within 6 h after taking melatonin, especially after taking controlled-release products.
8. Worsening of Restless Leg Syndrome
Taking melatonin may increase leg movements in restless leg syndrome (RLS). A small study of 8 subjects with severe RLS found significantly more leg movement when measured 1 h and 4.5 h after taking 3 mg of melatonin in the evening compared to no melatonin. However, the patients in the study did not report any increase in leg discomfort [51][18]. In contrast, preliminary evidence shows that melatonin may decrease periodic leg movement disorder symptoms involving involuntary leg movements while sleeping [52][19].
9. Worsening of Asthma
There has been concern that exogenous melatonin might worsen asthma. However, a small study among people with stable, mild, to moderate asthma found that taking 3 mg of melatonin at night for 1 month did not significantly affect lung function compared to placebo [53][20].
10. Worsening of Depression and Bipolar Disorder
References
- Tarocco, A.; Caroccia, N.; Morciano, G.; Wieckowski, M.R.; Ancora, G.; Garani, G.; Pinton, P. Melatonin as a master regulator of cell death and inflammation: Molecular mechanisms and clinical implications for newborn care. Cell Death Dis. 2019, 10, 317.
- Martín Giménez, V.M.; de las Heras, N.; Lahera, V.; Tresguerres, J.A.F.; Reiter, R.J.; Manucha, W. Melatonin as an Anti-Aging Therapy for Age-Related Cardiovascular and Neurodegenerative Diseases. Front. Aging Neurosci. 2022, 14, 491. Available online: https://www.frontiersin.org/articles/10.3389/fnagi.2022.888292 (accessed on 9 March 2023).
- Van Geijlswijk, I.M.; Mol, R.H.; Egberts, T.C.G.; Smits, M.G. Evaluation of sleep, puberty and mental health in children with long-term melatonin treatment for chronic idiopathic childhood sleep onset insomnia. Psychopharmacology 2011, 216, 111–120.
- How Biomarkers Help Diagnose Dementia|National Institute on Aging. Available online: https://www.nia.nih.gov/health/how-biomarkers-help-diagnose-dementia (accessed on 9 March 2023).
- Melatonin Levels in the Alzheimer’s Disease Continuum: A Systematic Review. Available online: https://www.researchgate.net/publication/349541215_Melatonin_levels_in_the_Alzheimer%27s_disease_continuum_a_systematic_review (accessed on 9 March 2023).
- Mild Cognitive Impairment (MCI)|Symptoms & Treatments|alz.org. Available online: https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/mild-cognitive-impairment (accessed on 9 March 2023).
- Neurocognitive Effects of Melatonin Treatment in Healthy Adults and Individuals with Alzheimer’s Disease and Insomnia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/33957167/ (accessed on 9 March 2023).
- Boafo, A.; Greenham, S.; Alenezi, S.; Robillard, R.; Pajer, K.; Tavakoli, P.; De Koninck, J. Could long-term administration of melatonin to prepubertal children affect timing of puberty? A clinician’s perspective. Nat. Sci. Sleep 2019, 11, 1–10.
- Zwart, T.C.; Smits, M.G.; Egberts, T.C.; Rademaker, C.M.A.; van Geijlswijk, I.M. Long-Term Melatonin Therapy for Adolescents and Young Adults with Chronic Sleep Onset Insomnia and Late Melatonin Onset: Evaluation of Sleep Quality, Chronotype, and Lifestyle Factors Compared to Age-Related Randomly Selected Population Cohorts. Healthcare 2018, 6, 23.
- Carr, R.; Wasdell, M.B.; Hamilton, D.; Weiss, M.D.; Freeman, R.D.; Tai, J.; Rietveld, W.J.; Jan, J.E. Long-term effectiveness outcome of melatonin therapy in children with treatment-resistant circadian rhythm sleep disorders. J. Pineal Res. 2007, 43, 351–359.
- Sheldon, S.H. Pro-convulsant effects of oral melatonin in neurologically disabled children. Lancet 1998, 351, 1254.
- Wasdell, M.B.; Jan, J.E.; Bomben, M.M.; Freeman, R.D.; Rietveld, W.J.; Tai, J.; Hamilton, D.; Weiss, M.D. A randomized, placebo-controlled trial of controlled release melatonin treatment of delayed sleep phase syndrome and impaired sleep maintenance in children with neurodevelopmental disabilities. J. Pineal Res. 2008, 44, 57–64.
- Melatonin Effect on Seizures in Children with Severe Neurologic Deficit Disorders—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/11580772/ (accessed on 9 March 2023).
- Maghbooli, M.; Alyan NajafAbadi, S.; MalekMahmoudi, G.; Molseghi, M.H. Effect of add-on melatonin on seizure outcomes and quality of sleep in epilepsy with idiopathic generalized tonic-clonic seizures alone in adult patients: Cross-sectional, randomized, double-blind, placebo-controlled clinical trial. Brain Behav. 2023, 13, e2860.
- Frisher, M.; Gibbons, N.; Bashford, J.; Chapman, S.; Weich, S. Melatonin, hypnotics and their association with fracture: A matched cohort study. Age Ageing 2016, 45, 801–806.
- Lui, M.F.G.; Chow, H.K.D.; Wong, W.M.K.; Tsang, W.N.W. Melatonin Affects Postural Control in Community-Dwelling Older Adults While Dual Tasking: A Randomized Observation Study. J. Aging Phys. Act. 2019, 27, 102–107.
- Gooneratne, N.S.; Edwards, A.Y.Z.; Zhou, C.; Cuellar, N.; Grandner, M.A.; Barrett, J.S. Melatonin pharmacokinetics following two different oral surge-sustained release doses in older adults. J. Pineal Res. 2012, 52, 437–445.
- Whittom, S.; Dumont, M.; Petit, D.; Desautels, A.; Adam, B.; Lavigne, G.; Montplaisir, J. Effects of melatonin and bright light administration on motor and sensory symptoms of RLS. Sleep Med. 2010, 11, 351–355.
- Aurora, R.N.; Kristo, D.A.; Bista, S.R.; Rowley, J.A.; Zak, R.; Casey, K.; Lamm, C.I.; Tracy, S.; Rosenberg, R.S. The treatment of restless legs syndrome and periodic limb movement disorder in adult—An update for 2012: Practice parameters with an evidence-based systematic review and meta-analyses: An American Academy of Sleep Medicine Clinical Practice Guideline. Sleep 2012, 35, 1039–1062.
- Campos, F.L.; da Silva-Júnior, F.P.; de Bruin, V.M.S.; de Bruin, P.F.C. Melatonin improves sleep in asthma: A randomized, double-blind, placebo-controlled study. Am. J. Respir. Crit. Care Med. 2004, 170, 947–951.
- Carman, J.S.; Post, R.M.; Buswell, R.; Goodwin, F.K. Negative effects of melatonin on depression. Am. J. Psychiatry 1976, 133, 1181–1186.
- Hansen, M.; Danielsen, A.; Hageman, I.; Rosenberg, J.; Gögenur, I. The therapeutic or prophylactic effect of exogenous melatonin against depression and depressive symptoms: A systematic review and meta-analysis. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2014, 24, 1719–1728.
More
