Lynch syndrome (LS) is a genetic condition predisposing to a variety of tumors, including endometrial (EC) and ovarian cancers (OC), with cancer lifetime risk depending on the specific LS-mutation involved. Universal Screening is the standard for LS detection. Prophylactic surgery is a risk-reducing option that may be considered, and the age at hysterectomy and recommendation for bilateral oophorectomy depend on the mutated variant and offspring desire. Besides surgery, chemoprevention via contraceptives combination or progestin-alone is a viable option, and vaccination with tumor-specific antigens has shown promising results in mouse models.
- endometrial cancer
- ovarian cancer
- lynch syndrome
- mismatch repair deficiency
- immunohistochemistry markers
- microsatellite instability
1. Introduction
2. Lynch Syndrome-Associated Gynecologic Tumors
2.1. Lynch Syndrome-Associated Endometrial Cancer
Endometrial cancer is the second most common malignancy of the female genital tract worldwide, and it is the first most common gynecologic tumor in Western countries, with globally increasing incidence and mortality [15][16]. The most common risk factors for endometrial neoplasia include unopposed hyperestrogenism conditions (associated with diabetes, obesity, early age at menarche and late age at menopause, nulliparity, high postmenopausal estrogen concentrations), older age, history of breast cancer, and long-term use of tamoxifen [17]. However, approximately 5% of endometrial neoplasms are associated with a genetic predisposition, and 2–3% of all ECs are caused by a germline mutation in one of the MMR genes (MLH1, PMS2, MSH2 and MSH6) [18][19]. However, the incidence in selected populations at higher risk for LS (based on family, personal, and pathologic criteria), evaluated by NGS, has been reported to be approximately 13% [20]. LS-related EC is typically characterized by an endometrioid histotype, lower uterine involvement, peritumoral and tumor infiltrating lymphocytes (≥40 TIL/10HPFs), with more CD8+, CD45RO+, and PD1+ T cells at the invasive margin compared to sporadic MMRd EC, morpho-phenotypic heterogeneity, higher pathologic grade or undifferentiated forms, frequent lymphovascular invasion, deeper myometrial invasion, in particular with a typical MELF pattern [21], frequent association with synchronous ovarian cancer, early age at diagnosis (45–55 years), and lower body mass index [22]. In general, the MMRd group represents the 20–30% of all ECs and is considered a molecular subset with a good-to-intermediate prognosis, regardless of the histotype [23]. Among MMRd patients, approximately 10–30% of ECs were observed to be associated with a germline variant [18][24]. More specifically, methylated MMRd ECs seem to have a worse prognosis compared to mutated MMRd ECs, allowing a substratification of the MMRd/MSI group [25]. However, although histopathologic features can significantly improve the efficacy of MMRd/MSI detection and the identification of those sentinel cases highly suspicious for LS, other authors have demonstrated that 58% of LS-related ECs do not exhibit the classically described morphologic MSI tumor features [26]. Therefore, the use of Universal Screening to support a morphologic suspicion of LS has recently been recommended in the latest NCCN guidelines [13].2.2. Lynch Syndrome-Associated Ovarian Cancer
Ovarian cancer is the second most common gynecologic tumor in developed countries, with an incidence of more than 19,000 new cases in the United States and a higher mortality rate compared to EC [15]. More than one-fifth of ovarian tumors are caused by a hereditary susceptibility, and in approximately 65–85% of these cases, the genetic abnormality is a germline mutation in the BRCA genes. However, several other suppressor genes and oncogenes have been associated with hereditary OC, and LS is estimated to be the cause of 10–15% of hereditary OC [19]. Approximately 80% of LS-related OCs are diagnosed at stage I or II, mostly non-serous, with most of them presenting with endometrioid histology, with improved survival rates [27].3. Universal Screening
The evaluation of MMRd and/or MSI in EC has been shown to be relevant for LS screening, histo-molecular diagnosis, prognostic risk stratification, and as a predictive biomarker of response to immunotherapy [24]. Prior to the introduction of Universal Screening, the diagnostic management of LS was mainly based on Selective Screening, which included clinical criteria based on the evaluation of family and personal history and the clinicopathological features of the tumor (Amsterdam criteria 1990 [28][29], Bethesda criteria 1997 [30], and Society of Gynecologic Oncology 20–25% and 5–10% criteria 2007 [31]). However, these have been limited in their application to clinical practice due to their complexity and the frequent lack of complete family history data. In particular, Ryan et al. reported that these criteria were only able to identify the 36% (Amsterdam criteria 1990), 58% (Bethesda criteria 1997), 71% (Society of Gynecologic Oncology 20–25% criteria), and 93% (Society of Gynecologic Oncology 5–10% criteria) of patients who required further LS testing [32]. Selective Screening has traditionally been applied only to a selected population of EC or CRC patients at higher risk of being LS carriers based on family and/or personal history and pathologic features suspicious for MSI [33]. In contrast, Universal Screening has been applied to all newly diagnosed EC and CRC cases; with studies comparing the two screening approaches showing a greater sensitivity of Universal Screening in detecting patients with LS [34]. Therefore, a Universal Screening for LS diagnosis by the identification of MMRd in the tumor tissue of all newly diagnosed CRC and EC cases has recently been proposed [35][36][37]. The first step of Universal Screening is performed by IHC, a technique capable of evaluating the somatic loss of expression of the four proteins (MLH1, MSH2, MSH6, and PMS2) encoded by the MMR genes on a tumor sample. The flowchart for the identification of LS cases through Universal Screening is represented in Figure 1. Although, in some instances, a pathologist may encounter various analytical problems or diagnostic pitfalls, IHC is considered the standard, because it is more cost effective, has a shorter turnaround time, and is widely available. IHC can correlate with morphology and provide useful information about which of the four proteins is missing, thus guiding genetic testing. In addition, IHC is considered superior to MSI evaluation as a first-line testing strategy, due to the high frequency of microsatellite stable (MSS) ECs harboring mutations in MSH6, which can only be detected by the IHC approach in some cases [38][39]. Finally, considering the high frequency of MMRd and MSI observed in the peritumoral endometrial background in LS-EC patients, the IHC evaluation of MMR protein expression in the benign endometrium could be further explored as a possible integrative test to the LS screening algorithm [40]. As mentioned previously, the loss of MMR protein expression, which occurs in approximately 20–30% of patients with EC [18], requires further evaluation, and genetic counseling is always particularly recommended. About 10–30% of MMRd/MSI ECs have been observed to be associated with a germline variant [18][24], and the loss of expression of the protein encoded by the MLH1 gene represents the majority of all MMRd cases. Most of these patients do not have a germline mutation, but a loss of expression is due to somatic biallelic hypermethylation of the MLH1 promoter, as reported for CRC [41], to somatic biallelic MMR gene mutations, or to a somatic mutation associated with a loss of heterozygosity (LOH) of the other allele; alternatively, it is due to a secondary epigenetic silencing of MSH6 after neoadjuvant radio-chemotherapy treatments. In EC cases characterized by defective MLH1 expression, a somatic ‘reflex test’ is required to assess the MLH1 promoter methylation status. In contrast, the loss of expression of any of the proteins encoded by the MSH2, MSH6, or PMS2 genes, and the absence of MLH1 hypermethylation always requires a germline evaluation by NGS.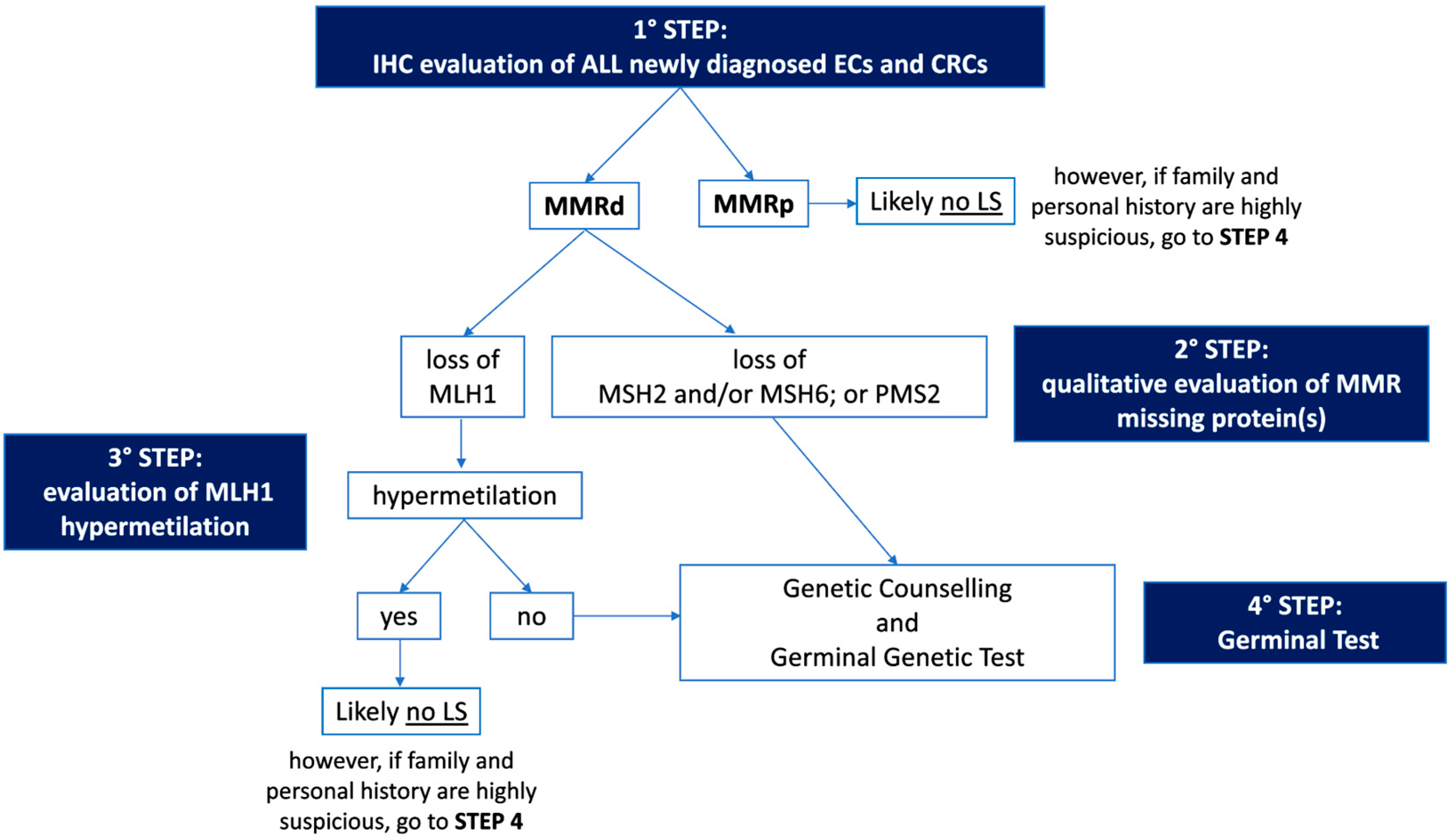
4. Prevention of Lynch Syndrome-Associated Gynecologic Tumors
4.1. Surveillance and Surgical Prophylaxis
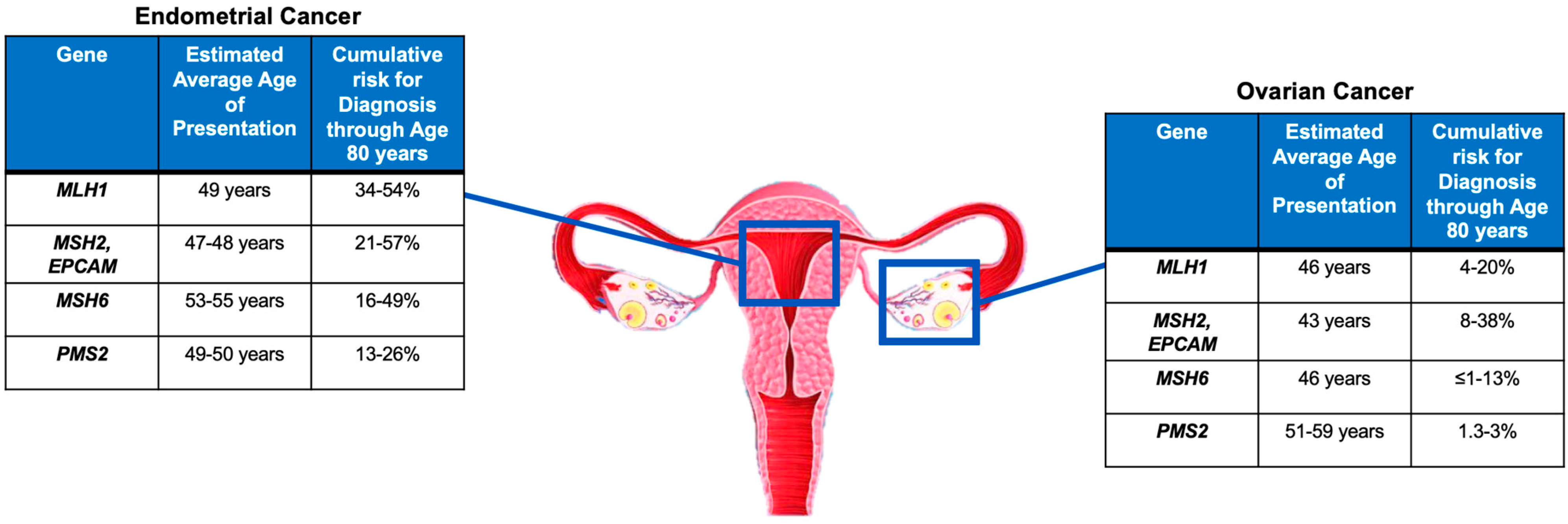
As mentioned in the previous sections, women with LS have a 19–71% and 3–14% lifetime risk of developing endometrial cancer (EC) and ovarian cancer (OC), respectively, depending on the specific mismatch repair gene mutated [6][7][8][9][10][11]. The gene-specific cancer risk for EC and OC and the average age at diagnosis are summarized in Figure 2. Large retrospective population studies have reported a cumulative risk of developing EC by the age of 70 years in patients with LS to be approximately 34–54% for MLH1mut, 21–57% for MSH2mut, 16–49% for MSH6mut, and 24% for PMS2mut [42][43]. Similar results were confirmed also in a large prospective multicenter study [5]. There is less evidence in the literature for LS-associated OC compared to the more commonly found LS-associated EC. Engel et al. found similar cumulative odds of lifetime OC diagnosis for MSH2mut and MSH6mut and a reduced risk for MLH1mut [44]. Similarly, previous data reported that MSH2mut had almost twice the OC incidence rate observed for MLH1mut [45][46]. Specifically, the cumulative risk of developing OC by the age of 70 years was reported to be 4–20% for MLH1mut, 8–38% for MSH2mut, <1–13% for MSH6mut, and, similarly to the overall population, 1.3–3% for PMS2mut [5][42][43]. The ESGO-ESTRO-ESP 2021 consensus recommends surveillance for EC in LS pa- tients starting at the age of 35 years by annual transvaginal ultrasound (TVUS) and annual or biennial endometrial biopsy; and prophylactic hysterectomy and bilateral salpingo- oophorectomy should be considered to prevent both EC and OC at the end of the childbear- ing age and preferably before the age of 40 years. In addition, estrogen replacement therapy should be recommended in premenopausal women undergoing prophylactic surgery with hysterectomy and bilateral salpingo-oophorectomy.The ESGO-ESTRO-ESP 2021 consensus recommends surveillance for EC in LS pa- tients starting at the age of 35 years by annual transvaginal ultrasound (TVUS) and annual or biennial endometrial biopsy; and prophylactic hysterectomy and bilateral salpingo- oophorectomy should be considered to prevent both EC and OC at the end of the childbear- ing age and preferably before the age of 40 years. In addition, estrogen replacement therapy should be recommended in premenopausal women undergoing prophylactic surgery with hysterectomy and bilateral salpingo-oophorectomy.
More recently, the NCCN 2022 guidelines have outlined a series of recommenda- tions for the preventive management of LS-related tumors based on the specific mutational pattern carried. Specifically, surveillance by endometrial biopsy should be performed annu- ally or biennially beginning at the age of 30–35 years; in addition, TVUS in postmenopausal women, although not considered sufficiently sensitive or specific, may be performed for screening at the clinician’s discretion in MLH1mut, MSH2mut, MSH6mut, and PMS2mut. Serum CA125 is an additional ovarian marker that could be incorporated into OC screening in any mutation status. Moreover, any abnormal uterine bleeding or postmenopausal bleed- ing, pelvic or abdominal pain, bloating, increased abdominal circumference, and any other abnormal and newly onset sign or symptom should be reported promptly to a clinician in any mutation-carrier patient. Regarding prophylactic surgery, a total hysterectomy and bilateral salpingo-oophorectomy are recommended in MLH1mut and MSH2mut to reduce the risk of both EC and OC. In these cases, the timing of surgery should be individualized based on whether childbearing is complete, comorbidities, family history, and LS gene. In MSH6mut and PMS2mut, a total hysterectomy should be recommended to reduce EC risk after completion of the reproductive desire; however, evidence is lacking to make a specific recommendation for risk-reducing salpingo-oophorectomy, and in particular the PMS2 pathogenic variant appears to have no greater than average risk for OC and may consider postponing surveillance and may reasonably elect not to have oophorectomy. Therefore, for both MSH6mut and PMS2mut, the decision on whether undergo bilateral salpingo- oophorectomy should be discussed with the patient and individualized accordingly.

4.2. Chemoprevention
4.3. Vaccination
5. Management of Patients with LS-Associated Gynecologic Cancers
5.1. Surgery and Conservative Treatment Management
5.2. Systemic Treatment
References
- Win, A.K.; Jenkins, M.A.; Dowty, J.G.; Antoniou, A.C.; Lee, A.; Giles, G.G.; Buchanan, D.D.; Clendenning, M.; Rosty, C.; Ahnen, D.J.; et al. Prevalence and Penetrance of Major Genes and Polygenes for Colorectal Cancer. Cancer Epidemiol. Biomark. Prev. 2017, 26, 404–412.
- Stoffel, E.; Mukherjee, B.; Raymond, V.M.; Tayob, N.; Kastrinos, F.; Sparr, J.; Wang, F.; Bandipalliam, P.; Syngal, S.; Gruber, S.B. Calculation of risk of colorectal and endometrial cancer among patients with Lynch syndrome. Gastroenterology 2009, 137, 1621–1627.
- Lynch, H.T.; Snyder, C.L.; Shaw, T.G.; Heinen, C.D.; Hitchins, M.P. Milestones of Lynch syndrome: 1895–2015. Nat. Rev. Cancer 2015, 15, 181–194.
- Jenkins, M.A.; Baglietto, L.; Dowty, J.G.; Van Vliet, C.M.; Smith, L.; Mead, L.J.; Macrae, F.A.; St. John, D.J.; Jass, J.R.; Giles, G.G.; et al. Cancer risks for mismatch repair gene mutation carriers: A population-based early onset case-family study. Clin. Gastroenterol. Hepatol. 2006, 4, 489–498.
- Møller, P.; Seppälä, T.T.; Bernstein, I.; Holinski-Feder, E.; Sala, P.; Gareth Evans, D.; Lindblom, A.; Macrae, F.; Blanco, I.; Sijmons, R.H.; et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: A report from the Prospective Lynch Syndrome Database. Gut 2018, 67, 1306–1316.
- Lin, K.M.; Shashidharan, M.; Thorson, A.G.; Ternent, C.A.; Blatchford, G.J.; Christensen, M.A.; Watson, P.; Lemon, S.J.; Franklin, B.; Karr, B.; et al. Cumulative incidence of colorectal and extracolonic cancers in MLH1 and MSH2 mutation carriers of hereditary nonpolyposis colorectal cancer. J. Gastrointest. Surg. 1998, 2, 67–71.
- Hendriks, Y.M.; Wagner, A.; Morreau, H.; Menko, F.; Stormorken, A.; Quehenberger, F.; Sandkuijl, L.; Møller, P.; Genuardi, M.; Van Houwelingen, H.; et al. Cancer risk in hereditary nonpolyposis colorectal cancer due to MSH6 mutations: Impact on counseling and surveillance. Gastroenterology 2004, 127, 17–25.
- Vasen, H.F.; Stormorken, A.; Menko, F.H.; Nagengast, F.M.; Kleibeuker, J.H.; Griffioen, G.; Taal, B.G.; Moller, P.; Wijnen, J.T. MSH2 mutation carriers are at higher risk of cancer than MLH1 mutation carriers: A study of hereditary nonpolyposis colorectal cancer families. J. Clin. Oncol. 2001, 19, 4074–4080.
- Barrow, E.; Robinson, L.; Alduaij, W.; Shenton, A.; Clancy, T.; Lalloo, F.; Hill, J.; Evans, D.G. Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: A report of 121 families with proven mutations. Clin. Genet. 2009, 75, 141–149.
- Vasen, H.F.; Morreau, H.; Nortier, J.W. Is breast cancer part of the tumor spectrum of hereditary nonpolyposis colorectal cancer? Am. J. Hum. Genet. 2001, 68, 1533–1535.
- Hampel, H.; Stephens, J.A.; Pukkala, E.; Sankila, R.; Aaltonen, L.A.; Mecklin, J.P.; de la Chapelle, A. Cancer risk in hereditary nonpolyposis colorectal cancer syndrome: Later age of onset. Gastroenterology 2005, 129, 415–421.
- Yurgelun, M.B.; Hampel, H. Recent Advances in Lynch Syndrome: Diagnosis, Treatment, and Cancer Prevention. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 101–109.
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Genetic/Familial High-Risk Assessment: Colorectal Version 1.2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf (accessed on 10 February 2023).
- Llach, J.; Pellisé, M.; Monahan, K. Lynch syndrome; towards more personalized management? Best Pract. Res. Clin. Gastroenterol. 2022, 58–59, 101790.
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33.
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249.
- Amant, F.; Moerman, P.; Neven, P.; Timmerman, D.; Van Limbergen, E.; Vergote, I. Endometrial cancer. Lancet 2005, 366, 491–505.
- Ryan, N.A.J.; Glaire, M.A.; Blake, D.; Cabrera-Dandy, M.; Evans, D.G.; Crosbie, E.J. The proportion of endometrial cancers associated with Lynch syndrome: A systematic review of the literature and meta-analysis. Genet. Med. 2019, 21, 2167–2180.
- Daniels, M.S.; Lu, K.H. Genetic predisposition in gynecologic cancers. Semin. Oncol. 2016, 43, 543–547.
- Kim, Y.N.; Kim, M.K.; Lee, Y.J.; Lee, Y.; Sohn, J.Y.; Lee, J.Y.; Choi, M.C.; Kim, M.; Jung, S.G.; Joo, W.D.; et al. Identification of Lynch Syndrome in Patients with Endometrial Cancer Based on a Germline Next Generation Sequencing Multigene Panel Test. Cancers 2022, 14, 3406.
- Santoro, A.; Angelico, G.; Inzani, F.; Spadola, S.; Arciuolo, D.; Valente, M.; Musarra, T.; Capelli, G.; Fanfani, F.; Gallotta, V.; et al. Pathological features, immunoprofile and mismatch repair protein expression status in uterine endometrioid carcinoma: Focus on MELF pattern of myoinvasion. Eur. J. Surg. Oncol. 2021, 47, 338–345.
- Zhao, S.; Chen, L.; Zang, Y.; Liu, W.; Liu, S.; Teng, F.; Xue, F.; Wang, Y. Endometrial cancer in Lynch syndrome. Int. J. Cancer 2022, 150, 7–17.
- Kommoss, S.; McConechy, M.K.; Kommoss, F.; Leung, S.; Bunz, A.; Magrill, J.; Britton, H.; Kommoss, F.; Grevenkamp, F.; Karnezis, A.; et al. Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann. Oncol. 2018, 29, 1180–1188.
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int. J. Gynecol. Cancer 2021, 31, 12–39.
- Pasanen, A.; Loukovaara, M.; Bützow, R. Clinicopathological significance of deficient DNA mismatch repair and MLH1 promoter methylation in endometrioid endometrial carcinoma. Mod. Pathol. 2020, 33, 1443–1452.
- Mills, A.M.; Liou, S.; Ford, J.M.; Berek, J.S.; Pai, R.K.; Longacre, T.A. Lynch syndrome screening should be considered for all patients with newly diagnosed endometrial cancer. Am. J. Surg. Pathol. 2014, 38, 1501–1509.
- Nakamura, K.; Banno, K.; Yanokura, M.; Iida, M.; Adachi, M.; Masuda, K.; Ueki, A.; Kobayashi, Y.; Nomura, H.; Hirasawa, A.; et al. Features of ovarian cancer in Lynch syndrome (Review). Mol. Clin. Oncol. 2014, 2, 909–916.
- Vasen, H.F.; Mecklin, J.P.; Khan, P.M.; Lynch, H.T. The International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC). Dis. Colon Rectum 1991, 34, 424–425.
- Vasen, H.F.; Watson, P.; Mecklin, J.P.; Lynch, H.T. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology 1999, 116, 1453–1456.
- Rodriguez-Bigas, M.A.; Boland, C.R.; Hamilton, S.R.; Henson, D.E.; Jass, J.R.; Khan, P.M.; Lynch, H.; Perucho, M.; Smyrk, T.; Sobin, L.; et al. A National Cancer Institute Workshop on Hereditary Nonpolyposis Colorectal Cancer Syndrome: Meeting highlights and Bethesda guidelines. J. Nat. Cancer Inst. 1997, 89, 1758–1762.
- Lancaster, J.M.; Powell, C.B.; Kauff, N.D.; Cass, I.; Chen, L.M.; Lu, K.H.; Mutch, D.G.; Berchuck, A.; Karlan, B.Y.; Herzog, T.J. Society of Gynecologic Oncologists Education Committee statement on risk assessment for inherited gynecologic cancer predispositions. Gynecol. Oncol. 2007, 107, 159–162.
- Ryan, P.; Mulligan, A.M.; Aronson, M.; Ferguson, S.E.; Bapat, B.; Semotiuk, K.; Holter, S.; Kwon, J.; Kalloger, S.E.; Gilks, C.B.; et al. Comparison of clinical schemas and morphologic features in predicting Lynch syndrome in mutation-positive patients with endometrial cancer encountered in the context of familial gastrointestinal cancer registries. Cancer 2012, 118, 681–688.
- Kidambi, T.D.; Blanco, A.; Myers, M.; Conrad, P.; Loranger, K.; Terdiman, J.P. Selective Versus Universal Screening for Lynch Syndrome: A Six-Year Clinical Experience. Dig. Dis. Sci. 2015, 60, 2463–2469.
- Moreira, L.; Balaguer, F.; Lindor, N.; de la Chapelle, A.; Hampel, H.; Aaltonen, L.A.; Hopper, J.L.; Le Marchand, L.; Gallinger, S.; Newcomb, P.A.; et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA 2012, 308, 1555–1565.
- Carnevali, I.; Sahnane, N.; Chiaravalli, A.M.; Di Lauro, E.; Facco, C.; Facchi, S.; Casarin, J.; Ghezzi, F.; Sessa, F.; Tibiletti, M.G. Strategies for Lynch syndrome identification in selected and unselected gynecological cancers. Eur. J. Cancer Prev. 2022, 31, 369–376.
- Crosbie, E.J.; Ryan, N.A.J.; Arends, M.J.; Bosse, T.; Burn, J.; Cornes, J.M.; Crawford, R.; Eccles, D.; Frayling, I.M.; Ghaem-Maghami, S.; et al. The Manchester International Consensus Group recommendations for the management of gynecological cancers in Lynch syndrome. Genet. Med. 2019, 21, 2390–2400.
- Mange, S.; Bellcross, C.; Cragun, D.; Duquette, D.; Gorman, L.; Hampel, H.; Jasperson, K. Creation of a network to promote universal screening for Lynch syndrome: The LynchSyndrome Screening Network. J. Genet. Couns. 2015, 24, 421–427.
- Dedeurwaerdere, F.; Claes, K.B.; Van Dorpe, J.; Rottiers, I.; Van der Meulen, J.; Breyne, J.; Swaerts, K.; Martens, G. Comparison of microsatellite instability detection by immunohistochemistry and molecular techniques in colorectal and endometrial cancer. Sci. Rep. 2021, 11, 12880.
- Zannoni, G.F.; Bragantini, E.; Castiglione, F.; Fassan, M.; Troncone, G.; Inzani, F.; Pesci, A.; Santoro, A.; Fraggetta, F. Current Prognostic and Predictive Biomarkers for Endometrial Cancer in Clinical Practice: Recommendations/Proposal from the Italian Study Group. Front. Oncol. 2022, 12, 805613.
- Hegazy, S.; Brand, R.E.; Dudley, B.; Karloski, E.; Bhargava, R.; Elishaev, E.; Pai, R.K. DNA mismatch repair-deficient non-neoplastic endometrial glands are common in Lynch syndrome patients and are present at a higher density than in the colon. Histopathology 2021, 79, 573–583.
- Hampel, H.; Frankel, W.L.; Martin, E.; Arnold, M.; Khanduja, K.; Kuebler, P.; Clendenning, M.; Sotamaa, K.; Prior, T.; Westman, J.A.; et al. Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J. Clin. Oncol. 2008, 26, 5783–5788.
- Bonadona, V.; Bonaïti, B.; Olschwang, S.; Grandjouan, S.; Huiart, L.; Longy, M.; Guimbaud, R.; Buecher, B.; Bignon, Y.J.; Caron, O.; et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 2011, 305, 2304–2310.
- Møller, P.; Seppälä, T.; Bernstein, I.; Holinski-Feder, E.; Sala, P.; Evans, D.G.; Lindblom, A.; Macrae, F.; Blanco, I.; Sijmons, R.; et al. Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: First report from the prospective Lynch syndrome database. Gut 2017, 66, 464–472.
- Engel, C.; Loeffler, M.; Steinke, V.; Rahner, N.; Holinski-Feder, E.; Dietmaier, W.; Schackert, H.K.; Goergens, H.; von Knebel Doeberitz, M.; Goecke, T.O.; et al. Risks of less common cancers in proven mutation carriers with lynch syndrome. J. Clin. Oncol. 2012, 30, 4409–4415.
- Watson, P.; Vasen, H.F.A.; Mecklin, J.P.; Bernstein, I.; Aarnio, M.; Järvinen, H.J.; Myrhøj, T.; Sunde, L.; Wijnen, J.T.; Lynch, H.T. The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int. J. Cancer 2008, 123, 444–449.
- Ryan, N.A.J.; Evans, D.G.; Green, K.; Crosbie, E.J. Pathological features and clinical behavior of Lynch syndrome-associated ovarian cancer. Gynecol. Oncol. 2017, 144, 491–495.
- Ryan, N.A.J.; Morris, J.; Green, K.; Lalloo, F.; Woodward, E.R.; Hill, J.; Crosbie, E.J.; Evans, D.G. Association of Mismatch Repair Mutation With Age at Cancer Onset in Lynch Syndrome: Implications for Stratified Surveillance Strategies. JAMA Oncol. 2017, 3, 1702–1706.
- Ten Broeke, S.W.; van der Klift, H.M.; Tops, C.M.J.; Aretz, S.; Bernstein, I.; Buchanan, D.D.; de la Chapelle, A.; Capella, G.; Clendenning, M.; Engel, C.; et al. Cancer Risks for PMS2-Associated Lynch Syndrome. J. Clin. Oncol. 2018, 36, 2961–2968.
- Zhang, Y.; Liu, H.; Yang, S.; Zhang, J.; Qian, L.; Chen, X. Overweight, obesity and endometrial cancer risk: Results from a systematic review and meta-analysis. Int. J. Biol. Markers 2014, 29, e21–e29.
- Dossus, L.; Allen, N.; Kaaks, R.; Bakken, K.; Lund, E.; Tjonneland, A.; Olsen, A.; Overvad, K.; Clavel-Chapelon, F.; Fournier, A.; et al. Reproductive risk factors and endometrial cancer: The European Prospective Investigation into Cancer and Nutrition. Int. J. Cancer 2010, 127, 442–451.
- Dashti, S.G.; Chau, R.; Ouakrim, D.A.; Buchanan, D.D.; Clendenning, M.; Young, J.P.; Winship, I.M.; Arnold, J.; Ahnen, D.J.; Haile, R.W.; et al. Female Hormonal Factors and the Risk of Endometrial Cancer in Lynch Syndrome. JAMA 2015, 314, 61–71.
- Allen, N.; Yang, T.O.; Olsson, H. Endometrial cancer and oral contraceptives: An individual participant meta-analysis of 27,276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol. 2015, 16, 1061–1070.
- Lu, K.H.; Loose, D.S.; Yates, M.S.; Nogueras-Gonzalez, G.M.; Munsell, M.F.; Chen, L.M.; Lynch, H.; Cornelison, T.; Boyd-Rogers, S.; Rubin, M.; et al. Prospective multicenter randomized intermediate biomarker study of oral contraceptive versus depo-provera for prevention of endometrial cancer in women with Lynch syndrome. Cancer Prev. Res. 2013, 6, 774–781.
- Drew, D.A.; Cao, Y.; Chan, A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer 2016, 16, 173–186.
- Burn, J.; Sheth, H.; Elliott, F.; Reed, L.; Macrae, F.; Mecklin, J.P.; Möslein, G.; McRonald, F.E.; Bertario, L.; Evans, D.G.; et al. Cancer prevention with aspirin in hereditary colorectal cancer (Lynch syndrome), 10-year follow-up and registry-based 20-year data in the CAPP2 study: A double-blind, randomised, placebo-controlled trial. Lancet 2020, 395, 1855–1863.
- von Knebel Doeberitz, M.; Kloor, M. Towards a vaccine to prevent cancer in Lynch syndrome patients. Fam. Cancer 2013, 12, 307–312.
- Kloor, M.; von Knebel Doeberitz, M. The Immune Biology of Microsatellite-Unstable Cancer. Trends Cancer 2016, 2, 121–133.
- Roudko, V.; Bozkus, C.C.; Orfanelli, T.; McClain, C.B.; Carr, C.; O’Donnell, T.; Chakraborty, L.; Samstein, R.; Huang, K.L.; Blank, S.V.; et al. Shared Immunogenic Poly-Epitope Frameshift Mutations in Microsatellite Unstable Tumors. Cell 2020, 183, 1634–1649.e1617.
- Roudko, V.; Cimen Bozkus, C.; Greenbaum, B.; Lucas, A.; Samstein, R.; Bhardwaj, N. Lynch Syndrome and MSI-H Cancers: From Mechanisms to “Off-The-Shelf” Cancer Vaccines. Front. Immunol. 2021, 12, 757804.
- Gebert, J.; Gelincik, O.; Oezcan-Wahlbrink, M.; Marshall, J.D.; Hernandez-Sanchez, A.; Urban, K.; Long, M.; Cortes, E.; Tosti, E.; Katzenmaier, E.M.; et al. Recurrent Frameshift Neoantigen Vaccine Elicits Protective Immunity With Reduced Tumor Burden and Improved Overall Survival in a Lynch Syndrome Mouse Model. Gastroenterology 2021, 161, 1288–1302.e1213.
- National Comprehensive Cancer Network. Uterine Neoplasms (Version 1.2022). Available online: https://www.nccn.org/guidelines/guidelinesdetail?category=1&id=1473 (accessed on 10 February 2023).
- Westin, S.N.; Fellman, B.; Sun, C.C.; Broaddus, R.R.; Woodall, M.L.; Pal, N.; Urbauer, D.L.; Ramondetta, L.M.; Schmeler, K.M.; Soliman, P.T.; et al. Prospective phase II trial of levonorgestrel intrauterine device: Nonsurgical approach for complex atypical hyperplasia and early-stage endometrial cancer. Am. J. Obstet. Gynecol. 2021, 224, e191.
- Marabelle, A.; Le, D.T.; Ascierto, P.A.; Di Giacomo, A.M.; De Jesus-Acosta, A.; Delord, J.P.; Geva, R.; Gottfried, M.; Penel, N.; Hansen, A.R.; et al. Efficacy of Pembrolizumab in Patients With Noncolorectal High Microsatellite Instability/Mismatch Repair-Deficient Cancer: Results From the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020, 38, 1–10.
- Mittica, G.; Ghisoni, E.; Giannone, G.; Aglietta, M.; Genta, S.; Valabrega, G. Checkpoint inhibitors in endometrial cancer: Preclinical rationale and clinical activity. Oncotarget 2017, 8, 90532–90544.
- Maio, M.; Ascierto, P.A.; Manzyuk, L.; Motola-Kuba, D.; Penel, N.; Cassier, P.A.; Bariani, G.M.; De Jesus Acosta, A.; Doi, T.; Longo, F.; et al. Pembrolizumab in microsatellite instability high or mismatch repair deficient cancers: Updated analysis from the phase II KEYNOTE-158 study. Ann. Oncol. 2022, 33, 929–938.
- Bellone, S.; Roque, D.M.; Siegel, E.R.; Buza, N.; Hui, P.; Bonazzoli, E.; Guglielmi, A.; Zammataro, L.; Nagarkatti, N.; Zaidi, S.; et al. A phase 2 evaluation of pembrolizumab for recurrent Lynch-like versus sporadic endometrial cancers with microsatellite instability. Cancer 2022, 128, 1206–1218.
- Bellone, S.; Roque, D.M.; Siegel, E.R.; Buza, N.; Hui, P.; Bonazzoli, E.; Guglielmi, A.; Zammataro, L.; Nagarkatti, N.; Zaidi, S.; et al. A phase II evaluation of pembrolizumab in recurrent microsatellite instability-high (MSI-H) endometrial cancer patients with Lynch-like versus MLH-1 methylated characteristics (NCT02899793). Ann. Oncol. 2021, 32, 1045–1046.
- Makker, V.; Colombo, N.; Casado Herráez, A.; Santin, A.D.; Colomba, E.; Miller, D.S.; Fujiwara, K.; Pignata, S.; Baron-Hay, S.; Ray-Coquard, I.; et al. Lenvatinib plus Pembrolizumab for Advanced Endometrial Cancer. N. Engl. J. Med. 2022, 386, 437–448.
- Oaknin, A.; Gilbert, L.; Tinker, A.V.; Brown, J.; Mathews, C.; Press, J.; Sabatier, R.; O’Malley, D.M.; Samouelian, V.; Boni, V.; et al. Safety and antitumor activity of dostarlimab in patients with advanced or recurrent DNA mismatch repair deficient/microsatellite instability-high (dMMR/MSI-H) or proficient/stable (MMRp/MSS) endometrial cancer: Interim results from GARNET-a phase I, single-arm study. J. Immunother. Cancer 2022, 10, e003777.
- Renner, N.; Robertson, J.; Welch, S.; Tinker, A.V.; Elit, L.; Ghatage, P.; Samouëlian, V.; Gilbert, L.; Spratlin, J.; Ellard, S.; et al. Post Hoc Analysis of Objective Response Rate by Mismatch Repair Protein Dimer Loss/Mutation Status in Patients with Mismatch Repair Deficient Endometrial Cancer Treated with Dostarlimab. In Proceedings of the European Society of Gynaecological Oncology (ESGO) 2022, Berlin, Germany, 27–30 October 2022.
