Online adaptive radiation is a new and exciting modality of treatment for gynecologic cancers. Traditional radiation treatments deliver the same radiation plan to cancers with large margins. Improvements in imaging, technology, and artificial intelligence have made it possible to account for changes between treatments and improve the delivery of radiation. These advances can potentially lead to significant benefits in tumor coverage and normal tissue sparing. Gynecologic cancers can uniquely benefit from this technology due to the significant changes in bladder, bowel, and rectum between treatments as well as the changes in tumors commonly seen between treatments. Preliminary studies have shown that online adaptive radiation can maintain coverage of the tumor while sparing nearby organs.
- gynecologic cancer
- online adaptive radiotherapy
- radiation oncology
1. Introduction
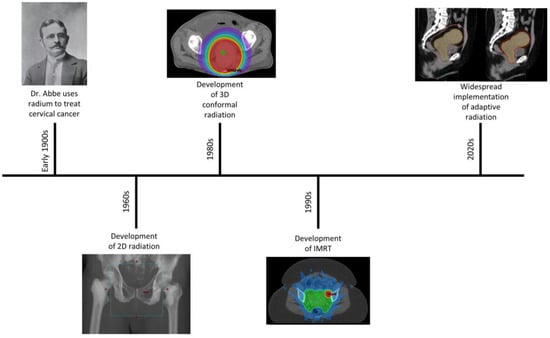
2. History of Radiotherapy for GYN Cancers
3. Adaptive Radiation Introduction
4. Logistics of Adaptive Radiation
The online ART workflow starts with on-board imaging aimed to obtain the anatomical/functional information on the day of treatment as guidance for adaptation. CBCT and MRI are the most common imaging modalities available in commercial on-line ART treatment units [16][17]. CBCT can be acquired quickly providing anatomical and physical properties of tissue in the scanned area. MRI, on the other hand, often takes longer to scan, but can offer better tissue delineation, and potentially some functional information [18]. Furthermore, functional imaging techniques, such as PET/CT, have also been integrated as an on-board imaging option which has the potential to provide additional information to guide online ART [19].
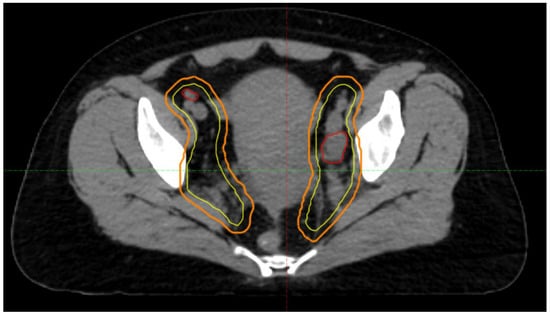
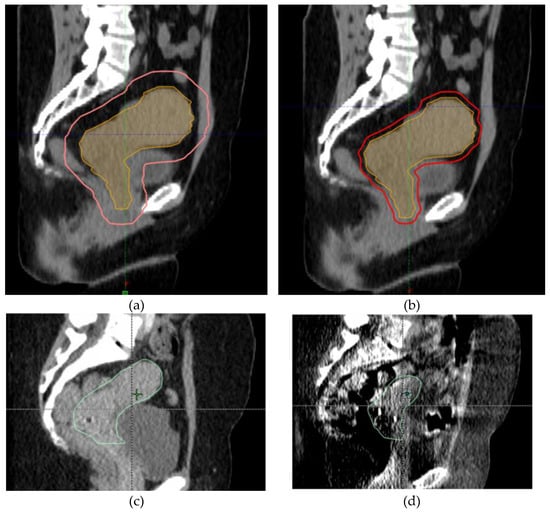
With images acquired, online contouring is performed to re-delineate treatment targets and critical organs to reflect the anatomical/functional changes of the patient at the time of treatment. Automatic contour generation is highly demanded to not only improve efficiency, but also to reduce manual efforts and potential human errors under intense time pressure. There are many approaches developed recently for automatic contour generation including artificial intelligence-based segmentation methods, which directly contour targets and OARs, and deformable registration-based methods, which propagates contours from the pre-planning stage to the images of the day. Regardless of the strategy employed for automatic contour generation, it is recommended that clinicians review and adjust contours if needed in routine clinical practice to ensure the integrity of contours.
With contours generated, online re-planning is then performed. Different commercial systems have implemented distinct plan optimization strategies to generate high-quality treatment plans efficiently.
Upon the completion of online re-planning, plan review and approval will be performed by the attending physician followed by treatment delivery. Unlike a conventional workflow, patients remain on the couch throughout the entire ART session to minimize changes in patient positioning and anatomy. After plan review and approval, computation-based quality assurance (QA) is often performed using commercial or in-house software to ensure the proper delivery of treatment.
An example for a typical workflow for a CBCT-based system during the day of treatment is as follows: the radiation therapist brings the patient into the treatment vault and positions the patient accordingly. A cone-beam CT is acquired which is then deformably registered to initial planning CT and the treating physician is then paged to the machine. Next, the physician reviews the contours and OARs and adjusts as needed. PTV expansions and other derived structures are automatically generated based on the physician’s contours. The dose is rapidly recalculated and a plan is automatically generated. The physician reviews this new plan and decides whether to treat with the new adapted plan or scheduled plan. Finally, QA is performed and the selected plan is delivered. Based on theour researcher'institution’s experience, the entire adaptive process takes ~40 minutes to treat a patient with pelvis-confined disease. The adaptive workflow is represented in Figure 4.
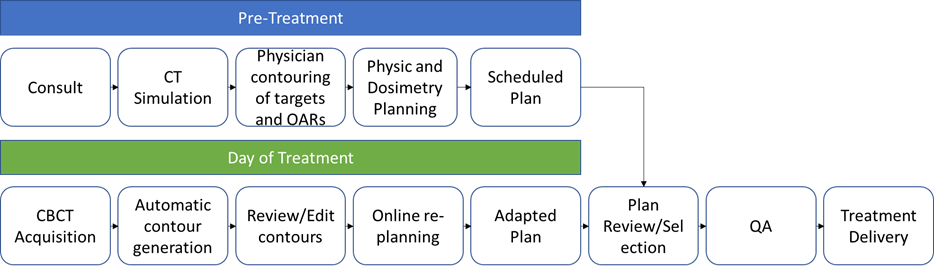
Figure 4. ART workflow. Prior to treatment, patients undergo consultation followed by CT Simulation. Physicians contour targets and OARs on the CT obtained, which is then given to a physicist/dosimetrist to create a radiation plan called the scheduled plan. On the day of treatment, patients undergo a CBCT. Contours are automatically generated and a physician reviews and edits contours as needed. A plan is generated in the TPS to create a plan called the adapted plan. The scheduled plan and adapted plan are reviewed by the physician and a plan is selected. QA is performed by the physicist and the selected treatment plan is delivered. OAR: organ-at-risk, CBCT: cone-beam CT, TPS: treatment planning system, QA: quality assurance.
With online adaptive radiation, adaptation can be scheduled in different ways including daily, weekly, or adapt-on-demand. As these names suggest, patients can undergo adaptations every day, weekly, or as needed.
The different timings of adaptive radiation can have a significant impact on clinic resources. Daily adaptive radiation requires the most resources and time while adapt-on-demand requires the least. On the other hand, more frequent adaptations can lead to improved dosimetry. This balance of improved dosimetry versus clinic resources as well as the optimal timing for adaptations is still under investigation. Potential factors that could impact the timing of adaptation include clinic resources available, location of the tumor, and the planned total dose.
Interfractional motion can be accounted for with online adaptive radiation and is one of the main benefits of online adaptive radiation for GYN cancers. However, physicians must still account for intrafractional motion. This is especially relevant for the bladder and rectum, which can lead to significant motion in the uterus and cervix. Previous reports have shown that changes in bladder filling can lead to intrafractional motion of the uterocervix of up to 10.8 mm superiorly, 1.5 mm inferiorly, 3.19 mm anteriorly, 3.43 mm posteriorly, 2.74 mm to the left, and 2.48 mm to the right [20].
A recently published study described the potential for decreasing CTV to PTV margins from 1.5 - 2.0 cm down to 5 mm for patients undergoing daily adaptive radiation [21]. In this study, with a uniform 5 mm expansion, 98.39 ± 2.97% of the end-treatment CTV was covered in a validation cohort. Importantly, these patients were treated with only daily adaptive radiation. For patients undergoing weekly or adapt-on-demand, the study recommend larger 1.0 - 1.5 cm margins to account for potential interfractional motion during non-adapted fractions.[14]
On the other hand, nodal volumes are often static and have minimal intrafractional motion. In a study by Bjoreland et al., they found that clinical nodal volumes had minimal motion in patients with prostate cancer [22].
5. Benefits and Limitations of ART for GYN Cancers
There are a number of potential benefits from online adaptive radiation. First, as described above, online adaptive radiation can potentially be used to reduce CTV to PTV margins. Based on the study described above, by reducing margins from 15 mm to 5 mm, the volume of bowel treated decreased by 292 cm3. While this has not yet been proven to have a clinical benefit, there is an ongoing clinical trial investigating this [23]. This trial is investigating the benefits of ART to quality of life and toxicity improvements, while ensuring no compromise in tumor control and patient cancer outcomes.
Additionally, preliminary studies in other pelvic cancers have shown clear benefit in target coverage and OAR sparing with online ART. One such study, looking at online ART for prostate cancers showed 13% increase in minimum prostate dose and 13% decrease in dose to the rectum [24]. Another study looked at the benefits of an online adaptive plan-of-the-day approach for cervical cancers. In their study, if patients had > 2.5 cm uterocervix motion, they had 2 plan-of-the-day plans generated. With these plans, they reported improved bowel doses by 26-29% [25].
Another potential benefit that has not been well studied is utilization of adaptive radiation in response to biologic changes [10]. This may be the greatest benefit of ART. By monitoring tumor response to treatment at a physiologic or molecular level and tailoring treatment to those responses, we may be able to better utilize radiation in the treatment of GYN cancers. There are several on-going clinical trials examining the potential of biologic response driven ART [26][27][28][29]. Based on this notion, personalized ultrafractionated stereotactic adaptive radiotherapy (PULSAR) has become a new modality for delivering radiation where fractions, referred to as pulses, are delivered weeks apart with larger doses. In preliminary studies, immunotherapy in combination with PULSAR had better tumor control compared to traditional daily fractionation [30].
ART also comes with a number of limitations. The most obvious limitation is the significant required clinical resources required for the implementation of ART. This process involves physicians, physicists, dosimetrists, and therapists. Additionally, the time required for ART is also dependent on the accuracy of AI-segmentation and auto-planning. Lastly, online ART treatment machines can require significant economic investment for not only the purchase of the machine, but additionally maintenance.
6. Future Directions
Given the potential benefits of online adaptive radiation, numerous trials have been opened to explore the potential benefits. These trials are highlighted in Table 1.
Table 1.
Ongoing clinical trials utilizing online ART
|
Clinical Trial Name |
Goal |
|
ARTIA-Cervix [23] |
Demonstrate that ART for locally advanced cervical cancer will translate into decreased GI toxicities |
|
Phase I Trial of Stereotactic MRI-Guided Online Adaptive Radiation Therapy (SMART) for the Treatment of Oligometastatic Ovarian Cancer [31] |
Assess the feasibility of stereotactic MRI-guided online adaptive radiation therapy for treatment of oligometastatic ovarian cancer |
|
Intratreatment FDG-PET During Radiation Therapy for Gynecologic and Gastrointestinal Cancers [32] |
Evaluate the utility of adaptive intratreatment PET-CT planning for gynecologic and gastrointestinal cancers |
7. Conclusion
Online ART presents the newest frontier in the treatment of gynecologic cancers. The potential benefits from online ART include improved normal tissue sparing, improved target coverage, and improved treatment in response to biologic changes. However, they come at the cost of increased demand of clinic resources. These benefits need to be proven through clinical trials that are currently ongoing and recruiting. Online ART is the next step in the personalization of cancer care and has the possibility to revolutionize the treatment of GYN cancers.
References
- Centers for Disease Control and Prevention. Gynecologic Cancer Incidence, U.S.U.D.B., no 11. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2019.
- Hellman, K., A.-C. Hellström, and B.F. Pettersson, Uterine cervix cancer treatment at Radiumhemmet: 90 years' experience. Time trends of age, stage, and histopathology distribution. Cancer Medicine, 2014. 3(2): p. 284-292.
- Erickson, B., Lim, K., Stewart, J., Donnelly, E., Small, W., Fyles, A., & Milosevic, M, Adaptive Radiation Therapy for Gynecologic Cancers., in Adaptive Radiation Therapy. 2011, CRC Press. p. 351-368.
- Williamson, C.W., et al., Advances in External Beam Radiation Therapy and Brachytherapy for Cervical Cancer. Clinical Oncology, 2021. 33(9): p. 567-578.
- Klopp, A.H., et al., Patient-Reported Toxicity During Pelvic Intensity-Modulated Radiation Therapy: NRG Oncology–RTOG 1203. Journal of Clinical Oncology, 2018. 36(24): p. 2538-2544.
- Roeske, J.C., et al., Intensity-modulated whole pelvic radiation therapy in patients with gynecologic malignancies. Int J Radiat Oncol Biol Phys, 2000. 48(5): p. 1613-21.
- Beriwal, S., et al., Intensity-modulated radiotherapy for the treatment of vulvar carcinoma: a comparative dosimetric study with early clinical outcome. Int J Radiat Oncol Biol Phys, 2006. 64(5): p. 1395-400.
- Lim, K., et al., Consensus Guidelines for Delineation of Clinical Target Volume for Intensity-Modulated Pelvic Radiotherapy for the Definitive Treatment of Cervix Cancer. International Journal of Radiation Oncology*Biology*Physics, 2011. 79(2): p. 348-355.
- Bondar, M.L., et al., Individualized nonadaptive and online-adaptive intensity-modulated radiotherapy treatment strategies for cervical cancer patients based on pretreatment acquired variable bladder filling computed tomography scans. Int J Radiat Oncol Biol Phys, 2012. 83(5): p. 1617-23.
- Glide-Hurst, C.K., et al., Adaptive Radiation Therapy (ART) Strategies and Technical Considerations: A State of the ART Review From NRG Oncology. Int J Radiat Oncol Biol Phys, 2021. 109(4): p. 1054-1075.
- Pötter, R., et al., The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Transl Radiat Oncol, 2018. 9: p. 48-60.
- Sturdza, A., et al., Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in RetroEMBRACE, a multicenter cohort study. Radiother Oncol, 2016. 120(3): p. 428-433.
- Small, W., Jr., et al., NRG Oncology/RTOG Consensus Guidelines for Delineation of Clinical Target Volume for Intensity Modulated Pelvic Radiation Therapy in Postoperative Treatment of Endometrial and Cervical Cancer: An Update. Int J Radiat Oncol Biol Phys, 2021. 109(2): p. 413-424.
- Gaffney, D.K., et al., Consensus Recommendations for Radiation Therapy Contouring and Treatment of Vulvar Carcinoma. Int J Radiat Oncol Biol Phys, 2016. 95(4): p. 1191-200.
- Gay, H.A., et al., Pelvic normal tissue contouring guidelines for radiation therapy: a Radiation Therapy Oncology Group consensus panel atlas. Int J Radiat Oncol Biol Phys, 2012. 83(3): p. e353-62.
- Varian, Ethos Therapy: An Adaptive Intelligence Solution. 2020, Varian.
- Elekta, Elekta Unity: Two worlds, one future. 2020, Elekta.
- Holdsworth, S.J. and R. Bammer, Magnetic resonance imaging techniques: fMRI, DWI, and PWI. Semin Neurol, 2008. 28(4): p. 395-406.
- Reflexion, Discover the Reflexion X1. 2021, Reflexion.
- Li, X., et al., Online MR evaluation of inter- and intra-fraction uterus motions and bladder volume changes during cervical cancer external beam radiotherapy. Radiation Oncology, 2021. 16(1): p. 179.
- Yen, A., et al., Spare the Bowel, Don't Spoil the Target: Optimal Margin Assessment for Online Cone-Beam Adaptive Radiation Therapy (OnC-ART) of the Cervix. Practical Radiation Oncology, 2022.
- Björeland, U., et al., Inter-fraction movements of the prostate and pelvic lymph nodes during IGRT. J Radiat Oncol, 2018. 7(4): p. 357-366.
- Daily Adaptive Radiation Therapy an Individualized Approach for Carcinoma of the Cervix. https://ClinicalTrials.gov/show/NCT05197881.
- Ahunbay, E.E., et al., Online adaptive replanning method for prostate radiotherapy. Int J Radiat Oncol Biol Phys, 2010. 77(5): p. 1561-72.
- Heijkoop, S.T., et al., Clinical Implementation of an Online Adaptive Plan-of-the-Day Protocol for Nonrigid Motion Management in Locally Advanced Cervical Cancer IMRT. International Journal of Radiation Oncology*Biology*Physics, 2014. 90(3): p. 673-679.
- Randomized Phase II Study of DCE-MRI-based Dose Escalation for Poor-prognosis and Neck Cancer. https://clinicaltrials.gov/ct2/show/NCT02031250.
- Individualized Adaptive De-escalated Radiotherapy for HPV-related Oropharynx Cancer. https://clinicaltrials.gov/ct2/show/NCT03416153.
- Trial of Magnetic Resonance Imaging Guided Radiotherapy Dose Adaptation in Human Papilloma Virus Positive Oropharyngeal Cancer. https://clinicaltrials.gov/ct2/show/NCT03224000.
- Adaptive Radiation Treatment for Head and Neck Cancer (ARTFORCE). https://clinicaltrials.gov/ct2/show/NCT01504815.
- Moore, C., et al., Personalized Ultrafractionated Stereotactic Adaptive Radiotherapy (PULSAR) in Preclinical Models Enhances Single-Agent Immune Checkpoint Blockade. Int J Radiat Oncol Biol Phys, 2021. 110(5): p. 1306-1316.
- Henke, L.E., et al., Phase I Trial of Stereotactic MRI-Guided Online Adaptive Radiation Therapy (SMART) for the Treatment of Oligometastatic Ovarian Cancer. Int J Radiat Oncol Biol Phys, 2022. 112(2): p. 379-389.
- Intratreatment FDG-PET During Radiation Therapy for Gynecologic and Gastrointestinal Cancers. https://clinicaltrials.gov/ct2/show/NCT03403465.
