Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Jason Zhu and Version 2 by Jason Zhu.
The most recent development in the field of automated electrocardiogram (ECG) analysis has been the use of artificial intelligence (AI), including a variety of machine learning techniques to aid interpretation. One of the authors (PWM) was involved in the use of neural networks in the early 1990s but at that time, use of a simple neural network did not prove to be of any great advantage in ECG interpretation compared to the use of more basic, straightforward diagnostic criteria. This entry describes the development of automated ECG interpretation since its beginnings in Washington DC around 1960 up until the present.
- electrocardiogram (ECG)
- automated ECG analysis
- CSE study
- age
- sex
- race
- historical aspects
1. Introduction
Augustus Waller (1856–1922) was the first person to record a single lead electrocardiogram (ECG), which is a recording of the electrical activity of the human heart, in St Mary’s Hospital, London in May 1887 [1]. Ventricular depolarisation and repolarisation were demonstrated using the Lippmann capillary electrometer. Waller had been a medical student in Aberdeen and Edinburgh and was made professor in the University of Aberdeen, Scotland, in 1881. He made further observations on ECGs on his dog Jimmie, who was often used in his lectures.
Around the same time, in Aberdeen, Scotland, John A. MacWilliam, Professor of the Institute of Medicine, introduced the term atrial flutter and the concept of ventricular fibrillation [2]. James Mackenzie, a Scottish Physician, published his own work in 1902 on the study of the pulse [3]. He used a home-made polygraph to record the action of all four chambers of the heart. His contribution to ECG development was acknowledged by Karel Frederik Wenckebach, the much-honoured Dutch physician who researched irregularities of cardiac rhythm.
Shortly thereafter, Willem Einthoven, based in Leiden in the Netherlands, introduced the three standard bipolar limb leads with the use of his own galvanometer, as a result of which he was awarded the Nobel Prize for Medicine in 1924 [4]. The first commercial version of the Einthoven electrocardiograph was produced in 1908 by the Cambridge Instrument Company in England. It recorded Einthoven’s three leads, I, II and III and used pails of conducting solution as electrodes.
Thomas Lewis, one of Mackenzie’s former junior staff members, published ‘The Mechanism and Graphic Registration of the Human Heart’. In its third edition, in 1925, it summarized early work on cardiac arrhythmias based on the use of Einthoven’s three limb leads.
It is unthinkable that these pioneers could have projected forwards over 100 years to predict what electrocardiography would be like at the present time. Electronic computers had not been invented and electrical circuitry had certainly not been miniaturised to the extent which it is nowadays.
Electrocardiography itself advanced from the use of 3 leads to what became known as the standard 12 lead configuration, although only 10 electrodes were required to derive the 12 signals [5]. Further advances were made through the use of multiple electrodes on the body surface which allowed the spread of electrical activation to be mapped [6]. Thereafter, modelling became extremely sophisticated and the cardiac electrical activity could be calculated from inverse modelling with body surface potentials as the input to the model [7].
In 1920, Hubert Mann of the Cardiographic Laboratory, Mount Sinai Hospital, New York, described the derivation of a ‘monocardiogram’ later to be called ‘vectorcardiogram’ or VCG [8]. Waller had also been interested in the concept of the vector force. The VCG displays P, QRS and T waves, in the form of ‘loops’ which are determined from vectors representing successive instantaneous mean electrical forces from the heart throughout an entire cardiac cycle. These forces are oriented three-dimensionally during each heartbeat and can be represented by a time sequence of vectors which display their magnitude and direction. A number of electrode arrays have been developed, aimed at recording the three components of the resultant cardiac electrical force, the so-called heart vector, in three mutually perpendicular directions. This approach became known as three orthogonal lead electrocardiography. The most popular lead system, a ‘corrected orthogonal lead system’, which recorded leads X, Y and Z, was developed by Ernest Frank in 1956 [9]. The vector loops were initially viewed on oscilloscopes.
Advances in data collection and in miniaturisation of ECG amplifiers and recording equipment greatly facilitated such studies. It goes without saying that the introduction of the digital computer itself also led to a transformation in the way that analogue ECG signals could be processed, interpreted and stored.
Other electrical circuits were used to record additional (unipolar and augmented unipolar) ECG leads, and the basic 12 lead ECG, i.e., a recording of 12 different electrical signals of which 8 were independent, was established by the early 1940s. A fuller account can be found elsewhere [10]. Since that time, many other developments have emerged in the interim, but the 12 lead ECG still remains the major approach to recording the electrical activity of the heart in hospitals and healthcare facilities worldwide. Its use is complemented by other techniques which have emerged more recently but, nevertheless, the 12 lead ECG has remained the rock on which other advances have been built.
2. The Early Days
The use of computers for ECG interpretation was first evaluated using the orthogonal lead ECG and the 12 lead ECG. The first approach to automating analysis of ECGs commenced in 1960 in the laboratory of Dr. Hubert V. Pipberger (Figure 1) using three simultaneously recorded orthogonal leads [11]. The Veteran’s Administration (VA) Hospital in Washington DC established a special research programme for medical electronic data processing as medical electronics began a period of growth, and Pipberger was appointed director [12].
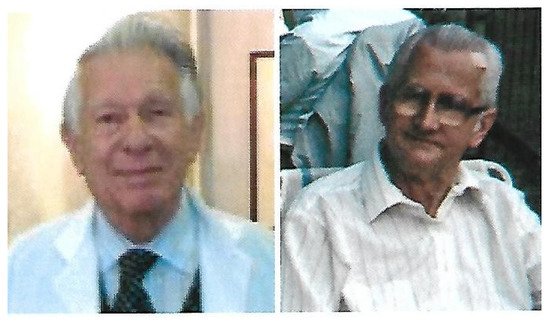
Figure 1. Dr. C. Caceres (left) and Dr. H. Pipberger (right).
Pipberger was born in Hamburg in 1920 and studied at the Rheinische Friedrich Wilhelms University in Bonn, Germany. He was an army doctor during World War II and was captured and imprisoned in France. He saved himself by telling stories in French, entertaining his captors [13].
A pioneer in the field of electrocardiology, he trained as a cardiologist and recognised the effectiveness of collaboration with electrical engineers, physicists, mathematicians, statisticians and computer programmers in problem solving and interdisciplinary research [14]. Dr. Pipberger’s lab based its early analysis system on the three orthogonal lead ECG [15]. Analogue ECG recordings had to be converted into digital data using rather large equipment [11], which has to be compared with the current possibility of converting an ECG signal into a digital form for analysis within a wearable such as a wristwatch. Each diagnostic output from Pipberger’s program had a probability attached on a scale of 0–1 and the sum of all outputs had to total 1. This could be confusing if a new diagnostic output was added, in a later ECG, to an existing abnormality which then had a reduced probability of being present.
In contrast, in 1959, Dr. Cesar Caceres (Figure 1) and his team in the National Institute of Health’s Medical Systems Development Laboratory, also in Washington DC, based their approach on the analysis of the 12 lead ECG using conventional clinical ECG criteria, but initially by processing one lead at a time [16]. Caceres coined the term ‘clinical engineering’, putting engineering into the clinical world of medicine in order that the various disciplines could work hand in hand to improve healthcare in practice. He graduated from Georgetown University and specialised in Internal Medicine at Tufts and Boston Universities in Boston, Massachusetts. He received Cardiology specialisation and research training from George Washington University [17].
This early work led to the expectation of the technique playing a significant role in ECG interpretation.
3. The Glasgow Contribution
One of the authors (PWM) began work in Glasgow on Computer Assisted Reporting of Electrocardiograms (C.A.R.E) as a student with Professor T.D. Veitch Lawrie in the Department of Medical Cardiology, University of Glasgow, who had anticipated an expansion of the use of computers in ECG analysis. Early work determined that the conventional 12 lead ECG and the three orthogonal lead ECG could be used for computer interpretation of ECGs and so diagnostic criteria were developed for both lead systems [18]. Additional vectorcardiographic measurements were made and incorporated into the diagnostic criteria. To record and analyse the ECGs, a standard 3 channel VCG system was combined with 3 single-channel electrocardiographic amplifiers and a multi-channel analogue tape recorder linked to a small PDP8 digital computer with an analogue–digital converter, allowing ECGs to be replayed from the tape recorder to the computer. An ECG database was accumulated in both analogue and digital form. In the early 1970s, portable ECG recording units were assembled which could be transported to wards and clinics easily on a trolley. The modified axial lead system [19] was used and the analysis time was the order of one minute. What was thought to be the first hospital-based mini-computer system for routine ECG interpretation was developed and introduced (Figure 2) in Glasgow Royal Infirmary around 1971 [20]. In the mid-70s, a hybrid lead system [21] was designed that combined the 12 lead and the three orthogonal lead ECG with the use of two additional electrodes (V5R and the neck), but there was little clinical acceptance.
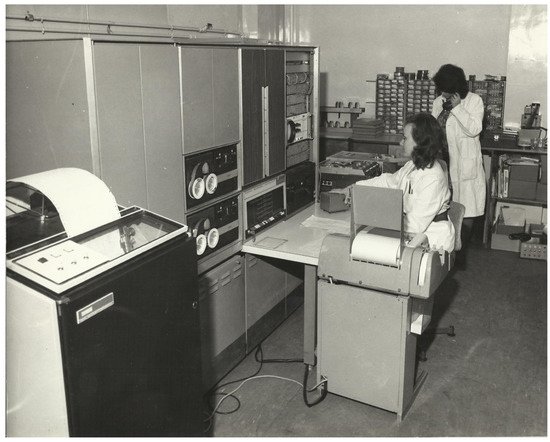
Figure 2. The first automated ECG interpretation system in operation in Glasgow Royal Infirmary around 1971. One technician controlled the tape recorder and listened to the patient details which were also recorded. The second technician monitored the three orthogonal lead ECG on the oscilloscope and started the analogue to digital conversion. The software was stored on the small digital tapes (DECtapes) and retrieved as necessary.
A major technological advance was the advent of the microprocessor and the arrival of automated ECG analysis at the bedside. In Glasgow, analogue to digital conversion at 500 samples per second was undertaken within an electrocardiograph designed and built by Dr. M. P. Watts, who had also introduced techniques for transmitting ECGs between a local hospital and the ECG lab for automated interpretation [22]. The analysis program was rewritten in Fortran and moved to a PDP11 series computer. New diagnostic criteria evolved for the 12 lead ECG including rhythm analysis and serial comparison [23]. Many clinical studies, some of which are described below, led to an enhanced program for automated ECG analysis, which was commercialised in the early 1980s.
4. Age, Sex and Racial Differences in the ECG
4.1. Neonatal and Paediatric ECG Analysis
The ECGs of the neonate, infant and child are completely different from the ECG of the adult. For this reason, special considerations apply to automated ECG interpretation of the neonatal and paediatric ECG.
The duration of the neonatal QRS complex is significantly shorter than that of the adult ECG, which implies a higher frequency content. This has often led to claims that the technology for recording the neonatal and paediatric ECG in general should be enhanced compared to that for recording the adult ECG. However, there has not been any study which has shown a clinically significant difference between a higher and a lower sampling rate when converting the ECG from analogue to digital form. Specifically, a major study by Rijnbeek [24] and colleagues from the Netherlands showed that reducing the sampling rate from 1000 samples per second to 500 samples per second had no impact on normal limits which they developed in infants and children.
The ECG of the newborn tends to have a QRS axis which is in the range of 90–180° which, for the adult, would be known as right axis deviation but for the baby is normal. This is simply a function of the path of circulation of blood through the foetus and the major role played by the right side of the heart at that stage in the development of the child. After the baby is born, the circulation changes and there is a gradual shift in emphasis of contraction, with the left ventricle becoming much more dominant than the right ventricle. It is probably not well appreciated that the ECG of the neonate therefore changes significantly, even over the first week of life. This was demonstrated by one of the authors (PWM) and colleagues [25]. Thus, interpretation of the neonatal ECG should ideally be based on a knowledge of the date of birth and date of recording so that changes from one day to another can be considered in an interpretation. Nowadays, new mothers are generally encouraged to leave hospital within 24 h or 48 h, and so trying to obtain a database of ECGs of neonates from birth to one week of life is currently extremely difficult.
Of course it goes without saying that, as the child grows, so does the heart and hence QRS duration, for example, linearly increases in duration from birth to adolescence. Allowance, therefore, has to be made for this in an interpretative program. Similarly, heart rate decreases shortly after birth, though not immediately, and again, simple equations can be used to set an upper limit of normal from the first week of life to adolescence [25].
It is suggested that with current advances, no matter how impressive, the use of machine learning will still prove challenging in the area of paediatric ECG interpretation.
4.2. Adult Age and Sex Differences in ECGs
There are many differences between adult male and female ECGs [26], and automated interpretation should be able to handle such variations with ease. In broad terms, QRS voltage is higher in younger compared to older persons, particularly in males, but this difference diminishes with increasing age. The same is true for ST amplitude, especially in the precordial leads, though it remains higher in males at all ages [27]. This latter publication eventually led to sex differences in ECG criteria being taken into account when reporting ST elevation myocardial infarction, as now acknowledged in the latest universal definition of myocardial infarction [28].
Mean QRS duration is higher in males than females though it is rare for this to be acknowledged in diagnostic criteria, with an exception being in ‘true’ left bundle branch block (LBBB) [29].
4.3. Racial Differences
It has been established that there is a clear ethnic variation in certain aspects of the ECG that should be acknowledged when making an interpretation. A number of studies have shown differences in normal limits of the ECG between Caucasians, Black people and Asian individuals [30][31] and diagnostic criteria should allow for this.
The availability of digital electrocardiographs and computers which can easily handle vast numbers of ECGs should allow for further work to be done on enhancing race-based diagnostic criteria. For example, it was noted that the mean ST segment amplitude is higher in Black people than in Caucasians and is higher in males than in females [30]. Rautaharju also showed that Black people had higher voltages than Caucasians in one of his studies [31]. From a historical perspective, Simonson pointed out racial differences in his 1961 treatise on the normal electrocardiogram [32]. His comparison was mainly between Caucasian and Japanese individuals, but differences were acknowledged at that time. One of the authors (PWM) also compared Caucasian with Indian, Nigerian and Chinese cohorts [30], showing a variety of differences, so it is important that race be acknowledged in ECG interpretation.
5. The European Contribution
In 1974, one of the authors (PWM) obtained a scholarship from the British Heart Foundation to spend one month in Europe visiting various centres which, by that time, had commenced work on some aspect of automated ECG interpretation. These included university departments in hospitals in Leuven in Belgium, Rotterdam in the Netherlands, Lyon in France, and Hannover in Germany. A report was compiled summarising the developments in progress and suggestions for collaboration were made. The net effect was that the European Economic Community, as it was known at the time, set up a project to further the technique of automated ECG analysis by supporting a joint project involving all those interested centres in various European countries. In due course, participation was opened to those from overseas, mainly the USA, who also had an interest in the topic. The North American delegates were mostly representatives from commercial companies developing products.
The project was entitled Common Standards for Quantitative Electrocardiography and it quickly became known as the CSE Project. A detailed summary of its main goals can be found elsewhere [33] and it arguably became the best-known project in automated electrocardiography. The project leader was Professor Jos Willems, who had spent time in Pipberger’s laboratory in Washington DC in the early stages of the development of the technique. He led the project from 1976 through to the early 1990s, when unfortunately he was found to have a brain tumour and died shortly thereafter [34].
Early in the project, a steering committee was established, consisting of Professor Jos Willems (Chairman), Rosanna Degani (Padua, Italy), Christoph Zywietz (Hannover, Germany), Peter Macfarlane (Glasgow, UK), Jan van Bemmel (Rotterdam, The Netherlands) and Pierre Arnaud (Lyon, France). Later, Paul Rubel from Lyon replaced Pierre Arnaud (Figure 3). The steering committee met almost quarterly for over 10 years and there were biennial meetings of the full working group where multiple individuals from the same team could attend.
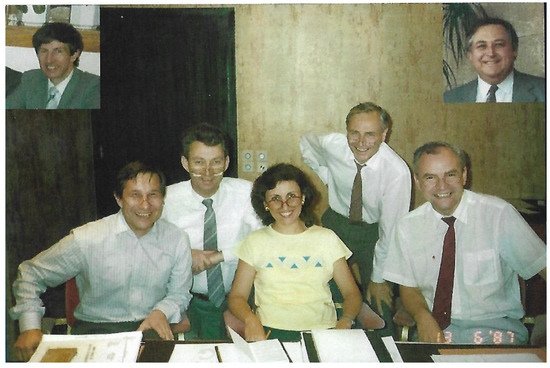
Figure 3. The CSE steering committee pictured in 1987 laughing at each other wearing glasses. The picture was taken by PWM. From left to right: (inset) Peter Macfarlane (1987); Christoph Zywietz; Jan van Bemmel; Rosanna Degani; Pierre Arnaud; Jos Willems; (inset) Paul Rubel (1992), who took over from Pierre Arnaud.
One of the biggest outcomes of the project was the establishment of databases, both of ECG waveforms for testing measurements and also of ECG interpretations from 1220 patients whose clinical condition was documented. These databases are still of importance to this day, over 30 years later.
The availability of the waveform database allowed the establishment of standards for ECG wave recognition which are still in use at the present time. The CSE diagnostic database resulted in a landmark publication [35] in 1991, where the accuracies of different diagnostic programs were assessed against both a clinical diagnosis and, separately, against the opinion of a group of eight cardiologists. Even today, companies wishing to submit data on performance of their software very often resort to using analysis based on the CSE diagnostic database. This requirement will continue in the new ISO/IEC standard for automated ECG interpretation which will be entitled ‘80601, Part 2-86: Particular requirements for the basic safety and essential performance of electrocardiographs, including diagnostic equipment, monitoring equipment, ambulatory equipment, electrodes, cables, and leadwires’. A summary of the expected contents based on a first draft already circulated can be found elsewhere in this issue [36].
The availability of a library of digitized ECGs made it possible for extensive recommendations on signal processing to be published as part of the CSE Study [37]. It should be noted that at that time (1985 and earlier), the majority of electrocardiographs produced recorded three leads simultaneously. Many of the recommendations therefore related to dealing with groups of three leads. Nevertheless, interval measures such as QT were recommended to be based on the longest QT interval measured in any single lead, though V1–V3 were suggested as giving the most accurate result. Other definitions, for example, included the exclusion of an isoelectric segment at the onset or termination of a QRS complex from the QRS duration in the lead in which it occurred. The overall QRS duration, nevertheless, was defined as the time from the earliest onset to the latest offset in the group of leads under consideration.
One of the interesting points to emerge from analysis of the CSE diagnostic database was that there were significant differences in sensitivity and specificity of diagnostic programs when the gold standard was, on the one hand, based on clinical data and, on the other, when it was based on the consensus interpretation of eight cardiologists. Some programs were developed on the basis of using clinical data while others were developed using cardiologist views as the gold standard, and that was reflected in the results of the study [35].
It is worthy of note that several programs developed in academic institutions in Europe were commercialised. These included the Glasgow program developed in the University of Glasgow [38], the HES program developed in the University of Hannover [39], and the MEANS program developed in the University of Rotterdam [40]. Software developed in the USA for commercial use was developed within industry, e.g., the Marquette—General Electric (GE) program, Hewlett Packard-Philips program, and the Mortara program.
It should also be noted that some programs used classical deterministic criteria, e.g., R amp in aVL > 1.5 mV, where others used a more statistical approach, involving probabilities. It was found that those programs which used classical criteria were more closely aligned with the gold standard based on cardiologist interpretations and conversely, those developed using probability theory were more closely aligned with the clinical data.
A typical example of this conundrum would be when the clinical diagnosis was left ventricular hypertrophy (LVH), which was based perhaps on a history of hypertension and an increased cardiothoracic ratio (1980s type of CSE criteria), but where the ECG was essentially within normal limits. The software developed according to a clinician’s view would report a normal ECG and that would be in line with the cardiologist interpretation. There is therefore agreement in that case between the computer and the cardiologist. On the other hand, both the computer program and the cardiologist are wrong with respect to the clinical diagnosis of LVH. Conversely, the statistical program would be more likely to report LVH correctly in line with the clinical diagnosis but would be wrong with respect to the cardiologist interpretation. This example explains why different results are obtained with different software and different gold standards.
This still remains a problem to some extent even with the newer techniques of machine learning, because more often than not when a large dataset is used for training, it can be that the cardiologist over-read of an ECG is used as the gold standard, although not always. This point will be considered later.
A by-product of the project was the establishment of a Standard Communications Protocol (SCP) for electrocardiography [41]. This was designed with the aim of providing data from different manufacturers’ ECG machines in a similar format which might for example contribute to a database or allow one vendor’s system to analyse ECGs recorded on another’s equipment. The SCP was strongly supported by Rubel who continued to regard it as of significant value, so much so that a new version has been released within the last year. Details can be found elsewhere in this issue [42].
In summary, the CSE Project has had a very significant influence over the field of automated ECG interpretation and still remains of great value at the present time.
References
- Waller, A.D. A demonstration in man of electromotive changes accompanying the heart’s beat. J. Physiol. 1887, 8, 229–234.
- McWilliam, J.A. Fibrillar contraction of the heart. J. Physiol. 1887, 8, 296–310.
- MacKenzie, J. The Study of the Pulse, Arterial, Venous, and Hepatic, and of the Movements of the Heart; Pentland: Edinburgh, UK, 1902.
- Snellen, H.A. Two Pioneers of Electrocardiography; Donker: Rotterdam, The Netherlands, 1983; p. 17.
- Macfarlane, P.W. Lead systems. In Comprehensive Electrocardiology, 2nd ed.; Macfarlane, P.W., van Oosterom, A., Pahlm, O., Kligfield, P., Janse, M., Camm, J., Eds.; Springer: London, UK, 2011; Volume 1, pp. 375–425.
- Lux, R.L. Body surface potential mapping techniques. In Comprehensive Electrocardiology, 2nd ed.; Macfarlane, P.W., van Oosterom, A., Pahlm, O., Kligfield, P., Janse, M., Camm, J., Eds.; Springer: London, UK, 2011; Volume 3, pp. 1361–1374.
- Ramanathan, C.; Ghanem, R.N.; Jia, P.; Ryu, K.; Rudy, Y. Electrocardiographic Imaging (ECGI): A Noninvasive Imaging Modality for Cardiac Electrophysiology and Arrhythmia. Nat. Med. 2004, 10, 422–428.
- Mann, H. A method of analysing the electrocardiogram. Arch. Int. Med. 1920, 25, 283–294.
- Frank, E. An accurate, clinically practical system for spatial vectorcardiography. Circulation 1956, 13, 737–749.
- Macfarlane, P.W. The coming of age of electrocardiology. In Comprehensive Electrocardiology, 2nd ed.; Macfarlane, P.W., van Oosterom, A., Pahlm, O., Kligfield, P., Janse, M., Camm, J., Eds.; Springer: London, UK, 2011; Volume 1, pp. 9–20.
- Pipberger, H.V.; Freis, E.D.; Taback, L.; Mason, H.L. Preparation of electrocardiographic data for analysis by digital electronic computer. Circulation 1960, 21, 413–418.
- Rautaharju, P.M. The birth of computerized electrocardiography: Hubert V. Pipberger. Cardiol. J. 2007, 14, 420–421.
- Bailey, J.J.; Dunn, R. Available online: http://ethw.org/Oral-History:James_J._Bailey_and_Rosalie_Dunn (accessed on 20 August 2021).
- Berson, A. In Memoriam. Hubert V. Pipberger, MD 1920–1993. Circulation 1993, 88, 817–818.
- Stallman, F.W.; Pipberger, H.V. Automatic recognition of electrocardiographic waves by digital computer. Circ. Res. 1961, 9, 1138–1143.
- Caceres, C.A.; Steinberg, C.A.; Abraham, S.; Carbery, W.J.; McBride, J.M.; Tolles, W.E.; Rikli, A.E. Computer extraction of electrocardiographic parameters. Circulation 1962, 25, 356–362.
- Cesar A. Caceres. Available online: https://bmet.fandom.com/wiki/Cesar_A._Caceres (accessed on 20 August 2021).
- Macfarlane, P.W.; Lorimer, A.R.; Lawrie, T.D.V. 3 and 12 lead electrocardiogram interpretation by computer. A comparison on 1093 patients. Brit. Heart J. 1971, 33, 266–274.
- Macfarlane, P.W. Modified axial lead system for orthogonal lead electrocardiography. Cardiovasc. Res. 1969, 3, 510–515.
- Macfarlane, P.W.; Cawood, H.T.; Taylor, T.P.; Lawrie, T.D.V. Routine automated electrocardiogram interpretation. Biomed. Eng. 1972, 7, 176–180.
- Macfarlane, P.W. A hybrid lead system for routine electrocardiography. In Progress in Electrocardiology; Macfarlane, P.W., Ed.; Pitman Medical: Tunbridge Wells, UK, 1979; pp. 1–5.
- Watts, M.P.; Macfarlane, P.W. 3-lead electrocardiogram transmission over Post Office telephone lines. Med. Biol. Eng. Comput. 1977, 15, 311–318.
- Macfarlane, P.W.; Podolski, M. Serial comparison in the Glasgow ECG analysis program. In Computerized Interpretation of the Electrocardiogram XI; Bailey, J.J., Ed.; Engineering Foundation: New York, NY, USA, 1986; pp. 110–113.
- Rijnbeek, P.R.; Witsenburg, M.; Schrama, E.; Hess, J.; Kors, J.A. New normal limits for the paediatric electrocardiogram. Eur. Heart J. 2001, 22, 702–711.
- Macfarlane, P.W.; Coleman, E.N.; Pomphrey, E.O.; McLaughlin, S.; Houston, A.; Aitchison, T.C. Normal limits of the high-fidelity ECG. Preliminary observations. J. Electrocardiol. 1989, 22, 162–168.
- Macfarlane, P.W. Influence of age and sex on the electrocardiogram. In Sex Specific Analysis of Cardiac Function; Kerkhof, P.L.M., Miller, V.M., Eds.; Springer: London, UK, 2018; pp. 93–106.
- Macfarlane, P.W. Age, sex, and the ST amplitude in health and disease. J. Electrocardiol. 2001, 34, 234–241.
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; European Society of Cardiology (ESC); Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269.
- Strauss, D.G.; Wagner, G.S. Defining left bundle branch block in the era of cardiac resynchronization therapy. Am. J. Cardiol. 2011, 107, 927–934.
- Macfarlane, P.W.; Katibi, I.A.; Hamde, S.T.; Singh, D.; Clark, E.; Devine, B.; Franq, B.G.; Lloyd, S.; Kumar, V. Racial differences in the ECG. J. Electrocardiol. 2014, 47, 809–814.
- Rautaharju, P.M.; Park, L.P.; Gottdiener, J.S.; Siscovick, D.; Boineau, R.; Smith, V.; Powe, N.R. Race- and sex-specific models for left ventricular mass in older populations. Factors influencing overestimation of left ventricular hypertrophy prevalence by ECG criteria in African-Americans. J. Electrocardiol. 2000, 33, 205–218.
- Simonson, E. Differentiation between Normal and Abnormal in Electrocardiography; C.V. Mosby: St. Louis, MO, USA, 1961; pp. 126–129.
- Willems, J.L.; Arnaud, P.; van Bemmel, J.H.; Degani, R.; Macfarlane, P.W.; Zywietz, C.; The CSE Working Party. Common Standards for Quantitative Electrocardiography: Goals and Main Results. Methods Inf. Med. 1990, 29, 263–271.
- Macfarlane, P.W. In memoriam: Jos Willems, MD, PhD (1939–1994). J. Electrocardiol. 1995, 28, 251–252.
- Willems, J.L.; Abreu-Lima, C.; Arnaud, P.; van Bemmel, J.H.; Brohet, C.; Degani, R.; Denis, B.; Gehring, J.; Graham, I.; van Herpen, G.; et al. The diagnostic performance of computer programs for the interpretation of electrocardiograms. N. Engl. J. Med. 1991, 325, 1767–1773.
- Young, B.; Schmid, J.J. The New ISO/IEC Standard for Automated ECG Interpretation. Hearts 2021, 2, 410–418.
- The CSE Working Party. Recommendations for measurement standards in quantitative electrocardiography. Eur. Heart J. 1985, 6, 815–825.
- Macfarlane, P.W.; Devine, B.; Latif, S.; McLaughlin, S.; Shoat, D.B.; Watts, M.P. Methodology of ECG interpretation in the Glasgow program. Methods Inf. Med. 1990, 29, 354–361.
- Zywietz, C.; Borovsky, D.; Gotsch, G.; Joseph, G. Methodology of ECG interpretation in the Hannover program. Methods Inf. Med. 1990, 29, 375–385.
- Van Bemmel, J.H.; Kors, J.A.; Van Herpen, G. Methodology of the modular ECG analysis system MEANS. Methods Inf. Med. 1990, 29, 346–353.
- Willems, J.L.; Arnaud, P.; Rubel, P.; Degani, R.; Macfarlane, P.W.; van Bemmel, J.H. A standard communications protocol for computerized electrocardiography. J. Electrocardiol. 1991, 24, 173–178.
- Rubel, P.; Fayn, J.; Macfarlane, P.W.; Pani, D.; Schlögl, A.; Värri, A. The History and Challenges of SCP-ECG: The Standard Communication Protocol for Computer-Assisted Electrocardiography. Hearts 2021, 2, 384–409.
More
