Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Conner Chen and Version 1 by Giovanni Ciccarelli.
Atherosclerosis is a multifactorial inflammatory pathology that involves metabolic processes. Improvements in therapy have drastically reduced the prognosis of cardiovascular disease. Nevertheless, a significant residual risk is still relevant, and is related to unmet therapeutic targets. Endothelial dysfunction and lipid infiltration are the primary causes of atherosclerotic plaque progression. In this contest, mitochondrial dysfunction can affect arterial wall cells, in particular macrophages, smooth muscle cells, lymphocytes, and endothelial cells, causing an increase in reactive oxygen species (ROS), leading to oxidative stress, chronic inflammation, and intracellular lipid deposition.
- mitochondrial disorders
- atherosclerosis
- endothelium
- cardiovascular disease
1. Introduction
Despite tremendous progresses in therapy in the last few years, cardiovascular diseases are still the leading cause of death worldwide [1,2][1][2]. To date, 18 million people die each year due to cardiovascular diseases [1,3,4,5,6,7][1][3][4][5][6][7]. These numbers are expected to increase, reaching 24 million yearly deaths worldwide from cardiovascular-related disease by 2030, with an average of over 66,000 per day, and a total global cost rising to over 1 trillion USD [1,3,4,5,6,7][1][3][4][5][6][7]. After a decline in mortality in recent decades, the numbers are rising again, reversing years of progress in both ischemic heart and cerebrovascular disease [1,4][1][4]. Thus, cardiovascular prevention is essential to make a 25% reduction in premature mortality from non-communicable diseases more realistic. There is an urgent need for plans and policies to reduce the burden of cardiovascular diseases which are a health challenge, starting from the territory and the role of cities in promoting health. There is also a need for improving the understanding of the basic mechanisms underlying cardiovascular diseases to design tailored therapy.
The atherosclerotic process is very often responsible for several cardiovascular and cerebrovascular diseases [8]. It is now well accepted and documented that atherosclerosis starts from endothelial dysfunction and lipid deposition, which progresses through macrophage infiltration, smooth muscle cell migration, and blood borne material deposition and becomes clinically relevant due to complications, eventually leading to local intravascular thrombus formation [8,9][8][9]. Modified lipoproteins, mainly oxidized low-density lipoproteins (oxLDL), are considered the major contributors to the genesis, progression, and immunological response occurring during the atherosclerotic process [10,11][10][11]. The first report linking mitochondria to atherosclerosis is from 1970 [12]. However, only in the last few years has increasing evidence really underlined the key role of mitochondrial dynamics in the pathogenesis of atherosclerosis [13]. Vascular cells, such as endothelial and smooth muscle cells, due to their metabolic functions and their barrier role are the main targets of mitochondrial dysfunction. In the atherosclerosis process, dysfunctional mitochondria might cause alterations in cellular metabolism and respiration resulting in the excessive production of reactive oxygen species (ROS), leading to oxidative stress [13]. While low levels of ROS exert important signaling functions [14[14][15],15], elevated ROS production induces the damage of cellular structures, alters DNA, proteins, and other molecules [16]. These conditions can become chronic, thereby favoring atherosclerosis progression and destabilization [17]. It is important to point out that mitochondrial dysfunction can be inherited and acquired [18]. Primary mitochondrial disease (PMD) is clinically diagnosed and confirmed by pathogenic mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) mutations [18]. However, there are some disorders with a ‘mitochondrial’ phenotype without identifiable mtDNA or nDNA mutations, or with variants of unknown clinical significance [18]. Conversely, secondary mitochondrial dysfunction (SMD) can be caused by genes encoding neither function nor production of oxphos proteins, and associated with many hereditary non-mitochondrial diseases [18]. This SMD can also be related to nongenetic causes, such as environmental factors and ageing. The strong relationship between ageing, atherosclerosis, and cardiovascular diseases is well established [19], and a correlation between mitochondrial dysfunction–ageing, and vice-versa, cannot be ruled out [20].
2. Mechanism of Mitochondrial Dysfunction and Molecular Implication for the Cardiovascular System
Mitochondria represent the engine of human cells generating ATP, and their function is regulated via mitophagy. However, mitochondria are also involved in the production of metabolites for protein assembling and signal transduction. Their metabolism is influenced by Ca2+ levels: low calcium concentrations can lead to mitochondrial dysfunction, while high levels of calcium can increase mitochondrial permeability [21]. As compared to other organs, the heart needs a high amount of energy; this is produced by oxidative metabolism in the mitochondria, which are one-third of the total volume of cardiomyocytes [22]. Mitochondrial dysfunctions are strongly related to cardiovascular diseases, in particular ischemic heart disease and atherosclerosis, cardiomyopathy, and hypertension [23]. This altered mitochondrial function results in reduced ATP, impairment of mitochondrial regulatory roles, reactive oxygen species (ROS) production and related signaling, cell growth and apoptosis, impaired mitochondrial electron transport chain activity, and an inflammatory response [24,25,26,27][24][25][26][27]. Mitochondrial fission and fusion impairments have been related to the development of cardiovascular diseases [28]. Novel mitochondrial biomarkers have been proposed to identify patients that can benefit from therapies specifically targeting mitochondria [29]. Mitochondrial homeostasis plays a crucial role in cells with high energy consumption, and in the pathological development of ischemic heart disease [30]. In particular, variation in the level of Ca2+ in mitochondria could lead to altered contraction coupling [31] and increased ROS levels during ischemic myocardial reperfusion, thereby inducing mitochondrial membrane damage, abnormal ATP synthesis, increased levels of Ca2+, and mPTP opening [32]. Thus, during ischemia, the mitochondrial succinate significantly increases in injured tissue [33,34][33][34], while during reperfusion, the accumulated metabolites are oxidized by the mitochondrial respiratory chain enzyme SDH (succinate dehydrogenase). This drives reactive oxygen species (ROS) production by reverse electron transport (RET) at mitochondrial complex I, stimulating mitochondrial permeability transition pore opening, and cell death associated with ischemia/reperfusion damage [35,36,37,38][35][36][37][38]. Sazanova et al. have demonstrated that specific mutations in the coding region of the mitochondrial genome, in particular m.14459G>A and m.5178C>A, are risk factors for occurrence and development of cardiac angina, while the mutation m.15059G>A instead had a protective effect [39]. Atherosclerosis is a chronic inflammatory condition characterized by impaired lipid metabolism, which stimulates innate and adaptive immune responses [9]. The presence of lipids in the intimal layer of arteries significantly affects mitochondrial activity/function. There are several mechanisms related to atherosclerosis progression and plaque instability, such as mutations in mitochondrial DNA (mtDNA), reactive oxidative species (ROS), and respiratory chain alterations, which induce hypertrophy of vascular smooth myocytes [40]. Mitochondrial ROS, associated with several risk factors, such as hyperglycemia and hypercholesterolemia [41], are involved in the expansion and potential damage of atherosclerotic plaques, particularly by inducing endothelial dysfunction, promoting monocyte infiltration, and increasing vascular smooth muscle cell and endothelial cell apoptosis [42]. Accumulation of ROS in the inner mitochondrial membrane can alter the mitochondrial cholesterol transporter, steroidogenic acute regulatory protein (StAR), which inhibits the storage of cholesterol through the mitochondrial membrane [43]. Under pathophysiological conditions, the dysfunctional mitochondria can stimulate the production of large amounts of ROS from adjacent mitochondria, modifying membrane potential, a process well known as “ROS-induced ROS”. Normally, this process of ROS is balanced by endogenous antioxidants. On the other hand, when there is an oxidative stress and hyper-production of ROS, the oxidative impairment in the arterial wall is increased [44], and a progression of the atherosclerotic plaque can be activated [45]. Mutations in mtDNA, related to ROS derived from mitochondrial dysfunction, are more frequent than in nuclear DNA and can cause impaired mitochondrial respiration in smooth muscle monocytes and macrophages, thereby contributing to atherosclerotic plaque progression [41]. In vitro studies have demonstrated that the damage induced byROS on mtDNA inhibits protein synthesis and alters gene expression, suggesting that ROS might mediate vascular cell dysfunction in the setting of atherogenesis [46] associated with changes in mitochondrial genome [47]. On the other hand, recent studies have put into question the correlation between ROS and mtDNA damage, highlighting that impaired mtDNA was observed in vascular and circulating cells before the development of atherosclerotic lesions [46]. Thus, these data suggested that the primary event is associated with mtDNA damage which increases ROS generation and variations in mitochondrial dysfunction and membrane potential, followed by activation of the apoptotic mechanism. Moreover, endogenous mitochondrial damage-associated molecular patterns (mtDAMPs) trigger sterile inflammation through various signaling pathways, including toll-like receptors (TLRs), nuclear factor kappa beta (NF-κβ), and the NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3) inflammasome [48]. In addition, damaged mtDNA can be seen as an endogenous damage-associated molecular pattern (DAMP), activating the inflammatory response [49].3. Mitochondrial Dysfunction and Endothelial Dysfunction
Endothelial cells represent the barrier for the molecular transport between blood and tissue, regulating the exchange of nutrients [53][50] and the vascular tone by production of nitric oxide (NO) and contractile factors. Nevertheless, in addition to its function as a barrier, the endothelium modulates inflammation, lipid metabolism, vascular tone, and hemostasis, and prevents penetration of inflammatory cells into the bloodstream. It also secretes adhesion molecules and cytokines involved in the inflammatory cascade [54,55][51][52]. Endothelial cells’ dysfunction is characterized by ROS production, in particular from mitochondria, infiltrations of LDL, and subsequent oxidation to oxLDL [56][53], which might induce endothelial impairment. This enhances the expression of adhesion molecules ICAM-1, VCAM-1, and P-selectins, resulting in smooth muscle cell growth and activation of inflammatory cells, such as monocytes and macrophages, thereby causing a pro-inflammatory burden by releasing cytokines and increasing circulating immune cells’ adhesion to the endothelium [57][54]. Damaged endothelium produces growth factors, which activates smooth muscle cells (SMCs) in the vascular bed and the phagocytosis of lipids, with subsequent evolution into the fibrous cap [58][55]. Mitochondria are important regulators of apoptosis and NO production in vascular endothelial cells, stimulating the cellular response to stress [59][56]. At the same time, the amounts of mitochondria in the endothelium are not abundant, but despite that, mitochondria not only affect energy supply, but also regulate blood oxygen levels and mediate NO-mediated vasodilation [60,61][57][58]. The decreased NO production in atherosclerotic plaques is mainly due to endothelial NO synthase (eNOS) degradation, induced by ROS-mediated oxidative stress. In addition, eNOS decoupling dysfunction produces additional ROS, which interfere with endothelial function, inducing the progression of atherosclerosis [62][59]. Recent studies have highlighted that the transcription factor NF-E2 p45-related factor 2 (Nrf2; gene name NFE2L2) regulates some mitochondrial functions [63][60] via the mtROS pathway, such as antioxidant activity, autophagy, and metabolism [64][61]. Nrf2 has a crucial role in the maintenance of cellular redox homeostasis by regulating biosynthesis, utilization, and regeneration of glutathione, thioredoxin, and NADPH, and controlling the production of ROS by mitochondria and NADPH oxidase. Moreover, Nrf2 activation inhibits Drp1-mediated mitochondrial fission, improving endothelial dysfunction [65][62]. Incubation of endothelial cells with oxLDL leads to an increase in the activity of mitochondrial complex I and oxidative stress [66][63], thereby stimulating the transcription and expression of superoxide dismutase 2 (SOD2) in macrophages [67][64]. Activation of mitophagy, a lysosome-mediated selective mitochondria degradation [68][65], is one of the characteristic signs of mitochondrial dysfunction and damage and leads to membrane potential collapse, increased ROS production, and decreased ATP levels, oxidative stress, and apoptosis [69][66]. The balance between mitophagy and mitochondrial neogenesis is crucial for correct homeostasis in the human body [70][67]. Mitochondrial biogenesis is an important process for maintaining energy control and protecting endothelial cells’ survival in critical pathological scenarios [71,72][68][69]. Mitochondrial dysfunction might represent the first real step of atherosclerosis by determining the endothelial impairment, which is the starting point of the atherosclerotic process [21]. The endothelial dysfunction, in particular decreased vasodilatation, is also typical of MELAS (Mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes) patients [73][70]. These patients can have lower levels of l-arginine, which regulates the endothelial-dependent vascular relaxation [74][71], which was significantly lowered in both acute and interictal phases of MELAS as compared to control subjects [75][72]. A schematic view of the atherosclerotic mitochondria-related process is shown in Figure 1.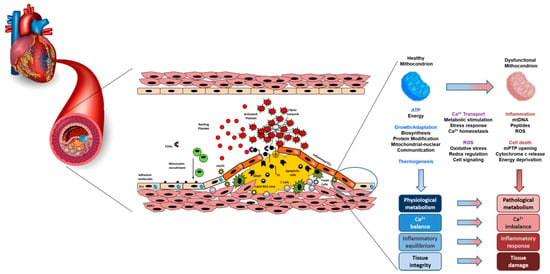
Figure 1.
A schematic view of the interaction between mitochondria dysfunction, atherosclerosis and oxidative stress.
References
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020, 141, e139–e596.
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021.
- Sanchez-Vinas, A.; Corral-Partearroyo, C.; Gil-Girbau, M.; Penarrubia-Maria, M.T.; Gallardo-Gonzalez, C.; Olmos-Palenzuela, M.D.; Aznar-Lou, I.; Serrano-Blanco, A.; Rubio-Valera, M. Effectiveness and cost-effectiveness of an intervention to improve Initial Medication Adherence to treatments for cardiovascular diseases and diabetes in primary care: Study protocol for a pragmatic cluster randomised controlled trial and economic model (the IMA-cRCT study). BMC Prim. Care 2022, 23, 170.
- Alizadeh, G.; Gholipour, K.; Azami-Aghdash, S.; Dehnavieh, R.; JafarAbadi, M.A.; Azmin, M.; Khodayari-Zarnaq, R. Social, Economic, Technological, and Environmental Factors Affecting Cardiovascular Diseases: A Systematic Review and Thematic Analysis. Int. J. Prev. Med. 2022, 13, 78.
- Lee, C.B.; Liao, C.M.; Peng, L.H.; Lin, C.M. Economic fluctuations and cardiovascular diseases: A multiple-input time series analysis. PLoS ONE 2019, 14, e0219358.
- Aminde, L.N.; Veerman, L. Interventions for the prevention of cardiovascular diseases: A protocol for a systematic review of economic evaluations in low-income and middle-income countries. BMJ Open 2016, 6, e013668.
- Leal, J.; Luengo-Fernandez, R.; Gray, A.; Petersen, S.; Rayner, M. Economic burden of cardiovascular diseases in the enlarged European Union. Eur. Heart J. 2006, 27, 1610–1619.
- Frak, W.; Wojtasinska, A.; Lisinska, W.; Mlynarska, E.; Franczyk, B.; Rysz, J. Pathophysiology of Cardiovascular Diseases: New Insights into Molecular Mechanisms of Atherosclerosis, Arterial Hypertension, and Coronary Artery Disease. Biomedicines 2022, 10, 1938.
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533.
- Boren, J.; Chapman, M.J.; Krauss, R.M.; Packard, C.J.; Bentzon, J.F.; Binder, C.J.; Daemen, M.J.; Demer, L.L.; Hegele, R.A.; Nicholls, S.J.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: Pathophysiological, genetic, and therapeutic insights: A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020, 41, 2313–2330.
- Khatana, C.; Saini, N.K.; Chakrabarti, S.; Saini, V.; Sharma, A.; Saini, R.V.; Saini, A.K. Mechanistic Insights into the Oxidized Low-Density Lipoprotein-Induced Atherosclerosis. Oxidative Med. Cell. Longev. 2020, 2020, 5245308.
- Greenberg, S.R. Atherosclerosis and mitochondria. Ann. Intern. Med. 1970, 73, 861–862.
- Salnikova, D.; Orekhova, V.; Grechko, A.; Starodubova, A.; Bezsonov, E.; Popkova, T.; Orekhov, A. Mitochondrial Dysfunction in Vascular Wall Cells and Its Role in Atherosclerosis. Int. J. Mol. Sci. 2021, 22, 8990.
- Sinenko, S.A.; Starkova, T.Y.; Kuzmin, A.A.; Tomilin, A.N. Physiological Signaling Functions of Reactive Oxygen Species in Stem Cells: From Flies to Man. Front. Cell Dev. Biol. 2021, 9, 714370.
- Zhang, J.; Wang, X.; Vikash, V.; Ye, Q.; Wu, D.; Liu, Y.; Dong, W. ROS and ROS-Mediated Cellular Signaling. Oxidative Med. Cell. Longev. 2016, 2016, 4350965.
- Yang, S.; Lian, G. ROS and diseases: Role in metabolism and energy supply. Mol. Cell. Biochem. 2020, 467, 1–12.
- Suarez-Rivero, J.M.; Pastor-Maldonado, C.J.; Povea-Cabello, S.; Alvarez-Cordoba, M.; Villalon-Garcia, I.; Talaveron-Rey, M.; Suarez-Carrillo, A.; Munuera-Cabeza, M.; Sanchez-Alcazar, J.A. From Mitochondria to Atherosclerosis: The Inflammation Path. Biomedicines 2021, 9, 258.
- Niyazov, D.M.; Kahler, S.G.; Frye, R.E. Primary Mitochondrial Disease and Secondary Mitochondrial Dysfunction: Importance of Distinction for Diagnosis and Treatment. Mol. Syndromol. 2016, 7, 122–137.
- North, B.J.; Sinclair, D.A. The intersection between aging and cardiovascular disease. Circ. Res. 2012, 110, 1097–1108.
- Haas, R.H. Mitochondrial Dysfunction in Aging and Diseases of Aging. Biology 2019, 8, 48.
- Shemiakova, T.; Ivanova, E.; Wu, W.K.; Kirichenko, T.V.; Starodubova, A.V.; Orekhov, A.N. Atherosclerosis as Mitochondriopathy: Repositioning the Disease to Help Finding New Therapies. Front. Cardiovasc. Med. 2021, 8, 660473.
- Jennings, R.B.; Ganote, C.E. Mitochondrial structure and function in acute myocardial ischemic injury. Circ. Res. 1976, 38, I80–I91.
- Forte, M.; Schirone, L.; Ameri, P.; Basso, C.; Catalucci, D.; Modica, J.; Chimenti, C.; Crotti, L.; Frati, G.; Rubattu, S.; et al. The role of mitochondrial dynamics in cardiovascular diseases. Br. J. Pharmacol. 2021, 178, 2060–2076.
- Zhou, B.; Tian, R. Mitochondrial dysfunction in pathophysiology of heart failure. J. Clin. Investig. 2018, 128, 3716–3726.
- Iglewski, M.; Hill, J.A.; Lavandero, S.; Rothermel, B.A. Mitochondrial fission and autophagy in the normal and diseased heart. Curr. Hypertens. Rep. 2010, 12, 418–425.
- Lee, C.F.; Chavez, J.D.; Garcia-Menendez, L.; Choi, Y.; Roe, N.D.; Chiao, Y.A.; Edgar, J.S.; Goo, Y.A.; Goodlett, D.R.; Bruce, J.E.; et al. Normalization of NAD+ Redox Balance as a Therapy for Heart Failure. Circulation 2016, 134, 883–894.
- Luongo, T.S.; Lambert, J.P.; Gross, P.; Nwokedi, M.; Lombardi, A.A.; Shanmughapriya, S.; Carpenter, A.C.; Kolmetzky, D.; Gao, E.; van Berlo, J.H.; et al. The mitochondrial Na+/Ca2+ exchanger is essential for Ca2+ homeostasis and viability. Nature 2017, 545, 93–97.
- Chehaitly, A.; Guihot, A.L.; Proux, C.; Grimaud, L.; Aurriere, J.; Legouriellec, B.; Rivron, J.; Vessieres, E.; Tetaud, C.; Zorzano, A.; et al. Altered Mitochondrial Opa1-Related Fusion in Mouse Promotes Endothelial Cell Dysfunction and Atherosclerosis. Antioxidants 2022, 11, 1078.
- Hubens, W.H.G.; Vallbona-Garcia, A.; de Coo, I.F.M.; van Tienen, F.H.J.; Webers, C.A.B.; Smeets, H.J.M.; Gorgels, T. Blood biomarkers for assessment of mitochondrial dysfunction: An expert review. Mitochondrion 2022, 62, 187–204.
- Xin, Y.; Zhang, X.; Li, J.; Gao, H.; Li, J.; Li, J.; Hu, W.; Li, H. New Insights Into the Role of Mitochondria Quality Control in Ischemic Heart Disease. Front. Cardiovasc. Med. 2021, 8, 774619.
- Garbincius, J.F.; Luongo, T.S.; Jadiya, P.; Hildebrand, A.N.; Kolmetzky, D.W.; Mangold, A.S.; Roy, R.; Ibetti, J.; Nwokedi, M.; Koch, W.J.; et al. Enhanced NCLX-dependent mitochondrial Ca2+ efflux attenuates pathological remodeling in heart failure. J. Mol. Cell. Cardiol. 2022, 167, 52–66.
- Lesnefsky, E.J.; Chen, Q.; Tandler, B.; Hoppel, C.L. Mitochondrial Dysfunction and Myocardial Ischemia-Reperfusion: Implications for Novel Therapies. Annu. Rev. Pharmacol. Toxicol. 2017, 57, 535–565.
- Martin, J.L.; Costa, A.S.H.; Gruszczyk, A.V.; Beach, T.E.; Allen, F.M.; Prag, H.A.; Hinchy, E.C.; Mahbubani, K.; Hamed, M.; Tronci, L.; et al. Succinate accumulation drives ischaemia-reperfusion injury during organ transplantation. Nat. Metab. 2019, 1, 966–974.
- Zhang, J.; Wang, Y.T.; Miller, J.H.; Day, M.M.; Munger, J.C.; Brookes, P.S. Accumulation of Succinate in Cardiac Ischemia Primarily Occurs via Canonical Krebs Cycle Activity. Cell Rep. 2018, 23, 2617–2628.
- Chouchani, E.T.; Pell, V.R.; James, A.M.; Work, L.M.; Saeb-Parsy, K.; Frezza, C.; Krieg, T.; Murphy, M.P. A Unifying Mechanism for Mitochondrial Superoxide Production during Ischemia-Reperfusion Injury. Cell Metab. 2016, 23, 254–263.
- Milliken, A.S.; Kulkarni, C.A.; Brookes, P.S. Acid enhancement of ROS generation by complex-I reverse electron transport is balanced by acid inhibition of complex-II: Relevance for tissue reperfusion injury. Redox Biol. 2020, 37, 101733.
- Yin, Z.; Burger, N.; Kula-Alwar, D.; Aksentijevic, D.; Bridges, H.R.; Prag, H.A.; Grba, D.N.; Viscomi, C.; James, A.M.; Mottahedin, A.; et al. Structural basis for a complex I mutation that blocks pathological ROS production. Nat. Commun. 2021, 12, 707.
- Chouchani, E.T.; Pell, V.R.; Gaude, E.; Aksentijevic, D.; Sundier, S.Y.; Robb, E.L.; Logan, A.; Nadtochiy, S.M.; Ord, E.N.J.; Smith, A.C.; et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature 2014, 515, 431–435.
- Sazonova, M.A.; Ryzhkova, A.I.; Sinyov, V.V.; Sazonova, M.D.; Nikitina, N.N.; Shkurat, T.P.; Sobenin, I.A.; Orekhov, A.N. Mitochondrial mutations associated with cardiac angina. Vessel Plus 2019, 3, 8.
- Shemiakova, T.; Ivanova, E.; Grechko, A.V.; Gerasimova, E.V.; Sobenin, I.A.; Orekhov, A.N. Mitochondrial Dysfunction and DNA Damage in the Context of Pathogenesis of Atherosclerosis. Biomedicines 2020, 8, 166.
- Madamanchi, N.R.; Runge, M.S. Mitochondrial dysfunction in atherosclerosis. Circ. Res. 2007, 100, 460–473.
- Hulsmans, M.; Van Dooren, E.; Holvoet, P. Mitochondrial reactive oxygen species and risk of atherosclerosis. Curr. Atheroscler. Rep. 2012, 14, 264–276.
- Wen, R.; Banik, B.; Pathak, R.K.; Kumar, A.; Kolishetti, N.; Dhar, S. Nanotechnology inspired tools for mitochondrial dysfunction related diseases. Adv. Drug Deliv. Rev. 2016, 99, 52–69.
- Naik, E.; Dixit, V.M. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J. Exp. Med. 2011, 208, 417–420.
- Yu, E.P.K.; Reinhold, J.; Yu, H.; Starks, L.; Uryga, A.K.; Foote, K.; Finigan, A.; Figg, N.; Pung, Y.F.; Logan, A.; et al. Mitochondrial Respiration Is Reduced in Atherosclerosis, Promoting Necrotic Core Formation and Reducing Relative Fibrous Cap Thickness. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 2322–2332.
- Ballinger, S.W.; Patterson, C.; Yan, C.N.; Doan, R.; Burow, D.L.; Young, C.G.; Yakes, F.M.; Van Houten, B.; Ballinger, C.A.; Freeman, B.A.; et al. Hydrogen peroxide- and peroxynitrite-induced mitochondrial DNA damage and dysfunction in vascular endothelial and smooth muscle cells. Circ. Res. 2000, 86, 960–966.
- Hu, H.; Lin, Y.; Xu, X.; Lin, S.; Chen, X.; Wang, S. The alterations of mitochondrial DNA in coronary heart disease. Exp. Mol. Pathol. 2020, 114, 104412.
- Nakahira, K.; Hisata, S.; Choi, A.M. The Roles of Mitochondrial Damage-Associated Molecular Patterns in Diseases. Antioxid. Redox Signal. 2015, 23, 1329–1350.
- Zakirov, F.H.; Zhang, D.; Grechko, A.V.; Wu, W.K.; Poznyak, A.V.; Orekhov, A.N. Lipid-based gene delivery to macrophage mitochondria for atherosclerosis therapy. Pharmacol. Res. Perspect. 2020, 8, e00584.
- Liao, J.K. Linking endothelial dysfunction with endothelial cell activation. J. Clin. Investig. 2013, 123, 540–541.
- Poredos, P.; Poredos, A.V.; Gregoric, I. Endothelial Dysfunction and Its Clinical Implications. Angiology 2021, 72, 604–615.
- Sima, A.V.; Stancu, C.S.; Simionescu, M. Vascular endothelium in atherosclerosis. Cell Tissue Res. 2009, 335, 191–203.
- Mundi, S.; Massaro, M.; Scoditti, E.; Carluccio, M.A.; van Hinsbergh, V.W.M.; Iruela-Arispe, M.L.; De Caterina, R. Endothelial permeability, LDL deposition, and cardiovascular risk factors—A review. Cardiovasc. Res. 2018, 114, 35–52.
- Moriya, J. Critical roles of inflammation in atherosclerosis. J. Cardiol. 2019, 73, 22–27.
- Bennett, M.R.; Sinha, S.; Owens, G.K. Vascular Smooth Muscle Cells in Atherosclerosis. Circ. Res. 2016, 118, 692–702.
- Dominic, E.A.; Ramezani, A.; Anker, S.D.; Verma, M.; Mehta, N.; Rao, M. Mitochondrial cytopathies and cardiovascular disease. Heart 2014, 100, 611–618.
- Tretter, L.; Ambrus, A. Measurement of ROS homeostasis in isolated mitochondria. Methods Enzymol. 2014, 547, 199–223.
- Sun, Q.; Zhong, W.; Zhang, W.; Zhou, Z. Defect of mitochondrial respiratory chain is a mechanism of ROS overproduction in a rat model of alcoholic liver disease: Role of zinc deficiency. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G205–G214.
- Frey, R.S.; Gao, X.; Javaid, K.; Siddiqui, S.S.; Rahman, A.; Malik, A.B. Phosphatidylinositol 3-kinase gamma signaling through protein kinase Czeta induces NADPH oxidase-mediated oxidant generation and NF-kappaB activation in endothelial cells. J. Biol. Chem. 2006, 281, 16128–16138.
- Dinkova-Kostova, A.T.; Abramov, A.Y. The emerging role of Nrf2 in mitochondrial function. Free. Radic. Biol. Med. 2015, 88, 179–188.
- Cheng, X.; Siow, R.C.; Mann, G.E. Impaired redox signaling and antioxidant gene expression in endothelial cells in diabetes: A role for mitochondria and the nuclear factor-E2-related factor 2-Kelch-like ECH-associated protein 1 defense pathway. Antioxid. Redox Signal. 2011, 14, 469–487.
- Zhu, Y.; Li, M.; Lu, Y.; Li, J.; Ke, Y.; Yang, J. Ilexgenin A inhibits mitochondrial fission and promote Drp1 degradation by Nrf2-induced PSMB5 in endothelial cells. Drug Dev. Res. 2019, 80, 481–489.
- Ceaser, E.K.; Ramachandran, A.; Levonen, A.L.; Darley-Usmar, V.M. Oxidized low-density lipoprotein and 15-deoxy-delta 12,14-PGJ2 increase mitochondrial complex I activity in endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2003, 285, H2298–H2308.
- Kinscherf, R.; Deigner, H.P.; Usinger, C.; Pill, J.; Wagner, M.; Kamencic, H.; Hou, D.; Chen, M.; Schmiedt, W.; Schrader, M.; et al. Induction of mitochondrial manganese superoxide dismutase in macrophages by oxidized LDL: Its relevance in atherosclerosis of humans and heritable hyperlipidemic rabbits. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 1997, 11, 1317–1328.
- Yang, X.; Pan, W.; Xu, G.; Chen, L. Mitophagy: A crucial modulator in the pathogenesis of chronic diseases. Clin. Chim. Acta Int. J. Clin. Chem. 2020, 502, 245–254.
- Garza-Lombo, C.; Pappa, A.; Panayiotidis, M.I.; Franco, R. Redox homeostasis, oxidative stress and mitophagy. Mitochondrion 2020, 51, 105–117.
- Dymkowska, D. The involvement of autophagy in the maintenance of endothelial homeostasis: The role of mitochondria. Mitochondrion 2021, 57, 131–147.
- Drabarek, B.; Dymkowska, D.; Szczepanowska, J.; Zablocki, K. TNFalpha affects energy metabolism and stimulates biogenesis of mitochondria in EA.hy926 endothelial cells. Int. J. Biochem. Cell Biol. 2012, 44, 1390–1397.
- Dymkowska, D.; Drabarek, B.; Michalik, A.; Nowak, N.; Zablocki, K. TNFalpha stimulates NO release in EA.hy926 cells by activating the CaMKKbeta-AMPK-eNOS pathway. Int. J. Biochem. Cell Biol. 2019, 106, 57–67.
- Koga, Y.; Akita, Y.; Junko, N.; Yatsuga, S.; Povalko, N.; Fukiyama, R.; Ishii, M.; Matsuishi, T. Endothelial dysfunction in MELAS improved by l-arginine supplementation. Neurology 2006, 66, 1766–1769.
- Wang, X.L.; Sim, A.S.; Badenhop, R.F.; McCredie, R.M.; Wilcken, D.E. A smoking-dependent risk of coronary artery disease associated with a polymorphism of the endothelial nitric oxide synthase gene. Nat. Med. 1996, 2, 41–45.
- Koga, Y.; Akita, Y.; Nishioka, J.; Yatsuga, S.; Povalko, N.; Tanabe, Y.; Fujimoto, S.; Matsuishi, T. L-arginine improves the symptoms of strokelike episodes in MELAS. Neurology 2005, 64, 710–712.
More
