2.2. Aptamers in ALL
ALL is the most prevalent type of childhood tumor, representing approximately 80% of total childhood leukemia, with over 349,000 new cases diagnosed worldwide in 2018
[39][40][41][62,63,64]. In addition, the prevalence of ALL is increasing every year and poses a huge threat to human health. The standard regimen for ALL is a combination of chemotherapy, radiation therapy, and surgery. Due to its unsatisfactory curative effect and strong systematic side effects, the current treatment is far from achieving the best effect
[42][43][65,66]. Nowadays, with the fast development of biomedicine, aptamers hold great promise in treating ALL.4
2.3. Aptamers in CML
CML is a malignancy formed by the clonal proliferation of bone marrow hematopoietic stem cells
[44][98]. Most patients with CML have the Philadelphia (Ph) chromosome, which is the product of a t (9; 22) translocation between chromosomes 9 and 22. During this translocation, the ABL fragment of the proto-oncogene on chromosome 9 translocate to chromosome 22 and fuse with the BCR gene, forming the chimeric fusion gene BCR-ABL
[45][99]. Oncogene-specific gene therapy is a highly promising strategy for the treatment of CML.
Ping et al. developed an aptamer that specifically targets the BCR-ABL gene and found that the aptamer-siRNA complex significantly induces apoptosis in the myeloid leukemia cell line K562 cells, providing a reference for gene therapy in CML patients
[46][100].
The use of tyrosine kinase inhibitors (TKI) can significantly improve CML outcomes and prolong survival, but resistance to TKI has become a serious challenge in the treatment of myeloid leukemia. NOX-A12 is an RNA oligonucleotide in L-configuration (Spiegelmer) that binds and neutralizes the chemokine CXCL12 with high affinity and specificity, The results of Weisberg et al. showed that the combination of NOX-A12 and TKIs was able to block CXCL12-induced migration of BCR-ABL-positive leukemia (e.g., CML) cells more effectively in vitro to promote the treatment of cancer, and the same results were obtained in vivo experiments in CML model mice
[47][101].
There are still relatively few studies on aptamers in CML, mainly on the use of aptamers as a targeting tool for CML cells using siRNA to induce apoptosis to achieve therapeutic effects, or aptamer-specific binding to target cells can effectively inhibit chronic myeloid leukemia cell migration. Currently, there is still a large gap in the diagnosis and treatment of CML with aptamers. Although the treatment of CML is well established, with the low price of aptamers, the diagnosis and treatment of aptamers in CML still have the potential for continued research.
2.4. Aptamers in CLL
CLL is the most widespread type of leukemia in Western adults (accounting for approximately 25% of adult leukemias), with a median age at diagnosis of 72 years and a higher incidence in males
[48][49][50][51][102,103,104,105]. Common symptoms are peripheral blood lymphocytosis, lymph node enlargement, hepatosplenomegaly, bone marrow failure, autoimmune hemolytic anemia, and thrombocytopenia
[52][53][106,107]. CLL is a heterogeneous disease that can be divided into indolent and aggressive forms based on its clinical course and response to treatment. Some patients survive longer without symptoms for decades after diagnosis or without the disease progressing to severe disease, while others progress rapidly to a high-risk state requiring immediate treatment after diagnosis and may eventually die due to complications from treatment or disease progression. However, the clinical status of most CLL patients falls somewhere in between these two conditions requiring early diagnosis or treatment
[51][54][55][105,108,109]. Therefore, the aptamer can be very helpful as a potential clinical diagnostic or therapeutic tool for patients with CLL.
The amount of eEF1A1/eEF1A2 was quantified in the lymphocytes of 46 CLL patients versus normal controls. Dapas et al.
[56][110] found elevated eEF1A1/eEF1A2 in CLL lymphocytes. In addition, eEF1A1 levels were higher in patients who died compared to survivors. Therefore, eEF1A1 may serve as a prognostic marker and a therapeutic target for CLL. GT75 aptamer, which contains the GT (guanosine-thymidine) repeat T(GTTT)18GT (75 nucleotides total length). This aptamer can bind eEF1A1 in a variety of human cells
[57][58][59][111,112,113]. The Dapas team used GT75 to cause reduced viability/autophagy stimulation of MEC-1 (CLL cells) and downregulation of tumor growth in vivo.
CXCL12 is a chemokine that supports the survival of CLL cells in the bone marrow and lymph node microenvironment by interacting with CXCR4 to promote the homing and retention of hematopoietic and immune cells and their trafficking
[60][61][114,115]. In a phase IIa study, treatment with NOX-A12 was found to improve the pharmacodynamic effect of CLL cells effectively
[62][116]. Hollenrigel et al. showed that by inhibiting CXCL12 with NOX-A12, they could modulate the tumor microenvironment, thereby mobilizing leukemic cells to the peripheral blood and making CLL cells more susceptible to cytotoxic drugs
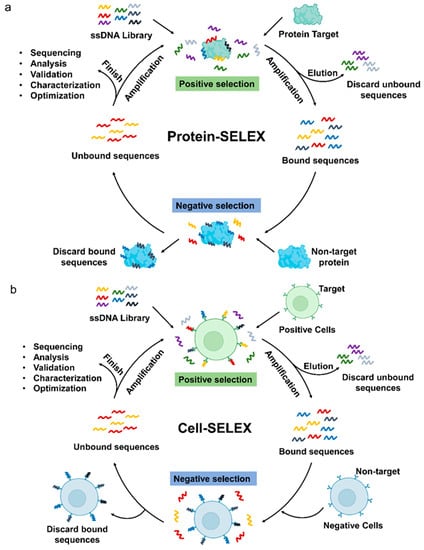
[63][117]. The research on aptamer therapy for CLL is still in its initial stage, and researchers have found higher levels of EEF1A1 in lymphocytes of CLL patients, so they have screened it as a therapeutic target to obtain aptamers for CLL. The aptamer in CLL is a Protein-SELEX progress, and perhaps using Cell-SELEX to screen for cell lines commonly used in CLL may lead to new targets for CLL therapy, which may be of great help in the treatment of CLL.
In leukemia diagnosis and treatment, aptamers have been studied in a considerable number, in which they contribute to the early diagnosis of leukemia and also serve as drug delivery tools for targeted therapy, enhancing the toxicity of various chemotherapeutic drugs to target cells and reducing the damage to normal tissues of the patient’s body, indicating that there is great potential for the application of aptamers in the clinical diagnosis or treatment of leukemia. However, there are still many problems in the research of aptamers in leukemia, firstly, there are abundant studies in AML and ALL, but there is still a lack of sufficient studies in CML and CLL, leaving a big gap that needs to be further promoted. Secondly, among these aptamers, only AS1411 and NOXA-12 have been promoted in clinical trials, while other aptamers still need to be tested in clinical trials. Meanwhile, the development of aptamers as early diagnostic reagents for leukemia can be considered. Aptamers are low-cost and very sensitive for leukemia diagnosis in combination with various biomaterials, and it is valuable to develop low-invasive diagnostic reagents for leukemia.
3. Aptamers in Lymphoma
Lymphomas are hematologic malignancies originating from different types of lymphocytes, mainly located in lymph nodes or other lymphatic structures, and are considered solid tumors of the immune system
[64][65][120,121]. Malignant lymphoma is now the most prevalent hematological neoplasm and its pathological types can be divided into non-Hodgkin’s lymphoma (NHL) and Hodgkin’s lymphoma (HL). The latter can be further divided into B cell origin and T/NK cell origin according to its source
[66][67][68][122,123,124]. Currently, aptamer-mediated targeted therapy and early diagnosis offer a promising new approach to lymphoma research.
Studies show that CD30 protein is overexpressed in anaplastic large cell lymphoma (ALCL) and classical Hodgkin’s lymphoma(cHL)
[69][70][125,126]. ALCL is a separate type of NHL. Parekh et al. generated ssDNA aptamers (C2) that bind CD30 with high affinity and specificity by a hybrid SELEX approach, and further optimized them to produce shorter truncated variants (C2NP,31nt) with 50-fold higher affinity
[71][127]. They found that C2NP polymers could induce apoptosis in ALCL cells by CD30 receptor oligomerization followed by activation of downstream signals. Xiao Luo et al. developed PEG-PLGA NPs encapsulated with Dox and modified with C2NP to prepare targeted formulations
[72][128]. The release time of the drug was effectively increased in the targeted formulation and accumulated more in ALCL cells than in non-targeted cells. This demonstrates the great potential of using C2NP-functionalized nanoparticles for the treatment of ALCL. Therefore, Chen Run et al.
[73][129]. modified straight and twisted DNA nanotubes with C2NP and loaded Dox, in which the interaction of C2NP with its receptor CD30 upregulated p53 expression and led to apoptosis of K299 cells (ALCL cell line). Zhao et al. exploited the aberrant expression of CD30 and anaplastic lymphoma kinase (ALK) genes in lymphoma cells by combining ALK siRNA and RNA-based CD30 aptamer probes into nano-sized polyethyleneimine-citrate carriers to construct nanocomplexes that specifically silenced ALK gene expression in lymphoma cells, causing growth arrest and apoptosis
[74][130]. In addition, a multifunctional aptamer-nanomedicine (Apt-NMed) containing not only CD30-specific aptamer and ALK-specific siRNA but also loaded with Dox was developed to enable targeted chemotherapy and synergistic gene therapy for ALCL. The Apt-NMed-mediated treatment not only significantly improved the survival of the mice compared to the control group but also reduced the side effects
[75][131]. Zeng reported a CD30 aptamer-modified protamine nanomedicine containing a dsDNA/drug that effectively killed lymphoma cells as well as an ALK-specific siRNA, and importantly, the complex was virtually nontoxic to off-target cells
[76][132]. CD30 aptamer has excellent performance in the treatment of ALCL, which can effectively increase the retention time of the drug in the target cells and prolong the release time of the drug, as well as specifically target siRNA to ALCL cells to inhibit ALK gene expression, leading to cell growth arrest and death, and has almost no toxic effects on non-targeted cells, these results suggest that CD30 may be a potential tool for targeted therapy against ALCL.
Based on the property that CD19 is overexpressed in the majority of human B-cell tumors, Yan Hu et al. identified the CD19 aptamer (LC1), a 59-nucleotide ss DNA that binds recombinant CD19 protein with high affinity (Kd = 85.4 nM)
[77][133]. LC1 was shown to specifically bind CD19-positive lymphoma cells (Ramos and Raji) and selective delivery of Dox was achieved in vitro by constructing LC1-Dox.
Mallikaratchy et al. used Ramos cells to identify TD05 aptamers that selectively bind membrane-bound immunoglobulin mu heavy chains, a target that is a major component of the B-cell receptor expressed in Burkitt’s lymphoma and could serve as a biomarker for Burkitt’s lymphoma
[78][79][80][134,135,136]. A few years later, Mallikaratchy’s group prepared TD05 aptamer-engineered polymorphs that reacted with the B-cell receptor and demonstrated B-cell specificity in lymphoma cell lines and fresh clinical leukemia samples
[81][137].
The B-cell activating factor (BAFF) receptor (BAFF-R) is overexpressed in B-cell malignancies such as NHL and may serve as a potential biomarker for tumors. Zhou et al. used in vitro SELEX to select 2’-F-modified RNA aptamers with a high affinity for BAFF-R that were able to block BAFF-mediated B cell proliferation and internalize it into B cells by binding effectively to BAFF-R
[82][138]. Subsequently, Zhou et al. described a BAFF-R aptamer-siRNA delivery system that specifically delivered STAT3 siRNA to various B-cell lines, resulting in gene silencing of mesangial STAT3 mRNA
[83][139].
Opazo et al. reported a DNA aptamer (C10.36) with an unconventional G-quadruplex structure that binds with high affinity and specifically enters Burkitt lymphoma cells and can be used as an efficient tool for the specific delivery of different cargoes to tumor cells
[84][140]. Through further studies, Tonapi et al. found that some lymphoma cells display a spliceosome complex (SSC) on their surface, consisting of at least 13 core components, and are binding targets for C10.36. Furthermore, the binding of C10.36 to lymphoma cells triggers SSC internalization, leading to global changes in variable splicing patterns and ultimately cell death
[85][141].
CD20 is a target of B cells, and Haghighi et al. used Cell-SELEX on recombinant HEK293T-CD20 cells to identify an aptamer named AP-1 that binds CD20 with high affinity (96.91 ± 4.5 nM), promising for diagnostic and therapeutic applications in lymphoma
[86][142]. A novel anti-lymphoma nano-drug CD20 aptamer-RBCm@Ag-MOFs/PFK15 (A-RAMP) was designed and prepared
[87][143]. The results showed that A-RAMP could effectively target B-cell lymphoma and exert synergistic antitumor effects with Ag
+ and FPK15 by reprogramming aerobic glycolysis.
Zümrüt et al. recently introduced a SELEX variant called “Ligand-Guided-Selection” (LIGS) that recognizes and selects for specific aptamers of known cell surface proteins
[88][144]. The aptamer identified by LIGS has a higher specificity for the target ligand than the typical Cell-SELEX. Using LIGS, they identified an aptamer that binds IgM on target cells, named R1. Subsequently, they designed a truncated variant of R1 with higher affinity (R1.2) that specifically binds IgM-positive human B lymphoma BJAB cells at physiological temperature. Despite the high specificity of the LIGS-identified aptamers, their optimized and still unsatisfactory affinity prevented the use of the aptamers for clinical translational applications. Batool et al. formed high-affinity variants by dimerizing R1.2, and importantly, binding experiments using CRISPR/Cas9 on IgM knockout Burkitt’s lymphoma cells verified that dimeric R1.2 did not affect the original specificity
[89][145]. Thus, LIGS-identified aptamers can be re-optimized into dimeric aptamers with high affinity and specificity, which provides a new strategy for developing clinical diagnostic and therapeutic aptamers. LIGS provides a new screening method with higher efficiency and specificity than the previous hybrid screening of Protein-SELEX and Cell-SELEX, but the main problem is the low affinity, which may need to be optimized by introducing some external modifications.
Although natural killer (NK) cells are an integral part of the immune system, they lack cellular targeting vectors for targeted cancer immunotherapy under normal circumstances. Yang et al. anchored CD30-specific aptamers to the cell surface to generate aptamer-engineered NK cells (ApEn-NK), and targeted NK cells guided by aptamers triggered higher apoptosis/mortality in lymphoma cells, thus providing a promising new approach for NK cell-targeted immunotherapy
[90][146].
Parekh et al. identified an ssDNA aptamer (PS1NP) with high affinity (5 ± 0.5 nM) and specific binding to HL based on Cell-SELEX, which selectively detects HL cells in cell mixtures and even in complex biological media, demonstrating the potential of this aptamer to be used as a vector for targeted drug delivery and the potential of the aptamer to detect HL cells
[91][147].
In addition, many nanomaterial-aptamer complexes have also been designed for tumor diagnosis in lymphoma. Slyusarenko et al. created an AuNP aptamer sensor analysis system to quantify plasma CD30 small cell extracellular vesicles
[92][148]. The developed method can differentiate between healthy donors and cHL patients, providing a promising new method for monitoring cHL patients.
An ultrasensitive nanopore sensor based on aptamer recognition and signal amplification for label-free detection of aerosolized cancer cells was developed for the first time by Xi et al. By introducing robust, one-step enzymatic cycling amplification in the aerosol nanopore system, Ramos cells down to 5 cells in number can be identified in this assay
[93][149]. Fazlali et al. introduced new label-free electrogenerated chemiluminescence aptasensors for the detection of lymphoma cells by exploiting the binding of aptamers to CD20 on the surface of B-cell membranes and the accumulation of the positive charges of a nanocomposite on the negatively negative-charge charged of the aptamer phosphate backbone
[94][150]. The complex achieved enhanced sensitivity detection of B-lymphoma cells with a detection limit of 31 cells/mL. In addition, a novel aptamer biosensor for cancer cell determination based on ultrasensitive electrochemical detection has been reported
[95][151]. The cancer cells are first recognized and bound by the aptamer, and then the cell-aptamer mediates an alkaline phosphatase-catalyzed silver deposition reaction that can be detected by electrochemical detection. This method exhibits excellent selectivity in Ramos cell identification with detection limits as low as 10 cells. In conclusion, the above strategies demonstrate the promising potential application of aptamers in the early diagnosis of lymphoma.
As a hematologic tumor with various subtypes, lymphoma has the highest incidence among hematologic tumors, and therefore many aptamers have been created for targeting and diagnosing various subtypes of lymphoma, and these aptamers have contributed to the future treatment of various lymphomas. For example, aptamers targeting CD30 have been richly studied in the diagnosis and treatment of ALCL and cHL, and researchers have loaded these aptamers with chemotherapeutic drugs and siRNAs to achieve targeted therapy, resulting in many potential targeted therapeutic regimens. Many studies have combined CD20 aptamers with various materials to construct diagnostic tools for lymphoma with high sensitivity and selectivity. In conclusion for this part, aptamers have shown sufficient potential for application in the treatment of lymphoma, and further optimization is needed for further development.
4. Aptamers in Multiple Myeloma
A malignant disease of plasma cell (PC) origin, MM causes approximately 1% of all cancer-related deaths and 13% of hematological malignancies each year, mainly affecting older adults with a median age of 69 years
[96][152]. MM presents with abnormal proliferation and accumulation of bone marrow PC and excessive production of monoclonal immunoglobulins, often accompanied by multiple osteolytic lesions, hypercalcemia, anemia, and renal injury. Currently, the development of chemotherapy, autologous stem cell transplantation, proteasome inhibitors, immunomodulators, nucleic acid analogs
[97][98][99][153,154,155], and their combination therapies have effectively prolonged the survival time of new cases of MM, but for most patients, MM remains an incurable disease
[100][101][156,157]. As biomedicine continues to advance, aptamers show promising clinical prospects in the treatment of MM.
B-cell maturation antigen (BCMA) is present on the cell surface of late-stage normal B lymphocytes and is highly expressed in malignant plasma cells of MM patients, where it plays a role in cell survival
[102][103][158,159]. apt69.T is the first RNA aptamer targeting BCMA that inhibits the APRIL-dependent BCMA downstream NF-kB pathway and rapidly internalizes it in MM cells
[104][160]. In addition, the aptamer binds to microRNA-137 (miR-137) and anti-miR-222, showing a high potential to inhibit tumor cells.
Annexin A2 (ANXA2) is a member of a protein superfamily that is closely associated with malignant tumorigenesis, proliferation, invasion, and metastasis
[105][106][107][161,162,163] and is highly expressed in MM patients
[108][109][164,165]. Zhou’s group used the Protein-SELEX method to identify the ss DNA aptamer (wh6) that binds ANXA2 protein with high affinity and specifically binds MM cells
[110][166]. wh6 inhibits ANXA2-induced MM cell proliferation by disrupting the adhesion of MM cells to ANXA2.
Activation of the hepatocyte growth factor (HGF)/c-met pathway is closely related to the pathogenesis of MM, and therefore blocking this pathway is a new strategy for the treatment of MM. The DNA aptamer SL1 binds c-met with high specificity and affinity and inhibits HGF/c-met signaling in SNU-5 cells
[111][167]. Through the study of SL1 in MM, Yibin Zhang et al. found that SL1 could target c-met in MM and inhibit MM cell growth, migration, and adhesion in vitro
[112][168]. Furthermore, SL1 synergistically inhibited the proliferation of CD138
+ primary MM cells with bortezomib.
The transmembrane glycoprotein CD38, which is widely used to detect PC and diagnose MM, is a promising biomarker for targeting MM therapy. Wen et al. identified a CD38-specific ssDNA aptamer (#1S) that can target MM cells with high affinity
[113][169]. The #1S aptamer is loaded with Dox by non-covalent embedding, and the aptamer-drug complex is specifically delivered to MM cells, and Dox is efficiently released intracellularly under a unique pH control mechanism to achieve selective inhibition of MM tumors
[114][170].
Dai et al. used Cell-SELEX to identify ss DNA aptamer TY04, which binds specifically to MM cells and induces cell cycle arrest by upregulating CDK1 and cyclin B1 expression and downregulating γ-microtubulin expression, leading to cell growth inhibition
[115][171].
Cell adhesion-mediated drug resistance (CAM-DR) in bone marrow is the basis for MM cell dissemination and survival. In phase I/II clinical trials, data suggest that CXCL12 is a potent target for antagonizing CAM-DR in MM. The combination of NOX-A12 with bortezomib-dexamethasone resulted in the re-sensitization of MM cells to anti-myeloma drugs, suggesting that NOX-A12 could serve as an effective add-on agent to antagonize myeloma CAM-DR
[116][172].
In conclusion, there is an abundance of aptamers for multiple myeloma, some of which bind to surface proteins and block certain pathways to organize the proliferation, invasion, and migration of MM cells, while others work in combination with chemotherapeutic agents such as DOX. Although there are many aptamers related to MM, these studies did not dig deeper to promote the application of these aptamers in the diagnosis and treatment of MM. Perhaps researchers can consider combining these aptamers with various nanomaterials to build MM diagnostic reagents to facilitate early screening of MM patients to improve survival rates.