Wound healing is a public health concern worldwide, particularly in chronic wounds due to delayed healing and susceptibility to bacterial infection. Nanomaterials are widely used in wound healing treatments due to their unique properties associated with their size and very large surface-area-to-volume ratio compared to the same material in bulk. The properties of nanomaterials can be expanded and improved upon with the addition of honey and propolis, due to the presence of bioactive molecules such as polyphenols, flavonoids, peptides, and enzymes. These bionanomaterials can act at different stages of wound healing and through different mechanisms, including anti-inflammatory, antimicrobial, antioxidant, collagen synthesis stimulation, cell proliferation, and angiogenic effects.
- wound healing
- bionanomaterials
- honey
- propolis
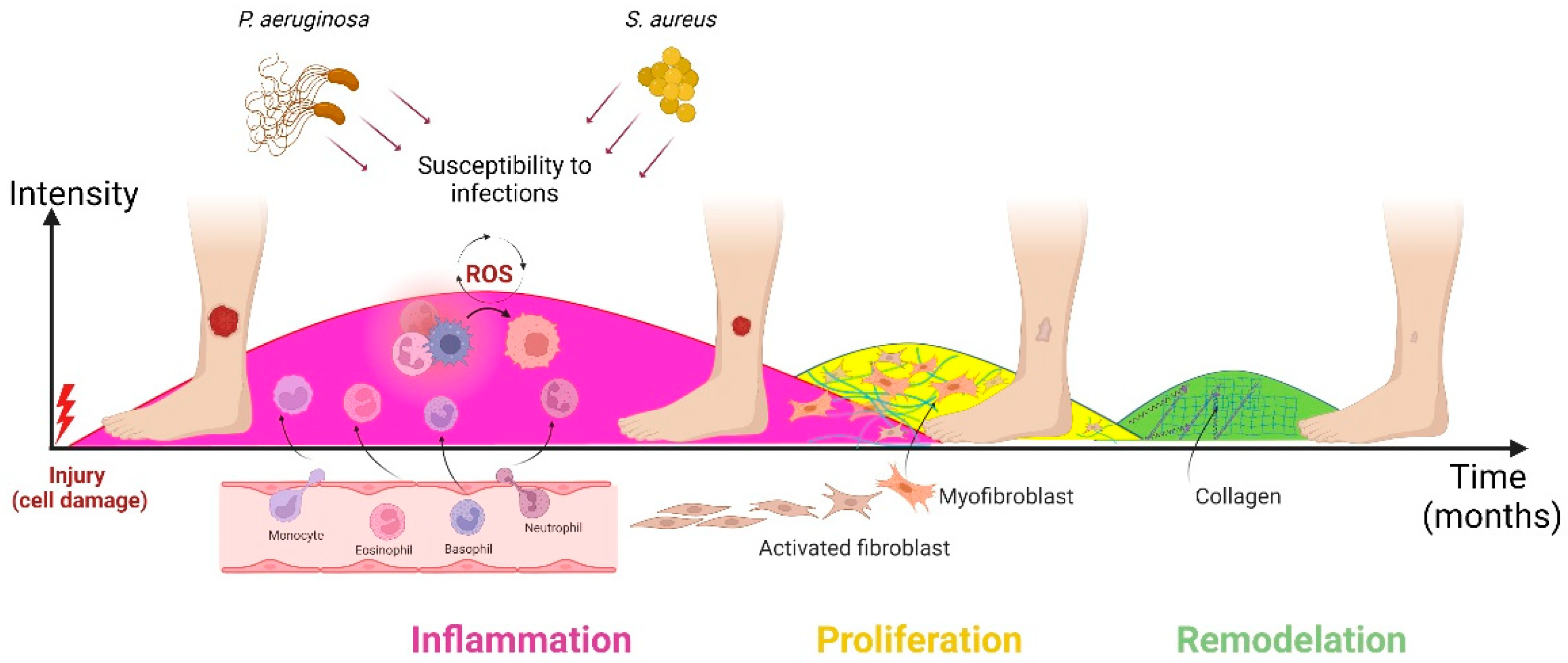
1. Wound Healing
2. Honey and Propolis Properties
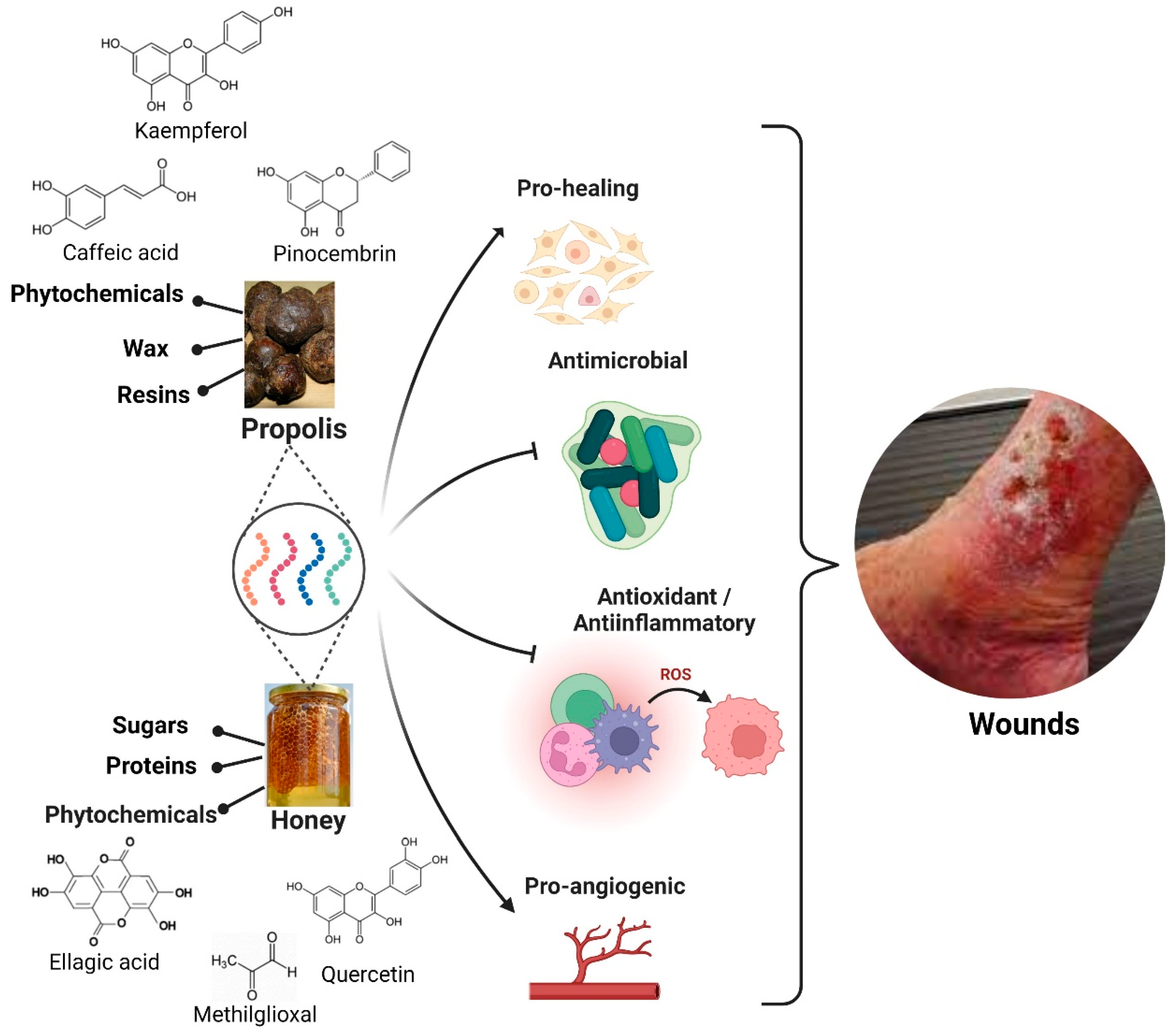
2.1. Honey
2.1.1. Antimicrobial Property
2.1.2. Anti-Inflammatory Property
2.1.3. Debriding Property
2.1.4. Tissue Regenerative Property
2.2. Propolis
2.2.1. Antimicrobial Properties
2.2.2. Antioxidant and Anti-Inflammatory Properties
2.2.3. Wound Healing Property
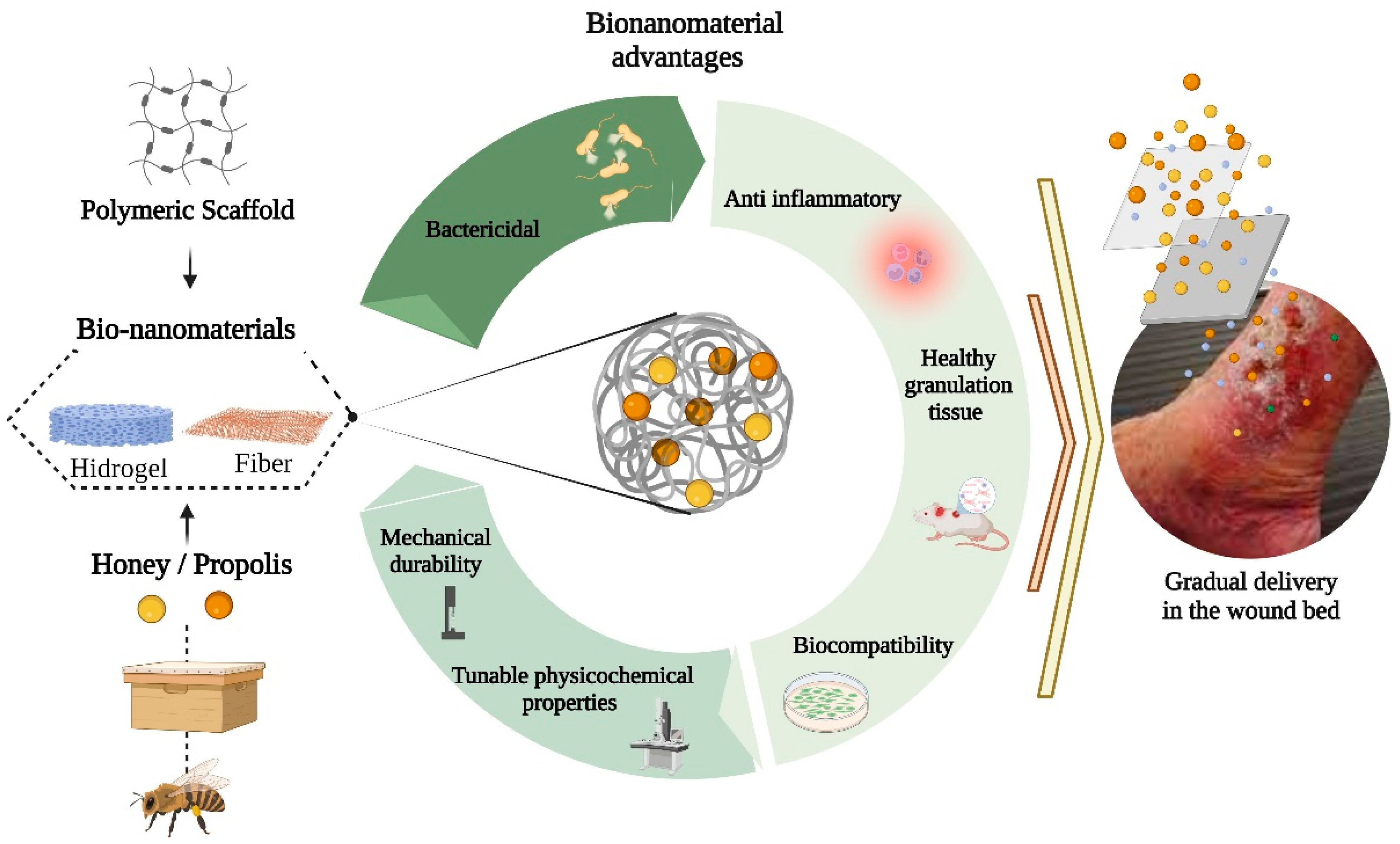
3. Bionanomaterials Based on Honey and Propolis
References
- Valencia-Gómez, L.E.; Martel-Estrada, S.A.; Vargas-Requena, C.L.; Rodriguez-González, C.A.; Olivas-Armendariz, I. Apósitos de polímeros naturales para regeneración de piel. Rev. Mex. Ing. Bioméd. 2016, 37, 235–249.
- Guo, S.; DiPietro, L.A. Critical review in oral biology & medicine: Factors affecting wound healing. J. Dent. Res. 2010, 89, 219–229.
- Martinotti, S.; Ranzato, E. Honey, Wound Repair and Regenerative Medicine. J. Funct. Biomater. 2018, 9, 34.
- Naskar, A.; Kim, K. Recent Advances in Nanomaterial-Based Wound-Healing Therapeutics. Pharmaceutics 2020, 12, 499.
- Eriksson, E.; Liu, P.Y.; Schultz, G.S.; Martins-Green, M.M.; Tanaka, R.; Weir, D.; Gould, L.J.; Armstrong, D.G.; Gibbons, G.W.; Wolcott, R.; et al. Chronic wounds: Treatment consensus. Wound Repair Regen. 2022, 30, 156–171.
- Zou, M.; Teng, Y.; Wu, J.; Liu, S.; Tang, X.; Jia, Y.; Chen, Z.-H.; Zhang, K.-W.; Sun, Z.-L.; Li, X.; et al. Fibroblasts: Heterogeneous Cells With Potential in Regenerative Therapy for Scarless Wound Healing. Front. Cell Dev. Biol. 2021, 9, 1–9.
- Jull, A.B.; Walker, N.; Deshpande, S. Honey as a topical treatment for wounds. Cochrane Database Syst. Rev. 2013, 2013, CD005083.
- Martinotti, S.; Ranzato, E. Propolis: A new frontier for wound healing? Burn. Trauma 2015, 3, 1–7.
- Viuda-Martos, M.; Ruiz-Navajas, Y.; Fernández-López, J.; Pérez-Álvarez, J.A. Functional Properties of Honey, Propolis, and Royal Jelly. J. Food Sci. 2008, 73, R117–R124.
- Singh, K.R.; Nayak, V.; Singh, R.P. Introduction to bionanomaterials: An overview. In Bionanomaterials; IOP Publishing: Bristol, UK, 2021; p. 1. ISBN 978-0-7503-3767-0.
- Alvarez-Suarez, J.M.; Gasparrini, M.; Forbes-Hernández, T.Y.; Mazzoni, L.; Giampieri, F. The composition and biological activity of honey: A focus on Manuka honey. Foods 2014, 3, 420–432.
- Balasooriya, E.R.; Jayasinghe, C.D.; Jayawardena, U.A.; Ruwanthika, R.W.D.; Mendis de Silva, R.; Udagama, P.V. Honey Mediated Green Synthesis of Nanoparticles: New Era of Safe Nanotechnology. J. Nanomater. 2017, 2017, 5919836.
- Maruhashi, E. Honey in Wound Healing. In Therapeutic Dressings and Wound Healing Applications; Wiley Online Library: New York, NY, USA, 2020; pp. 235–254.
- Samarghandian, S.; Farkhondeh, T.; Samini, F. Honey and Health: A Review of Recent Clinical Research. Pharmacogn. Res. 2017, 9, 121–127.
- Majtan, J.; Sojka, M.; Palenikova, H.; Bucekova, M.; Majtan, V. Vitamin C Enhances the Antibacterial Activity of Honey against Planktonic and Biofilm-Embedded Bacteria. Molecules 2020, 25, 992.
- Abou Zekry, S.S.; Abdellatif, A.; Azzazy, H.M.E. Fabrication of pomegranate/honey nanofibers for use as antibacterial wound dressings. Wound Med. 2020, 28, 100181.
- Mayba, J.N.; Gooderham, M.J. A Guide to Topical Vehicle Formulations. J. Cutan. Med. Surg. 2018, 22, 207–212.
- Karthik, T.; Rathinamoorthy, R. Sustainable biopolymers in textiles: An overview. Handb. Ecomater. 2019, 3, 1435–1460.
- Minden-Birkenmaier, B.A.; Bowlin, G.L. Honey-Based Templates in Wound Healing and Tissue Engineering. Bioengineering 2018, 5, 46.
- Hixon, K.R.; Klein, R.C.; Eberlin, C.T.; Linder, H.R.; Ona, W.J.; Gonzalez, H.; Sell, S.A. A Critical Review and Perspective of Honey in Tissue Engineering and Clinical Wound Healing. Adv. Wound Care 2019, 8, 403–415.
- Iacopetti, I.; Perazzi, A.; Martinello, T.; Gemignani, F.; Patruno, M. Hyaluronic acid, Manuka honey and Acemannan gel: Wound-specific applications for skin lesions. Res. Vet. Sci. 2020, 129, 82–89.
- Miguel, S.P.; Sequeira, R.S.; Moreira, A.F.; Cabral, C.S.D.; Mendonça, A.G.; Ferreira, P.; Correia, I.J. An overview of electrospun membranes loaded with bioactive molecules for improving the wound healing process. Eur. J. Pharm. Biopharm. 2019, 139, 1–22.
- Cushnie, T.P.T.; Lamb, A.J. Detection of galangin-induced cytoplasmic membrane damage in Staphylococcus aureus by measuring potassium loss. J. Ethnopharmacol. 2005, 101, 243–248.
- Cazander, G.; Ottelander, B.K.; Kamga, S.; Doomen, M.C.H.A.; Damen, T.H.C.; Well, A.M.E. Importance of Debriding and Wound Cleansing Agents in Wound Healing. In Therapeutic Dressings and Wound Healing Applications; Wiley: New York, NY, USA, 2020; pp. 59–89.
- Nina, N.; Quispe, C.; Jiménez-Aspee, F.; Theoduloz, C.; Feresín, G.E.; Lima, B.; Leiva, E.; Schmeda-Hirschmann, G. Antibacterial activity, antioxidant effect and chemical composition of propolis from the Región del Maule, central Chile. Molecules 2015, 20, 18144–18167.
- Velazquez, C.; Navarro, M.; Acosta, A.; Angulo, A.; Dominguez, Z.; Robles, R.; Robles-Zepeda, R.; Lugo, E.; Goycoolea, F.M.; Velazquez, E.F.; et al. Antibacterial and free-radical scavenging activities of Sonoran propolis. J. Appl. Microbiol. 2007, 103, 1747–1756.
- Ibrahim, M.E.E.-D.; Alqurashi, R.M. Anti-fungal and antioxidant properties of propolis (Bbee glue) extracts. Int. J. Food Microbiol. 2022, 361, 109463.
- Rossi, A.; Longo, R.; Russo, A.; Borrelli, F.; Sautebin, L. The role of the phenethyl ester of caffeic acid (CAPE) in the inhibition of rat lung cyclooxygenase activity by propolis. Fitoterapia 2002, 73, S30–S37.
- Toreti, V.C.; Sato, H.H.; Pastore, G.M.; Park, Y.K. Recent progress of propolis for its biological and chemical compositions and its botanical origin. Evid. Based. Complement. Alternat. Med. 2013, 2013, 697390.
- Olczyk, P.; Komosinska-Vassev, K.; Wisowski, G.; Mencner, L.; Stojko, J.; Kozma, E.M. Propolis modulates fibronectin expression in the matrix of thermal injury. Biomed Res. Int. 2014, 2014, 748101.
- Okur, M.E.; Bülbül, E.Ö.; Mutlu, G.; Eleftherıadou, K.; Karantas, I.D.; Okur, N.Ü.; Siafaka, P.I. An Updated Review for the Diabetic Wound Healing Systems. Curr. Drug Targets 2022, 23, 393–419.
- Kim, K.; Luu, Y.K.; Chang, C.; Fang, D.; Hsiao, B.S.; Chu, B.; Hadjiargyrou, M. Incorporation and controlled release of a hydrophilic antibiotic using poly (lactide-co-glycolide)-based electrospun nanofibrous scaffolds. J. Control. Release 2004, 98, 47–56.
- Bianchera, A.; Catanzano, O.; Boateng, J.; Elviri, L. The Place of Biomaterials in Wound Healing. In Therapeutic Dressings and Wound Healing Applications; Wiley: New York, NY, USA, 2020; pp. 337–366.
- Stoica, A.E.; Chircov, C.; Grumezescu, A.M. Nanomaterials for Wound Dressings: An Up-to-Date Overview. Molecules 2020, 25, 2699.
- Preem, L.; Kogermann, K. Electrospun Antimicrobial Wound Dressings: Novel Strategies to Fight Against Wound Infections. In Chronic Wounds, Wound Dressings and Wound Healing; Springer: Berlin/Heidelberg, Germany, 2018; pp. 213–253.
- Rajendran, N.K.; Kumar, S.S.D.; Houreld, N.N.; Abrahamse, H. A review on nanoparticle based treatment for wound healing. J. Drug Deliv. Sci. Technol. 2018, 44, 421–430.
- Jiao, Y.; Li, X.; Chen, J.; Li, C.; Liu, L.; Liu, X.; Wang, F.; Chen, G.; Wang, L. Constructing Nanoscale Topology on the Surface of Microfibers Inhibits Fibroblast Fibrosis. Adv. Fiber Mater. 2022, 4, 1219–1232.
- Sutjarittangtham, K.; Tragoolpua, Y.; Tunkasiri, T.; Chantawannakul, P.; Intatha, U.; Eitssayeam, S. The Preparation of Electrospun Fiber Mats Containing Propolis Extract/CL-CMS for Wound Dressing and Cytotoxicity, Antimicrobial, Anti-Herpes Simplex Virus. J. Comput. Theor. Nanosci. 2015, 12, 804–808.
- Farahani, M.; Shafiee, A. Wound Healing: From Passive to Smart Dressings. Adv. Healthc. Mater. 2021, 10, 2100477.
- Salama, A.; El-Sakhawy, M. Polysaccharides/propolis composite as promising materials with biomedical and packaging applications: A review. Biomass Convers. Biorefinery 2022, 1–11.
- Xu, Y.; Shi, G.; Tang, J.; Cheng, R.; Shen, X.; Gu, Y.; Wu, L.; Xi, K.; Zhao, Y.; Cui, W.; et al. ECM-inspired micro/nanofibers for modulating cell function and tissue generation. Sci. Adv. 2020, 6, 1–17.
