You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Conner Chen and Version 1 by Amin Gasmi.
Dental implants to replace lost teeth are a common dentistry practice nowadays. Titanium dental implants display a high success rate and improved safety profile. Nevertheless, there is an increasing peri-implantitis (PI), an inflammatory disease associated with polymicrobial infection that adversely affects the hard and soft tissues around the implant. Studies have demonstrated that oral microbiota (microorganisms residing in the oral cavity collectively known as oral microbiota) associated with periodontitis (PE) is involved in the infections related to PI, indicating a common link between PE and PI.
- dental implants
- inflammation
- peri-implantitis
1. Introduction
Dental issues are common health concerns that require immediate attention to relieve excruciating pain and prevent tooth deterioration [1]. There is a close association between oral and dental health, in which maintaining good oral hygiene directly links with better dental health [2]. According to an estimation, around 267 million people around the world are suffering from tooth loss [3]. The permanent tooth loss and alveolar bone defects can be managed by moveable dentures that are fixed in soft tissues and need to be changed over time. Now, dental implants have emerged as the preferred procedure for permanent tooth loss treatment and replaced the use of dentures. Biocompatibility and low cost of titanium dental implants make it the most often-used choice. Titanium is a bioinert substance that has little to no negative effects on the tissue it is adhered [4,5,6][4][5][6]. Despite all their usefulness, dental implants can sometimes cause infection. Improper implant placement or osseointegration failure can trigger the host inflammatory response and lead to the development of peri-implantitis (PI), which has become a growing concern in dentistry because of the lack of effective treatment strategies [7].
Generally, PI was defined as an inflammatory process affecting both soft and hard tissues surrounding an osseointegrated implant, associated with suppuration or bleeding after gentle probing, resulting in quick loss of supporting bone [8]. PI can limit dental implants’ clinical success and impose health and financial burdens on patients [9,10][9][10]. There are multiple causes of PI depending on the type of implant used and the overall health status of the patient such as poor oral hygiene, smoking, diabetes, history of periodontal disease, and previous implant loss [11,12][11][12]. According to Papi et al. [13], a higher risk of PI was observed in people with hyperglycemia.
Metabolic syndrome is a wide spectrum of health disorders, including hyperglycemia, dyslipidemia, visceral obesity, rheumatoid arthritis hypertension, etc. [14]. There is no doubt that the presence of metabolic disorders while studying implant engraftment in animals and patients complicates the process of survival of implants and increases the risk of PI relative to the healthy population [14,15,16][14][15][16]. In this regard, the frequency of PI increases strongly in older patients [17]. High life expectancy and reliability of modern implant dentistry are all factors that lead to the increased percentage of dental implants in elderly patients and risk an increase in the number of side effects, i.e., PI [13].
The inflammatory reactions in PI affect the surrounding tissues of the implant, where the high levels of pro-inflammatory cytokines such as interleukin 1beta (IL-1β) and tumor necrosis factor-alpha (TNF-α) promote bone resorption with subsequent adverse health consequences [18]. The colonized bacteria and their biofilms formation on the implants are the significant causes of peri-implant tissue inflammation due to their interactions with the host immune system. Streptococcus sanguinis, Streptococcus mitis, Streptococcus oralis and actinomyces are some common bacterial species that colonize at an early stage of biofilm formation while Porphyromonas gingivalis, Treponema denticola and Tannerella forsythia are some late colonizers [19,20,21][19][20][21]. With the recent increasing practice of dental implants, there are parallel increases in dental implant rejection and PI cases in dentistry practices. PI therapies using biomaterials such as fibers, gels, beads, and regeneration membranes to deliver antibiotics have been effectively applied in recent years.
The crucial mediators for PI are local tissue inflammation and increased oxidative stress [22]. These mediators are also the common determinations in most systemic metabolic conditions, such as type 2 diabetes mellitus and dyslipidemia [23]. As it is known, hormones coordinate different physiological processes in the body, including various metabolic conditions, growth, and development [24]. There is no doubt that bone physiology and the repair process for implant osseointegration strongly depend on the body’s hormonal status. Martin et al. [25] conducted the transcriptome-wide gene expression analysis and found the mechanisms of upregulation of genes in the endosomal-lysosomal and oxidative stress pathway in PI. They suggested that a crucial role in PI could be the receptor-driven responses to extracellular signals, such as implant-derived titanium particles. Through the transcriptome analysis, Cho et al. [23] found that smoking differentially affected PI and periodontitis (PE) in terms of host-defense mechanism impairment.
Several systemic metabolic diseases reduce the long-term success rate of dental implants. A 16-year follow-up study reported the success rate at only 82.9%, with around 5–8% of the failed osseointegration from PI [5]. Several reports indicate associations between chronic local dental inflammation, such as PE, and the increased risks of many systemic conditions, including metabolic diseases, cardiovascular diseases, cerebrovascular diseases, and neurodegenerative disorders [23,26,27,28,29][23][26][27][28][29]. The incidence of peri-implantitis patients with chronic PE is 4–5 times greater than those without a burdened periodontal history [9,30][9][30].
There are bi-directional relationships between local dental disease and systemic metabolic disorders, as shown in Figure 1. These relationships could be the crucial determinant for the success of the dental implant procedure and PI treatment. While planning and treating the local pathological oral conditions are necessary, the consideration and proper management of underlying metabolic disorders could determine the practice outcomes [5,22,31,32,33,34][5][22][31][32][33][34].
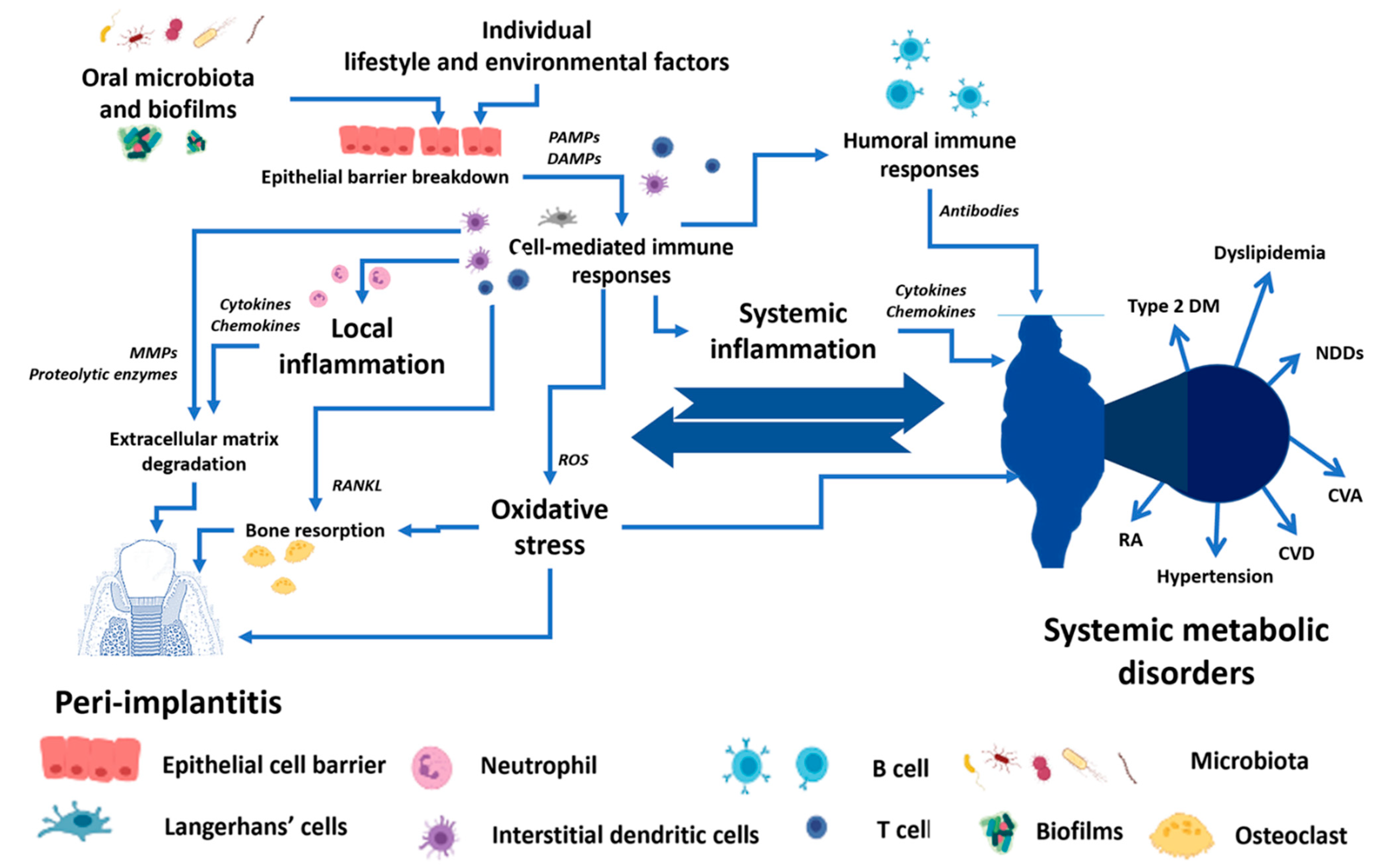
Figure 1. The conceptual framework of the bi-directional relationship between peri-implantitis and systemic metabolic disorders. PAMPs—Pathogen-associated molecular patterns, DAMPs—Damage-associated molecular patterns, MMPs—Matrix metalloproteinases, RANKL—Receptor activator of nuclear factor-κB ligand, ROS—Reactive oxygen species, Type 2 DM—Type 2 diabetes mellitus, NDDS—Neurodegenerative disorders, CVA—Cerebrovascular accident, CVD—Cardiovascular diseases, RA—Rheumatoid arthritis.
2. Association between Periodontitis and Peri-Implantitis
With rising dental problems, dental implants have increased considerably in recent times. Thus, the number of individuals suffering from PI has also increased. It has been observed that individuals suffering from PE which is gum disease and affects soft tissues show a greater risk of developing PI. In other words, PE is one of the major risk factors for developing PI [35]. Interestingly, the association between PE and PI is inconsistent. For instance, some studies show a direct association between the history of PE and the development of PI in later life [36,37][36][37]. However, other studies have shown that periodontally compromised patients are more prone to PI and implant loss [38,39][38][39]. Studies have demonstrated that oral microbiota (microorganisms residing in the oral cavity collectively known as oral microbiota) associated with PE is involved in the infections related to PI, indicating a common link between PE and PI. According to Norowski and Bumgardne [9], some pathogenic species of microorganisms associated with periodontitis, such as Aggregatibacter actinomycetemcomitans, Peptostreptococcus micros, Fusobacterium spp, Porphyromonas gingivalis, etc., are also closely associated with PI. It should be mentioned that PI is regarded as a more polymicrobial disease compared to PE [40,41][40][41]. Another reason for the association between PE and PI is an observation that dental implants cause more bone loss in individuals affected with PE [35,42][35][42]. Moreover, the microbiota associated with both disorders is similar to Treponema denticola, Tanarella forsythensi, and Prevotella intermedia, the common bacterial species in both dental disorders. However, recent studies have shown that the core microbiota associated with PE and PI is not necessarily the same, and a distinct microbial environment is present in both diseases [35,42,43][35][42][43]. It is important to highlight that both PE and PI show different features at the histological level. For example, in a study by Carcuac et al., 40 patients with PE and 40 patients with PI were recruited to understand the histological and immunological differences. It was observed that PI lesions were larger in size, twice in comparison with PE, and contained a higher number and density of key immune system cells positive for cluster of differentiation 138 (CD138), CD68-, and myeloperoxidase (MPO) markers. Moreover, the infiltration of the immune system cells is more pronounced in PI than in PE. According to Yang et al. [44] and Avdeev et al. [45], modulating the proper immune microenvironment could promote periodontal regeneration. The difference between PE and PI was also observed in the type of immune system cells infiltrated in the dental tissue. In PE, the primary infiltrating cells were lymphocytes and plasma cells, while in PI, inflammatory macrophages and neutrophils were the dominant cells [46]. The bone morphogenetic protein (BMP)/retinoic acid inducible neural specific 3 (BRINP3) gene has been linked with an aggressive form of PE. However, a recent study by Casado et al. has established that PI is also associated with BRINP3 polymorphic variant rs1342913, but the association is independent of PE. Thus, based on the available scientific evidence, it can be concluded that PE is a risk factor for PI, but both are not identical at histological and immunological levels [47]. Recently, Martin et al. [25] concluded that three core clinical features suggest that PI is very dissimilar to PE: (1) the bone destruction in PI is more significant than observed in PE; (2) clinical studies reported implant-derived titanium particles as being substantially increased in the peri-implant microenvironment in PI versus health; (3) mechanical and antimicrobial interventions that are very effective against PE have limited influence against PI which is regarded to a leading role of persistent titanium particles in PI. For instance, Safioti et al. [48] monitored the increased levels of dissolved titanium in PI.References
- Institute of Medicine (US) Division of Health Care Services. Chapter 3, Epidemiology and Prevention of Dental Diseases. In Public Policy Options for Better Dental Health: Report of a Study, Services; National Academies Press (US): Washington, DC, USA, 1980.
- Charalampakis, G.; Belibasakis, G.N. Microbiome of peri-implant infections: Lessons from conventional, molecular and metagenomic analyses. Virulence 2015, 6, 183–187.
- Silva, R.C.; Agrelli, A.; Andrade, A.N.; Mendes-Marques, C.L.; Arruda, I.R.; Santos, L.R.; Vasconcelos, N.F.; Machado, G. Titanium Dental Implants: An Overview of Applied Nanobiotechnology to Improve Biocompatibility and Prevent Infections. Materials 2022, 15, 3150.
- Guillaume, B. Dental implants: A review. Morphol. Bull. De L’association Des Anat. 2016, 100, 189–198.
- Prathapachandran, J.; Suresh, N. Management of peri-implantitis. Dent. Res. J. 2012, 9, 516.
- Razak, P.A.; Richard, K.J.; Thankachan, R.P.; Hafiz, K.A.; Kumar, K.N.; Sameer, K. Geriatric oral health: A review article. J. Int. Oral Health JIOH 2014, 6, 110.
- Fretwurst, T.; Nelson, K.; Tarnow, D.; Wang, H.-L.; Giannobile, W.V. Is Metal Particle release associated with peri-implant bone destruction? an emerging concept. J. Dent. Res. 2017, 97, 002203451774056.
- Albrektsson, T.; Isidor, F. Consensus Report of Session IV. In Proceedings of the First European Workshop on Periodontology; Lang, N.P., Karring, T., Eds.; Quintessence Publishing: London, UK, 1994; pp. 365–369.
- Norowski, P.A., Jr.; Bumgardner, J.D. Biomaterial and antibiotic strategies for peri-implantitis: A review. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 530–543.
- Bumgardner, J.D.; Adatrow, P.; Haggard, W.O.; Norowski, P.A. Emerging antibacterial biomaterial strategies for the prevention of peri-implant inflammatory diseases. Int. J. Oral Maxillofac. Implant. 2011, 26, 553–560.
- Toledano, M.; Osorio, M.T.; Vallecillo-Rivas, M.; Toledano-Osorio, M.; Rodriguez-Archilla, A.; Toledano, R.; Osorio, R. Efficacy of local antibiotic therapy in the treatment of peri-implantitis: A systematic review and meta-analysis. J. Dent. 2021, 113, 103790.
- Kormas, I.; Pedercini, C.; Pedercini, A.; Raptopoulos, M.; Alassy, H.; Wolff, L.F. Peri-Implant Diseases: Diagnosis, Clinical, Histological, Microbiological Characteristics and Treatment Strategies. A Narrative Review. Antibiotics 2020, 9, 835.
- Papi, P.; Letizia, C.; Pilloni, A.; Petramala, L.; Saracino, V.; Rosella, D.; Pompa, G. Peri-implant diseases and metabolic syndrome components: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 866–875.
- De Angelis, F.; Papi, P.; Mencio, F.; Rosella, D.; Di Carlo, S.; Pompa, G. Implant survival and success rates in patients with risk factors: Results from a long-term retrospective study with a 10 to 18 years follow-up. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 433–437.
- Coelho, P.G.; Pippenger, B.; Tovar, N.; Koopmans, S.J.; Plana, N.M.; Graves, D.T.; Engebretson, S.; van Beusekom, H.M.M.; Oliveira, P.; Dard, M. Effect of Obesity or Metabolic Syndrome and Diabetes on Osseointegration of Dental Implants in a Miniature Swine Model: A Pilot Study. J. Oral Maxillofac. Surg. 2018, 76, 1677–1687.
- de Oliveira, P.; Bonfante, E.A.; Bergamo, E.T.P.; de Souza, S.L.S.; Riella, L.; Torroni, A.; Benalcazar Jalkh, E.B.; Witek, L.; Lopez, C.D.; Zambuzzi, W.F.; et al. Obesity/Metabolic Syndrome and Diabetes Mellitus on Peri-implantitis. Trends Endocrinol. Metab. 2020, 31, 596–610.
- Compton, S.M.; Clark, D.; Chan, S.; Kuc, I.; Wubie, B.A.; Levin, L. Dental Implants in the Elderly Population: A Long-Term Follow-up. Int. J. Oral Maxillofac. Implants 2017, 32, 164–170.
- Al-Aali, K.A.; Alrabiah, M.; ArRejaie, A.S.; Abduljabbar, T.; Vohra, F.; Akram, Z. Peri-implant parameters, tumor necrosis factor-alpha, and interleukin-1 beta levels in vaping individuals. Clin. Implant. Dent. Relat. Res. 2018, 20, 410–415.
- Kumar, P.S.; Mason, M.R.; Brooker, M.R.; O’Brien, K. Pyrosequencing reveals unique microbial signatures associated with healthy and failing dental implants. J. Clin. Periodontol. 2012, 39, 425–433.
- Quirynen, M.; De Soete, M.; Van Steenberghe, D. Infectious risks for oral implants: A review of the literature. Clin. Oral Implant. Res. Rev. Artic. 2002, 13, 1–19.
- Berglundh, T.; Jepsen, S.; Stadlinger, B.; Terheyden, H. Peri-implantitis and its prevention. Clin. Oral Implant. Res. 2019, 30, 150–155.
- Frizzera, F.; Oliveira, G.J.P.L.d.; Shibli, J.A.; Moraes, K.C.d.; Marcantonio, E.B.; Marcantonio Junior, E. Treatment of peri-implant soft tissue defects: A narrative review. Braz. Oral Res. 2019.
- Winning, L.; Linden, G.J. Periodontitis and systemic disease. BDJ Team 2015, 2, 15163.
- Yi, M.; Yin, Y.; Sun, J.; Wang, Z.; Tang, Q.; Yang, C. Hormone and implant osseointegration: Elaboration of the relationship among function, preclinical, and clinical practice. Front. Mol. Biosci. 2022, 9, 965753.
- Martin, A.; Zhou, P.; Singh, B.B.; Kotsakis, G.A. Transcriptome-wide Gene Expression Analysis in Peri-implantitis Reveals Candidate Cellular Pathways. JDR Clin. Trans. Res. 2022, 7, 415–424.
- Suh, J.S.; Kim, S.; Boström, K.I.; Wang, C.-Y.; Kim, R.H.; Park, N.-H. Periodontitis-induced systemic inflammation exacerbates atherosclerosis partly via endothelial–mesenchymal transition in mice. Int. J. Oral Sci. 2019, 11, 21.
- Nascimento, P.C.; Castro, M.M.L.; Magno, M.B.; Almeida, A.P.C.P.S.C.; Fagundes, N.C.F.; Maia, L.C.; Lima, R.R. Association Between Periodontitis and Cognitive Impairment in Adults: A Systematic Review. Front. Neurol. 2019, 10, 323.
- Heikkilä, P.; But, A.; Sorsa, T.; Haukka, J. Periodontitis and cancer mortality: Register-based cohort study of 68,273 adults in 10-year follow-up. Int. J. Cancer 2018, 142, 2244–2253.
- D’Aiuto, F.; Gkranias, N.; Bhowruth, D.; Khan, T.; Orlandi, M.; Suvan, J.; Masi, S.; Tsakos, G.; Hurel, S.; Hingorani, A.D.; et al. Systemic effects of periodontitis treatment in patients with type 2 diabetes: A 12 month, single-centre, investigator-masked, randomised trial. Lancet Diabetes Endocrinol. 2018, 6, 954–965.
- Karoussis, I.; Salvi, G.; Heitz-Mayfield, L.; Brägger, U.; Hammerle, C.; Lang, N. Long-term implant prognosis in patients with and without a history of chronic periodontitis: A 10-year prospective cohort study of the ITI® Dental Implant System. Clin. Oral Implant. Res. 2003, 14, 329–339.
- Khammissa, R.; Feller, L.; Meyerov, R.; Lemmer, J. Peri-implant mucositis and periimplantitis: Bacterial infection. S. Afr. Dent. J. 2012, 67, 70–74.
- Van Winkelhoff, A.J.; Goené, R.J.; Benschop, C.; Folmer, T. Early colonization of dental implants by putative periodontal pathogens in partially edentulous patients. Clin. Oral Implant. Res. 2000, 11, 511–520.
- Tugnait, A.; Carmichael, F. Use of radiographs in the diagnosis of periodontal disease. Dent. Update 2005, 32, 536–542.
- Serino, G.; Wada, M. Non-surgical mechanical treatment of peri-implant mucositis: The effect of sub-mucosal mechanical instrumentation following supra-mucosal plaque removal. A 7-month prospective single cohort study. Eur. J. Oral Implantol. 2018, 11, 455–466.
- Khalil, D.; Hultin, M. Peri-implantitis Microbiota. In An Update of Dental Implantology and Biomaterial; IntechOpen: Rijeka, Croatia, 2018.
- Ravidà, A.; Rodriguez, M.V.; Saleh, M.H.; Galli, M.; Qazi, M.; Troiano, G.; Wang, H.L.; Moreno, P.G. The correlation between history of periodontitis according to staging and grading and the prevalence/severity of peri-implantitis in patients enrolled in maintenance therapy. J. Periodontol. 2021, 92, 1522–1535.
- Renvert, S.; Persson, G.R. Periodontitis as a potential risk factor for peri-implantitis. J. Clin. Periodontol. 2009, 36, 9–14.
- Pandolfi, A.; Rinaldo, F.; Pasqualotto, D.; Sorrentino, F.; La Torre, G.; Guerra, F. A retrospective cohort study on peri-implant complications in implants up to 10 years of functional loading in periodontally compromised patients. J. Periodontol. 2020, 91, 995–1002.
- Mombelli, A.; Müller, N.; Cionca, N. The epidemiology of peri-implantitis. Clin. Oral Implant. Res. 2012, 23, 67–76.
- Lasserre, J.; Brecx, M.; Toma, S. Oral Microbes, Biofilms and Their Role in Periodontal and Peri-Implant Diseases. Materials 2018, 11, 1802.
- de Avila, E.D.; van Oirschot, B.A.; van den Beucken, J. Biomaterial-based possibilities for managing peri-implantitis. J. Periodontal. Res. 2020, 55, 165–173.
- Gandra, R.A.; Fernandes, D.G.F.; Silva, I.L.; Zenóbio, E.G. Variáveis relacionadas à doença periodontal prévia e perda óssea peri-implantar. RGO-Rev. Gaúcha De Odontol. 2019, 67, e20190042.
- Ferreira, S.D.; Martins, C.C.; Amaral, S.A.; Vieira, T.R.; Albuquerque, B.N.; Cota, L.O.M.; Lima, R.P.E.; Costa, F.O. Periodontitis as a risk factor for peri-implantitis: Systematic review and meta-analysis of observational studies. J. Dent. 2018, 79, 1–10.
- Yang, B.; Pang, X.; Li, Z.; Chen, Z.; Wang, Y. Immunomodulation in the Treatment of Periodontitis: Progress and Perspectives. Front. Immunol. 2021, 12, 781378.
- Avdeev, O.; Drevnitska, R.; Boykiv, A.; Vydoinyk, O. Condition of fagocytosis of experimental animals with periodontitis due to modified reactivity. Wiad. Lek. 2019, 72, 401–404.
- Carcuac, O.; Berglundh, T. Composition of human peri-implantitis and periodontitis lesions. J. Dent. Res. 2014, 93, 1083–1088.
- Casado, P.L.; Aguiar, D.P.; Costa, L.C.; Fonseca, M.A.; Vieira, T.C.; Alvim-Pereira, C.C.; Alvim-Pereira, F.; Deeley, K.; Granjeiro, J.M.; Trevilatto, P.C. Different contribution of BRINP3 gene in chronic periodontitis and peri-implantitis: A cross-sectional study. BMC Oral Health 2015, 15, 33.
- Safioti, L.; Kotsakis, G.; Pozhitkov, A.; Chung, W.; Daubert, D.M. Increased Levels of Dissolved Titanium are Associated With Peri-Implantitis—A Case-Control Study. J. Periodontol. 2016, 88, 21.
More
