Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Rui Henrique and Version 2 by Catherine Yang.
Renal cell carcinoma (RCC) is the most common form of kidney cancer, characterized by silent progression at early stages, heterogeneous behavior and resistance to chemotherapy and radiotherapy. Circulating tumor cells (CTC) are rare cancer cells that are released from the primary tumor site, nodal or systemic metastases to the bloodstream. Thus, CTCs play a key role in the metastatic cascade, eventually becoming the precursors of metastasis in distant sites.
- circulating tumor cells
- renal cell carcinoma
- detection
1. Early Detection of Metastasis
The scientific community has been focused on the ability of CTCs in early prediction of metastasis. In this regard, a study evaluated the relationship between the CTC-positive status of patients with mRCC and the expression of blood tumor markers, namely cytokeratin 19 (CK19), endoglin (CD105) and CD146 [1][89]. The measurements were taken at different time points, namely before and after surgical treatment. Interestingly, a statistically significant difference in the expression of CK19 and CD105 markers was observed in CTC-positive, compared to CTC-negative patients between measurements taken one day before and one week after surgery. The same was not observed for CD146. Another statistically significant difference was depicted for expression of the three markers between measurements taken one day before and one month after surgery. Thus, it was hypothesized that those markers, when in the presence of CTCs, may help in early metastases detection and prognosis assessment [1] (Figure 1)[89].
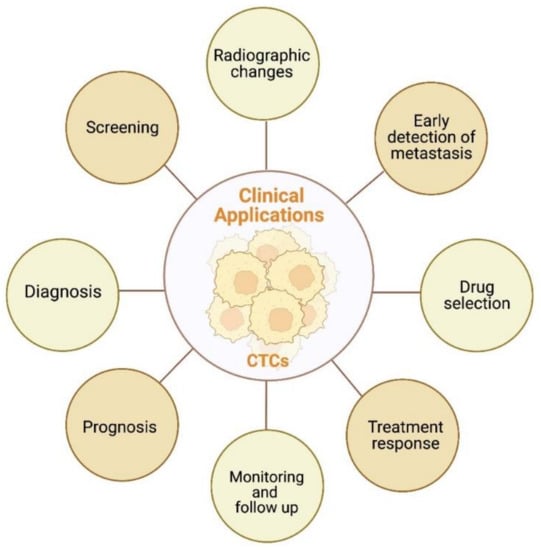
Figure 13.
Schematic representation of potential clinical applications of CTCs in RCC. Created with BioRender.com.
During the metastatic cascade, CTCs interact with various blood cells, including platelets and inflammatory cells. In 2022, a study evaluated the prognostic impact of this set of cells in 82 RCC patients [2][36]. Together, the presence of mesenchymal CTCs, monocyte/neutrophil ratio (MNR) and staging demonstrated prognostic potential, allowing metastization after surgical treatment to be predicted [2][36]. In the same year, another study, enrolling 1176 nephrectomized patients, emphasized the relevance of long-term follow-up to detect early recurrence, as it seems to be a frequent event. In fact, about one-fifth of patients with stage I RCC experienced late recurrence (after 20 years of follow-up), and this figure was higher in advanced stages [3][90]. Intriguingly, in a retrospective study of 464 nephrectomized patients for non-metastatic RCC, shorter survival (for both cancer-specific (CSS) and overall survival (OS)) was observed in patients with local recurrence and absence of distant metastasis, thus reflecting a worse prognosis [4][91].
2. Prognostic Value
As for the prognostic value of CTCs, it is known that their presence in the bloodstream is associated with poorer prognosis [5][92]. In this context, Klezl et al. investigated 186 patients with RCC, assessing the presence of CTCs before and after surgery as well as during follow-up, using mitochondrial activity to infer about their viability. They found CTCs in 86.7% of the samples and noted that detection of CTCs was associated with tumor size and that it was more likely to occur when the tumor was growing. Tumor size was also associated with the presence of metastases in lymph nodes and distant sites [6][93]. In another study, the numbers of RCC-CTCs before surgery were found to be significantly associated with tumor size but not other clinicopathological features [7][94]. Moreover, there was a significant positive association between high Ki-67 expression (a proliferation indicator) and the numbers of CTCs before surgery, especially for a number greater than or equal to five CTCs. Thus, the presence of ≥5 CTCs was proposed as a diagnostic and prognostic parameter for RCC. Then, it was concluded that the surgical strategy, namely nephrectomy, is responsible for changing the levels of CTCs, directly leading to a postoperative reduction in their number in RCC patients [7][94].
In the same perspective, to evaluate the impact of surgical technique on CTC numbers, Haga et al. conducted a study that included 60 RCC patients [8][95]. Patients who underwent open radical nephrectomy disclosed significantly higher CTC numbers after surgery, as well as significant perioperative change in CTCs compared to patients who underwent laparoscopic or partial open surgery. In particular, the CTC numbers after surgery were significantly associated with larger tumor masses. Regarding preoperative CTC number, a significant association was found between tumor diameter and TNM staging, with the highest numbers seen in advanced disease stages. Finally, the authors pointed out the importance of surgical technique and tumor diameter in the spread of CTCs, which may promote early postoperative metastasis, thus affecting prognosis [8][95]. Another study pointed out a significant association between the presence in the bloodstream of six or more CTCs after surgery and RCC progression [9][96]. Moreover, the presence in circulation of mesenchymal CTCs and CTC-WBCs post-surgery correlated with higher likelihood of recurrence and metastasis. Hence, these three CTC subtypes were highlighted as independent prognostic factors of worse clinical outcome and shorter PFS [9][96].
Recently, an observational study looked at the ability of CTCs to predict invasion of the inferior vena cava by RCC. It was then hypothesized that the total CTC count as well as the CTC subtype could be predictive indicators of that invasion, having potential to influence RCC prognosis [10][80].
In a prospective multicenter study including 195 patients with mRCC, CTC counts were obtained and compared according to patient outcome [11][62]. On the one hand, an association was initially depicted (independently of the International Metastatic RCC Database Consortium (IMDC) score) between the presence of three or more CTCs, and on the other, reduced PFS (median 8.3 months vs. 32.6 months) and OS (13.8 months vs. 52.8 months). Hence, a cut-off value of three CTCs, using the Cell Search system, was suggested as having prognostic value. Furthermore, a correlation between higher propensity to CTC counts less than three, and bone involvement was depicted. Interestingly, the same was not found for brain and liver involvement [11][62]. In another study, a significant association between the presence of CTCs and shorter PFS was reported. Nonetheless, the same was not verified for OS. Thus, it was suggested that the positivity of CTCs at baseline may constitute a relevant prognostic factor in mRCC patients for PFS only [12][79]. Intriguingly, a study indicated an absence of correlation between the initial numbers of CTCs and the likelihood of RCC recurrence or metastization. Instead, it seems that it is the dynamic change in CTCs (particularly mesenchymal CTCs and those expressing Beclin1) that correlates with recurrence or metastasis. Still, several limitations of the study hamper the conclusions [13][72].
Different CTC subtypes appear to influence cancer progression in RCC patients. This is illustrated by a recent study in ccRCC patients, in which a significant association between the enumeration of CTCs and positive CK marker expression, and disease progression was depicted. Surprisingly, the same was not disclosed for CTC counts with unique expression of CAXII, a kidney cancer-specific capture antibody [14][64].
In addition to CTCs, CTC-WBC clusters have also been the subject of intense research. In a study involving 163 patients with RCC, the prognostic role of both CTCs and CTC-WBC clusters was evaluated [15][70]. High total CTC counts and the presence of CTC-WBC clusters disclosed prognostic impact for MFS, the latter being more crucial for a worse outcome. Importantly, tumor mass diameter together with high total CTC count demonstrated value as prognostic indicators for OS, enabling better outcome prediction in RCC patients [15][70].
Karyotype analysis in renal CTCs has sparked increasing interest among investigators. An interesting finding in terms of clinical application was the recent indication of tetraploidy of chromosome 8 as potentially prognostic in RCC. This was suggested by the significantly higher presence of tetraploid CTCs in the advanced stage of the disease (T4 stage) compared to the other stages [16][65]. Interestingly, epigenetic factors, such as DNA methylation, have also been investigated as ccRCC prognostic biomarkers. Indeed, their combination with clinicopathological features seems to provide a more accurate prognostication in patients with localized ccRCC [17][97]. Methylated DNA has also been recently characterized in CTCs from other urological cancers, such as prostate cancer [18][98].
Importantly, patient characteristics seem to impact CTC enumeration. A recent study demonstrated that age of RCC patients may interfere with CTC numbers, being negatively associated with survival. Moreover, the number of CTCs may be affected by the expression of Beclin1 in mesenchymal and epithelial RCC-CTC, which decreases its production. Intriguingly, in a study that evaluated Beclin1 expression in CTCs and CTC count, no differences in OS and disease-free survival (DFS) were apparent [19][71].
Besides the potential prognostic value of CTCs, other biomarkers have also been tested, and circulating tumor DNA (ctDNA) has been shown to be a worthy competitor [20][99]. In fact, higher ctDNA levels have been found in disseminated disease (as opposed to localized disease), and its detection in blood samples may be associated with worse clinical outcome (i.e., higher risk of death and lower overall survival). Moreover, variations in ctDNA levels along disease progression may provide valuable information for monitoring treatment response and follow-up of RCC patients. Interestingly, the detection of genetic aberrations in ctDNA during cancer treatment may be useful for deciphering mechanisms of resistance to therapy. However, downsides of ctDNA include the low levels in the bloodstream of RCC patients. Furthermore, the paucity of studies (and with small sample size) in RCC coupled with the low sensitivity of ctDNA detection methods used mean that there is still a long way to go regarding this biomarker, making CTCs more attractive [20][99].
3. Prediction of Response to Therapy
A study conducted by Basso et al. evaluated the response to TKI treatment in mRCC patients by CTC enumeration [11][62]. After approximately 10 months of treatment, with measurement of CTCs at various time points, there was no significant association between CTC numbers (either at baseline or in sequence, using cutoff values of one/two/three/four/five CTCs) and response to treatment. Moreover, regarding radiological evolution of mRCC patients, it was not possible to predict radiological outcome based on CTC numbers (either at baseline or dynamic) [11][62]. Nonetheless, contrasting results were disclosed in another investigation that indicated a significant predictive role for the presence of CTCs at baseline in weaker response to TKI treatment in mRCC patients. Thus, CTCs may be useful as predictive biomarkers of response to TKI therapy in mRCC [12][79]. More recently, another study indicated CTC counts as a pharmacodynamic biomarker, going beyond treatment with TKIs [14][64].
Promising results have also been recently reported concerning the therapeutic response, namely, a significant association with PD-L1 and HLA-I expression in CTCs. CTCs with positive expression for CAXII and PD-L1 were associated with response to immune-checkpoint inhibitors (ICI) treatment, whereas CTCs with positive expression for CAX II and HLA-I were significantly associated with response to TKI therapy. The same was not observed for CTCs with positive CK expression, and it was suggested that the various subpopulations of CTCs influence RCC patient response to therapy [14][64].
In another study including 155 patients with various types of cancer, PD-L1 expression in CTCs was proposed as a possible biomarker for response to immunotherapy [21][100]. In fact, elevated PD-L1 expression in CTCs was found to be both predictive (with higher response rate) and prognostic (higher progression-free survival and overall survival) in advanced stage cancers under immune checkpoint inhibitor therapy [21][100]. In particular, during treatment of ccRCC patients with PD-L1 inhibitors, dynamic changes in CTCs’ PD-L1 expression may have prognostic value, and CTC counts may play a role in treatment monitoring [22][101]. Concordant results were found in urothelial carcinoma, and the presence of CTCs expressing PD-L1 at baseline may further allow real-time selection of the most suitable candidates for immunotherapy [23][102]. Besides the role of PD-L1, other immunosuppressive checkpoints, such as TIM-3 and LAG3, were also pointed out as useful markers in the context of immunotherapy for ccRCC. Indeed, blocking these checkpoints may favor the prognosis of ccRCC patients, since depletion of immune cells, namely CD8+ cells, was associated with worse clinical outcome in a recent report based on transcriptomic analysis [24][37].
Besides the role of predicting response to therapy, CTC counts may be used to monitor therapy over time in patients with mRCC [25][103]. This is well illustrated by a 2022 longitudinal study involving 104 patients with mRCC, which reported a lower overall survival for patients who submitted to immunotherapy, with a trend for a higher number of CTCs over time [26][104]. In addition, a worse outcome was found in patients with a trend for higher values of the HLA I to PD-L1 ratio. Thus, it was pointed out that the change in CTC count and in the molecular profile of CTCs along treatment may serve as biomarkers for monitoring treatment response [26][104].
4. Screening
To date, scarce research has been performed on the potential role of RCC-CTCs in screening. In fact, one of the few existing studies has focused on combining CTCs with polymorphisms of cancer susceptibility genes, namely XPC A2815C and XRCC1 G1196A [27][81]. Surprisingly, this combination proved to be highly sensitive (92.86% positivity) in detecting genitourinary cancer patients. Furthermore, a direct relationship was established between CTC count and cancer progression, in which RCC was included. Therefore, the application of this panel in the screening and monitoring of genitourinary cancers, such as RCC, has been suggested [27][81].
5. Monitoring and Follow-Up
Ultimately, it has been proposed that the presence of high numbers of RCC-CTCs before surgical treatment (≥5 CTCs) should motivate a stricter monitoring and longer-term follow-up among these RCC patients [8][95].
6. Radiological Impact
In a recent study, an association between changes in numbers of different CTC subpopulations and radiological tumoral findings was reported. Particularly, variations in CTC CK+ numbers were related to radiographic findings of tumor mass growth, this growth being more subtle when CTC numbers varied little. Additionally, after ablative therapy with radiation, an increased number of CTCs was found in circulation, and the authors suggested as an explanation the prompt effusion of these cells after the therapeutic intervention [14][64].
