Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Norhafiza Mat Lazim and Version 2 by Rita Xu.
At this juncture, autofluorescence and narrow-band imaging have resurfaced in the medicine arena in parallel with current technology advancement. The emergence of newly developed optical instrumentation in addition to the discovery of new fluorescence biomolecules have contributed to a refined management of diseases and tumors, especially in the management of upper aerodigestive tract tumors. The advancement in multispectral imaging and micro-endoscopy has also escalated the trends further in the setting of the management of this tumor, in order to gain not only the best treatment outcomes but also facilitate early tumor diagnosis.
- head and neck cancers
- autofluorescence
- narrow band imaging
1. Introduction
Head and neck tumors represent 5% of all neoplasms worldwide and manifest differently based on the patient demographic (e.g., HPV status) and the anatomical site which harbors the neoplasm (e.g., oral tongue versus tonsils). The majority of head and neck tumors are squamous cell carcinoma, which mostly arise in the upper aerodigestive tract mucosa, namely the oral cavity, pharynx, larynx, nasal cavity, paranasal sinus and nasopharynx [1]. The majority of upper aerodigestive tract tumor patients present at late stage, where the treatment is more challenging. This is compounded by multiple patient factors, as well as logistic factors that affect the treatment outcomes. Most patients who come with late-stage tumors have poor prognosis, especially in the presence of bulky tumors and distant metastasis. Despite poor prognosis, early screening, early treatment and a well-planned follow up scheme can lead to overall improved survival and quality of life of these patients.
Generally, for head and neck malignancy, a significant number of patients presented with neck recurrence, as well as multiple systemic metastases, despite multimodality treatment, whereas a minority of patients had second primaries. The contributing factors for these poor outcomes include late diagnosis during a primary tumor assessment and characteristic tumor biology, as well as a high prevalence of second primary tumors and recurrent tumors in patients who already have received treatment for head and neck carcinoma [2][3][2,3]. In addition, the prognosis is also strongly related to early screening, availability of accurate diagnostic procedures and adequate surgical resection margin of any given tumors [4][5][6][4,5,6]. This is vital in order to improve patient treatment outcomes and prognosis. A wide availability of effective screening methods and up-to-date and highly sensitive diagnostic procedures will ultimately improve head and neck carcinoma patients’ subsequent management.
Of note, in parallel with recent advancement in technology, the latest imaging techniques which are commonly applied for detecting cancer in any head and neck surgical oncology center are based on the structural changes in the tissues. In addition, advancement in optical appliances and hardware, nanomolecules and reagents has provided ideal opportunities for cancer screening and diagnosis, either in the clinic, ward or operating room settings. In addition, nowadays, patients also seek less invasive and less time-consuming procedures. The quest for a safe, efficient and less time-consuming diagnostic method capable of detecting premalignant and malignant lesions has led to the generation of photodiagnosis by autofluorescence (AF) endoscopy techniques.
Autofluorescence is the fluorescence that is naturally emitted by the primary fluorophores within specific tissues. The endogenous fluorophores include collagen with its nicotinamide adenine dinucleotide dehydrogenase (NADH) and flavin adenine dinucleotide (FAD), metabolic products and other structural proteins which are the content of the tissues [7]. These endogenous fluorophores absorb light at specific wavelengths and correspondingly emit light at a longer wavelength (lower energy), which is referred to as autofluorescence. Fluorescence lifetime is considered a state function as it does not depend on initial perturbation conditions, such as duration of light exposure, excitation wavelength, fluorophore concentration and photobleaching, and is independent of fluorescence intensity [8].
These fluorophores can be a good indication of the pathological state of the tissues, as different tissues show different fluorescence [9]. Imperatively, the tumor cells are also able to produce a higher intensity of fluorescence and, depending on their contents of (NADH and FAD), they have a longer fluorescence lifetime, which can be applied in cancer screening and diagnosis. Generally, in the tumor, there is neoangiogenesis and hypervascularization. This can be associated with a relatively high blood content of hemoglobin. The hemoglobin contains the NADH and FAD. The fluorescence of NADH and FAD may increase due to the Warburg effect, or as cells become dysplastic due to the disruption of the extracellular matrix during tumor progression [10][11][10,11]. Since alterations in the blood supply and in the architectural organization result in a noticeably enhanced cellularity in the tumor mass, the involvement of tissue optical characteristics is crucial because they alter the scatter phenomena, absorption, and reflectance, thus impacting the movement of light. This also results in excitation and fluorescence collection from various tissue depths (Figure 1). Indeed, the expansion of the neoplastic mass affects the integrity and depth of localization of the highly fluorescing submucosa [12].
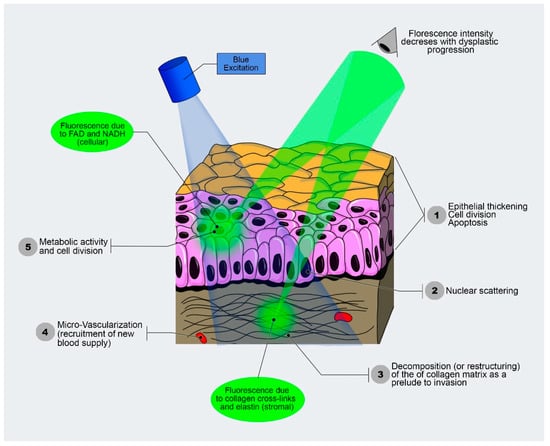
Figure 1. Autofluorescence functioning based on different fluorescence characteristics of the tissues, which illuminates with different intensity (modified from Optical Imaging Lab-screening and diagnosis with light, Vancouver, Canada).
Autofluorescence imaging (AFI) is an imaging modality that helps to visualize the autofluorescence bands of the endogenous fluorophores. When a specific wavelength of light and narrow-band filter are used, the normal mucosa appears as pale green autofluorescent compared with neoplastic tissues, which are visualized as a darker area due to the autofluorescence loss [7][13][14][7,13,14]. This is mainly due to loss of fluorophore collagen. Malignant tissues are characterized by numerous architectural changes such as high nuclear grade and mitochondrial density, as well as different amounts of keratin, elastin and collagen, which contribute to the different spectral characteristics if compared with the normal tissues [15]. These optical techniques such as microendoscopy and spectroscopy have been widely used to detect premalignant and malignant lesions based on subtle surface changes associated with mucosal ulceration and growth. These strategies have also been applied in a surgical setting, where the parameters of the tumor can be delineated effectively using optical imaging [13].
2. Clinical Application of Autofluorescence in Cancer Management
Recently, the application of autofluorescence endoscopy and imaging in biomedicine has surged globally in ensuring the optimum management of diseases and tumors, inclusive of head and neck malignancies. This applied new technology translates to better prognosis, survival and quality of life of any treated patients with upper aerodigestive tract tumors. For instance, early screening of malignant changes in the upper aerodigestive tract mucosa is the best strategy to enhance patient survival. Thus, screening is vital, especially targeting the population at high risk in certain geographic locations. Recently, many techniques that are frequently used in the diagnosis of oral cavity cancers, namely toluidine blue, Lugol’s iodine and brush biopsy, have dwindled due to certain limitations. In addition, the recent method of visual examination of the oral cavity for diagnosis of malignancy depends on the experience of the clinician in identifying early malignant changes. This requires a highly skilled and experienced surgeon and clinician who are able to detect suspicious tumor lesions during initial consultation. Indeed, recognizing the premalignant and early malignant lesions from benign inflammatory diseases by direct visual examination is challenging, not only for the trainee clinician but also for experienced practitioners. Imperatively, the premalignant lesions showed variable AF appearance. For example, mucosal alterations, which are characterized by overproduction of keratin or hyperkeratosis, are challenging to be recognized as harboring malignant cells. Macroscopically, in the majority of cases, these lesions appear as whitish grey “spots” on the surface of unhealthy mucosa. Generally, they exhibit a high fluorescence intensity and appear as a light green which is lighter than the healthy surrounding mucosa. Importantly, these lesions can mimic benign pathology in case there are no other characteristic fluorescence that can assist in identifying the underlying malignant transformation, such as the presence of violet or reddish blue spots [16][30]. Jo et al. reported that early dysplasia and early oral cancer can be distinguished from benign lesions by using multispectral endogenous fluorescence lifetime imaging [17][31]. This is based on a diagnostic computer generation system derived from the biochemical and biomarker used. VELscope is a nonmagnifying device, which is used for direct visualization of oral mucosa. In this device, an arc lamp of 120 W and a series of filters and reflectors were optimized for producing a 400–460nm wavelength light. In the oral mucosa, emitted light reaches and excites endogenous autofluorescence substances, known as fluorophores. This produces the autofluorescence signals, which are tissue-specific. It can be one of the selected devices used to further assess the hyperkeratotic lesions of the head and neck region. A study by Mascitti et al. comprised of 44 patients with oral dysplasia and OCSCC using both conventional oral examination and VELscope. They found out that the device gives high sensitivity and specificity for the differentiation of potentially malignant disorders and OCSCC from the normal healthy oral mucosa [18][19][19,32]. This is a vital study which highlight the effective usage of AF devices. Future studies are required to improve the specificity of this device, which may allow VELscope to be used in wider clinical applications in routine general practice globally [18][20][19,33]. Detection of precancerous lesions is challenging due to the multistep processes involved, in addition to field cancerization. Usually, direct visualization and inspection is used to diagnose early malignant lesion of the upper aerodigestive tract. This essentially depends on the expertise of the in-charged clinician in recognizing any suspicious lesions during clinical examination. However, it is challenging to detect and distinguish early malignant lesions from benign inflammatory pathology during a conventional white-light endoscopy, as this lesion may appear as normal healthy mucosa [16][30].2.1. Screening of Aerodigestive Tract Tumors by Autofluorescence
The screening and early detection of tumors are vital for achieving higher curative rates and improving prognosis of head and neck cancer patients. Oral cavity carcinoma is a significant tumor of the head and neck and is known for poor prognosis, and the majority of patients present with late-stage disease. Detecting the tumor early in the disease process ensures better treatment outcomes and prognosis. Chiang et al. showed that autofluorescence imaging is a useful adjunct used for screening for dysplasia and premalignant lesions in the oral cavity [21][22][23][34,35,36]. Noteworthily, the application of autofluorescence videoendoscopy for assessing the head and neck carcinoma is a promising method in the armamentarium of cancer management, because it has greater specificity and sensitivity. Gorpas et al. reported that oral lichen planus can be diagnosed by using a time-resolved fluorescence spectroscopy [24][37]. It is a noninvasive, time-efficient and safe procedure. The mucosa surrounding the tumor can be visualized effectively using autofluorescence (Figure 2). This means that the autofluorescence-based device can be used as an effective screening method and follow-up examination in a high-risk patient population.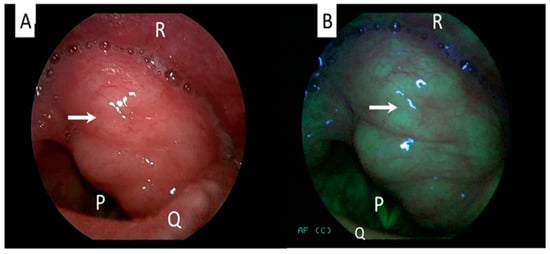
Figure 2. Laryngeal examination of a patient with benign laryngeal tumor showing no changes in the mucosa between white-light (A) and autofluorescence mode (B). Arrow indicates the tumor. Structure P: vocal cord/glottic, Q: epiglottis, R: posterior pharyngeal wall (Figure is from author’s own collection).
2.2. Diagnosis of Aerodigestive Tract Tumors by Autofluorescence Techniques
Head and neck cancer diagnosis requires a thorough clinical examination. A physical examination can determine an accurate clinical characteristic of tumoral mass, such as ulcerative pattern, infiltration depth or presence of multiple matted neck metastases. Endoscopic evaluation of suspicious malignant lesions with autofluorescence is mandatory to investigate all the subsites’ involvement to facilitate a comprehensive biopsy of selected tissues, which in turn can produce high representative tumoral tissues. In addition, these autofluorescent techniques will also allow clinicians to exclude the presence of second primary tumors. A complete biopsy of a suspicious lesion will produce accurate histological types of tumors, which is vital for a subsequent refined treatment plan. During endoscopic autofluorescence evaluation, extra information about mucosal and submucosal changes to better characterize the lesion and its margins can be obtained. For instance, the nasopharyngeal area can be assessed with autofluorescence for any suspicious malignant changes (Figure 3). This technique allows early diagnosis of nasopharyngeal carcinoma [42][52]. A challenging issue is to determine whether conditions of chronic inflammation, such as chronic laryngitis and hyperkeratosis or pre-neoplastic lesions, such as leucoplakia, will show a mild or severe dysplasia [43][53]. The tissue biopsy and histopathological examination remain as the gold standard for diagnosis of any head and neck cancers, inclusive of oral cavity carcinoma [44][54]. In these cases, autofluorescent endoscopic techniques are useful for targeted tissue biopsy as they highlight the highly suspicious malignant areas. In select groups of patients, direct examination under general anesthesia with laryngoscopy, bronchoscopy and endoscopy will allow multiple biopsies from different anatomic subsites simultaneously.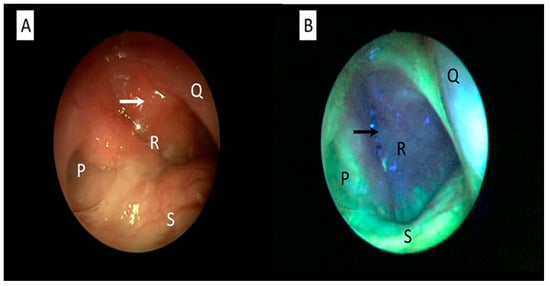
Figure 3. Nasopharyngeal examination of a patient with nasopharyngeal cancer using white-light (A) and autofluorescence mode (B). Abnormal mucosa around the cancerous area is clearly seen as autofluorescent loss compared with the normal healthy mucosa, which appears as cyan-green. An arrow indicates cancerous mucosa. Structure P: eustachian tube. Q: posterior part of nasal septum, R: nasopharynx, S: floor of nasal cavity (Figure is from author’s own collection).
2.3. Treatment of Aerodigestive Tract Tumors by Autofluorescence Techniques
The primary objective of tumor surgery is to maximize tumor removal and minimize the damage to the surrounding healthy tissue. Extensive resection with unnecessary removal of normal tissue may result in significant functional impairment, as the head and neck regions involve the structures that play vital roles in breathing, speech, swallowing and so forth. At the end of the spectrum, if the tumor resection is incomplete, the probability of the disease to recur is high. Recurrent tumors are difficult to manage and are associated with poor prognosis and survival. A positive surgical margin is associated with a dismal prognosis in terms of increased local recurrence and decreased patient overall survival [50][51][60,61]. Therefore, the ability to define the tumor resection margin with greater accuracy is a prerequisite in order to attain the best effective treatment for optimal patient management. For example, the usage of a fluorescence lifetime imaging technique in transoral robotic surgery enables the detection of oropharyngeal carcinoma in the setting of the management of metastatic carcinoma of unknown primary [52][62]. Additionally, the resection margin of oral and oropharyngeal cancer can be determined by using this technique [53][54][63,64]. This technique is an adjunct to visual inspection during intraoperative transoral robotic resection of oral cancers, in order to achieve a clear surgical margin [55][65]. Autofluorescent endoscopy aided with up-to-date scanning can further increase the effectiveness of surgical therapy of upper aerodigestive tract tumors. The developed scan with scanning time in the order of seconds can provide an objective, fast and cost-effective tool which is able to provide real-time assessment for a complete resection margin. Of note, this technique is able to quantify not only the surface mucosa but also different faces of the resection margins. In addition, Tajudeen et al. highlighted the usage of dynamic contrast imaging in aiding the good resection of tumor margins [56][66]. The availability of these various highly advance techniques will strengthen the management protocol for all head and neck cancer patients. To illustrate further, in the management oral cavity malignancy, the margin can be safely delineated by using autofluorescence (Figure 4). A safe resection margin is vital to avoid residual micrometastatic tumor deposits at the periphery of the main tumor. This is critical to hinder the tumor recurrence that is difficult to manage, as well as to prevent distant metastases. Leukoplakia should also be resected with a good margin in order to prevent a geographical miss. Leukoplakia, which is one of the important risk factors for oral cancer, may show hyperkeratosis with variable degree of dysplasia when examined microscopically [57][58][67,68]. Lesions at the dorsum of the tongue and floor of the mouth are the most probable to be dysplastic, especially in elderly patients who are chronic smokers. Erythroplakia is a rarer lesion but clinically significant, as it carries higher risk of malignancy [58][68]. Thus, meticulous assessment of erythroplakia is necessary, and biopsy is warranted in highly suspicious cases.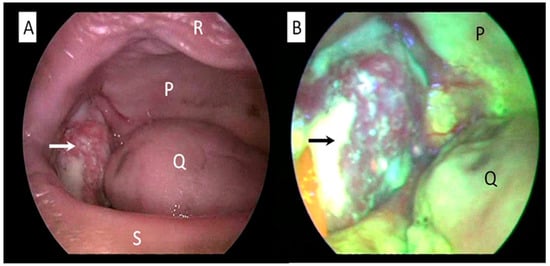
Figure 4. Oral cavity examination of a patient with oral cavity cancer using white-light (A) and autofluorescence mode (B). Abnormal mucosa around the cancerous area is clearly seen as autofluorescence loss compared with the surrounding normal healthy mucosa. An arrow indicates cancerous mass arising from buccal mucosa. Structure P: hard palate, Q: tongue, R: upper lip, S: lower lip (Figure is from author’s own collection).
