2. Risk Factors for Grade C POPF
Although there are many studies on risk factors for POPF, few studies have examined and identified risk factors for the development of grade C POPF. The risk factor most consistently shown to be predictive of grade C POPF after pancreatic surgery is soft gland texture, while other factors, such as male sex, small pancreatic duct diameter <3 mm, BMI ≥25.0 kg/m
2, preoperative serum albumin <3.0 g/mL, high intraoperative blood loss, and an operative time ≥480 min, were also reported
[9][10][11][12][10,11,12,13]. To better evaluate the characteristics of the pancreas before surgery, imaging examinations, including retrorenal fat thickness, subcutaneous fat area, and total fat area, were found to be significant predictors of grade C pancreatic fistula
[13][14].
Despite these possible risk factors, they are not particularly helpful for prevention or treatment because of the usually unchangeable features in clinical practice. Chiba et al., in a recent retrospective study, found that the detection of gram-negative rods within the first 7 postoperative days was a significant factor after multivariate analysis. Interestingly, this study also found that neither preoperative biliary drainage nor cholangitis were independent risk factors for grade C POPF
[14][15]. Therefore, the relationship between infection and grade C POPF may be a novel and useful direction of study.
3. Operation Technique
3.1. Pancreaticojejunostomy Dehiscence Is Found in Grade C POPF after PD on Radiographic Examination
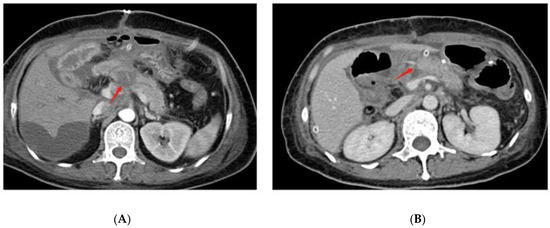
On radiographic examination, grade C POPF was found to have wider diameters of pancreaticojejunostomy dehiscence (
Figure 1A) than grade A and grade B POPF after pancreaticoduodenectomy. In this research, most grade C pancreatic fistulas were combined with infection, which can be interpreted as dehiscent anastomosis
[15][39]. In addition to the complete dehiscence of the pancreaticojejunostomy, the crevice of the pancreaticojejunostomy (
Figure 1B) can also cause grade C POPF. Another study found that CT-imaging findings of fluid collection on the dorsal side of pancreaticojejunostomy and operative area bubble signs remained significant predictive factors of delayed hemorrhage in POPF patients
[16][40]. Because postoperative hemorrhage is one of the leading causes of death in grade C POPF, these CT manifestations might also indicate the occurrence of grade CPOPF.
Figure 1. Postoperative CT findings of grade C POPF. (A) shows the complete dehiscence of the pancreaticojejunostomy at the red arrow. (B) shows the crevice of the pancreaticojejunostomy at the red arrow.
3.2. Reconstruction Methods
Confirming the best reconstruction method for pancreatic surgery has remained controversial up to now. Pancreaticogastrostomy (PG) and pancreaticojejunostomy (PJ) are the most common reconstruction methods among the several available techniques. Local inflammation due to the leakage of the pancreatic anastomosis is induced by activated pancreatic enzymes on the one hand and the simultaneous leakage of enteric microorganisms on the other hand. Keck et al.
[17][41] reported the rate of CR-POPF in a multicenter randomized controlled trial with 440 patients. They concluded that the rate of grade B/C fistula after PG versus PJ was not different, but grade C pancreatic fistula was not discussed. However, they performed a perioperative secondary endpoint analysis and found that there was no significant difference in perioperative in-house mortality (PG vs. PJ, 6% vs. 5%,
p = 0.963) or 90-day mortality (PG vs. PJ, 10% vs. 5%,
p = 0.167). Recently, several meta-analyses have compared PG and PJ, and most concluded that there was no significant difference in the rate of CR-POPF
[18][19][20][21][22][23][24][42,43,44,45,46,47,48]. Cheng et al.
[19][43] demonstrated that PJ probably has little or no difference from PG in the risk of postoperative mortality (3.9% versus 4.8%; RR 0.84, 95% CI 0.53 to 1.34; moderate-quality evidence). However, a recent meta-analysis compared 971 patients who underwent PJ end-to-side duct-to-mucosa, 791 patients who underwent PJ end-to-side invagination, 505 patients who underwent PG end-to-side invagination, and 98 patients who underwent PG end-to-side duct-to-mucosa and demonstrated that duct-to-mucosa pancreaticogastrostomy was associated with the lowest rates of clinically relevant POPF and had the best outcome profile, in terms of postoperative morbidity and postoperative mortality, among all pancreatic anastomosis techniques following PD
[20][44]. Controversially, an RCT published in 2020 found that PJ had a lower incidence of grade C POPF than PG among patients at the highest risk for POPF (0% versus 11.1%)
[25][49]. In contrast, this study applied a risk stratification system and included only patients at high risk for POPF, and an external stent was used in all patients.
Reconstruction after pancreatic surgery remains under debate, and most studies have found no difference in the rate of CR-POPF after PD. Therefore, the reconstruction method should be identified based on the condition of the patients, tumor characteristics, and the habits of surgeons.
3.3. Anastomotic Techniques
In addition to bowel reconstruction, anastomotic techniques are critical in pancreatic surgery. To date, there have been more than 50 different pancreaticojejunostomy methods, including end-to-end anastomosis and end-to-side anastomosis, coating-in, binding, and duct-to-mucosa anastomosis. The incidence of pancreatic fistula varies with different anastomosis methods. Currently, end-to-end invagination pancreaticojejunostomy and end-to-side duct-to-mucosa pancreaticojejunostomy are the two most widely used anastomosis methods in clinical practice. End-to-side duct-to-mucosa pancreaticojejunostomy includes anastomosis of the pancreatic duct and jejunum mucosa and anastomosis of pancreatic palpation and the jejunum plasma muscle layer, usually in the form of end-to-side anastomosis. However, the anastomotic procedure is not always easy, particularly with narrow pancreatic ducts and a soft pancreas. End-to-end invagination pancreaticojejunostomy, an easier reconstruction method, refers to the insertion of the intact pancreatic stump into the jejunum, which can be a single or double anastomosis.
A 120-patient RCT conducted by Senda et al. in 2018 found no significant difference in the incidence of clinical pancreatic fistulas between duct-to-mucosa PJ and invagination PJ, but in high-risk patients with a soft pancreas, the incidence of clinical pancreatic fistulas was better reduced by invagination PJ, and patients who underwent invagination PJ had shorter hospital stays
[26][50]. The possible reason is that a soft pancreas is usually accompanied by a small main pancreatic duct diameter, which directly increases the difficulty of anastomosis between the pancreatic duct and jejunal mucosa. Some meta-analyses also demonstrated that invagination PJ did not reduce CR-POPF rates compared to duct-to-mucosa PJ, especially in patients with a hard pancreas
[22][27][46,51]. However, a meta-analysis found a superiority of invagination anastomosis over duct-to-mucosa anastomosis in reducing the risk of grade B/C POPF, but it did not significantly reduce the mortality rate or length of hospital stay. The effect of invagination in reducing pancreatic fistula formation is obvious in patients with a soft pancreas, but there is no significant difference between the two anastomosis techniques in patients with a hard pancreas
[28][52].
However, several recent studies have found a superiority of an uncommon anastomosis technology named Blumgart anastomosis (BA). BA was devised by LH Blumgart in 2000 and combines the principle of duct-to-mucosa anastomosis with the invagination technique of the pancreas remnant, showing a low rate of grade C POPF
[29][53]. The original Blumgart technique was subsequently modified by decreasing the number of transpancreatic sutures and by tying the sutures only once over the anterior aspect of the jejunal limb, instead of first tying them on the pancreas before placing the anterior seromuscular suture on the jejunum
[30][54]. Several studies found that BA reduced severe complications, such as POPF grade C, reoperation rate, and 90-day mortality, after PD compared to traditional PJ
[30][31][54,55]. Therefore, BA could be used with more frequency, and the transpancreatic U-suture, the small incision of the jejunal loop, and jejunal wrapping seemed to be the key technical factors.
Similar to reconstruction methods, traditional anastomotic techniques after pancreatic surgery are under debate, and the results of most studies could be affected by many factors, including the condition of patients, characteristics of tumors, and the technology of surgeons. With the improvement of anastomosis technology, the new method of BA anastomosis may be reliable and feasible in clinical practice. Therefore, more high-quality RCTs are needed to confirm this notion.
3.4. Stent or No-Stent
Stent placement in PJ anastomosis is also controversial, as is whether the stent should be an external or internal stent. Several recent meta-analyses have found that stent use has the potential benefit of reducing the incidence of POPF
[32][33][34][56,57,58]. However, Pessaux et al. found that stents mainly reduced the occurrence of grade B pancreatic fistula, but there was no significant difference in the incidence of grade C pancreatic fistula
[35][59]. Compared with stents, external stents exert a more pronounced effect on the prevention of CR-POPF, especially grade C POPF
[36][37][60,61]. The reason might be that the external stent minimizes the digestive erosion of the residual pancreas and fully eliminates pancreatic juices from the anastomosis.
From what has been discussed above, external stent application in PD is better than internal stent application in reducing the incidence of grade C POPF; however, whether stent use could reduce grade C POPF is still unclear. Because few studies have discussed grade C POPF alone, along with the superiority of external stents compared to internal stents, additional RCTs comparing the efficacy toward grade C POPF of external pancreatic duct stenting versus non-stenting must be performed, particularly for cases with a high risk for pancreatic fistula.
3.5. Two-Stage Surgical Procedure
A two-stage surgical procedure was undertaken to prevent the development of POPF in patients with high-risk pancreases, which contained two approaches: completion pancreatectomy or two-stage pancreaticojejunostomy. The purpose of the planned PD intraoperatively converted to completion pancreatectomy is to remove the source of inflammation and leakage and to prevent POPF. Recently, several analyses have demonstrated that completion pancreatectomy exhibited lower rates of major morbidity and comparable mortality compared to high-risk PD
[38][39][40][62,63,64]. Despite acceptable postoperative outcomes, performing completion pancreatectomy still raises important concerns due to the inevitable presence of endocrine and exocrine insufficiency. Since completion pancreatectomy does not appear to reduce mortality, completion pancreatectomy may be considered rather than high-risk PD only in a few selected cases. Another method is two-stage pancreaticojejunostomy. In the two-stage PJ method, the insertion of an external tube is performed first, in which the tube is not passed through the jejunal loop, followed approximately 3 months later by second-stage reconstruction for PJ. A few studies have reported this method with a low rate of postoperative hemorrhage and mortality and indicated that two-stage PJ may be a safe and useful method in PD in patients with a soft pancreas or a narrow main pancreatic duct
[41][42][43][65,66,67]. However, the availability of both methods requires more high-quality studies in the future.
4. Surgical Treatment for Grade C POPF
According to the definition revised by ISGPF, grade C POPF usually requires surgical treatment. During relaparotomy, different surgical strategies are possible: completion pancreatectomy, the revision of the pancreatic anastomosis, and the bridge stent technique
[44][98].
4.1. Debridement and Open Drainage
For POPF, a step-up approach is usually used in fluid collection, which is first treated by antibiotic therapy and then radiologic-guided drainage or endoscopic ultrasound-guided drainage. If the patients developed postoperative abdominal bleeding, hemostatic therapy or angiographic procedures were needed. Once conservative treatment fails, reoperation becomes the last option. Debridement and drainage are the basic operations for patients with grade C pancreatic fistula after the failure of interventional procedures. The advantages of this approach are a short operation time, less trauma, and safety, and simple drainage is significantly superior in most evaluated parameters, such as the lower rate of 90-day mortality. However, it is frequently associated with high rates of reoperations compared to completion pancreatectomy and PJ disconnection
[45][46][99,100]. Therefore, debridement and drainage seem to be indicated in patients with uncomplicated dehiscence or severe hemodynamic instability.
4.2. Completion Pancreatectomy
Completion pancreatectomy is the most aggressive strategy to treat grade C POPF, especially in cases of PJ dehiscence with severe inflammation. A theoretical advantage of completion pancreatectomy is that it completely removes the focus of intra-abdominal leakage and the source of inflammation, thereby possibly decreasing the risk of additional relaparotomies. However, this radical surgical strategy may induce the deterioration of organ failure, intraoperative blood loss, the risk of damaging other structures, and pancreatic exocrine and endocrine insufficiency
[47][101]. Due to the high mortality and the low quality of life of patients after completion pancreatectomy, surgeons prefer a pancreas-preserving procedure to completion pancreatectomy during relaparotomy, and only in the case of pancreatic necrosis or the complete destruction of the former anastomosis can completion pancreatectomy be reserved. According to the above theories of intestinal fluid and intestinal bacteria in the occurrence of grade C POPF, another surgical treatment was gradually applied that blocked the flow of pancreatic fluid to the intestines to control local infection.
4.3. Revision of the Pancreatic Anastomosis
Repeating PJ anastomosis usually includes two parts: salvage relaparotomy and wirsungostomy, and delayed restorative laparotomy reconstructing the PJ anastomosis. A study implemented this strategy in patients with grade C POPF, and most patients underwent repeat pancreaticojejunostomy after wirsungostomy with unaltered long-term endocrine function
[48][102]. The precondition of repeating PJ anastomosis is that the patients survive after wirsungostomy. Several analyses have found that wirsungostomy seems not to be inferior to open drainage procedures or completion pancreatectomy in terms of mortality rate
[45][49][99,103]. Meanwhile, this treatment for grade C POPF has the advantage of preserving pancreatic function compared to completion pancreatectomy and may be an alternate method for surgeons.
4.4. The Bridge Stent Technique
The bridge stent technique is an alternative approach for managing PJ dehiscence in the following steps: a. Transpancreatic U-stitches are placed at the edge of the pancreatic stump to avoid leakage; b. The distal part of the thin silicon tube stenting the pancreatic duct is inserted into the jejunal lumen and fixed by purse-string sutures to the jejunal wall; c. An irrigating catheter and drains are put in place
[50][104]. Kent et al. used this technique in five patients with grade C POPF, and all those patients survived this complication and were discharged from the hospital without long-term complications of PJ anastomosis
[51][105]. Therefore, the bridge stent technique may be a safe and effective method for treating grade C POPF while retaining pancreatic function.
Grade C POPF following pancreaticoduodenectomy is a rare and difficult problem to manage. Traditionally, re-exploration with completion pancreatectomy and wide drainage has been employed, but this process carries significant morbidity and mortality. The revision of the pancreatic anastomosis or the bridge stent technique seems to have a higher priority than completion pancreatectomy, and studies with a larger sample size and longer follow-up are required to establish the short- and long-term efficacy.