Obesity is a critical medical condition worldwide that is increasingly involved with nutritional derangements associated with micronutrient deficiencies, including iron, zinc, calcium, magnesium, selenium, and vitamins A, C, D, and E. Nutritional deficiencies in obesity are mainly caused by poor-quality diets, higher nutrient requirements, alterations in micronutrient metabolism, and invasive obesity treatments. The current conventional agricultural system is designed for intensive food production, focusing on food quantity rather than food quality, consuming excessive agricultural inputs, and producing nutrient-deficient foods, thus generating severe health and environmental problems; agricultural food products may worsen obesity-related malnutrition. Therefore, modern agriculture is adopting new biofortification technologies to combat micronutrient deficiencies and improve agricultural productivity and sustainability.
- agri-food systems
- beneficial soil microorganisms
- biofertilization
- micronutrients
- nanofertilization
- obesity
- malnutrition
1. Introduction
2. Nutritional Deficiencies Associated with Overweight or Obese Patients
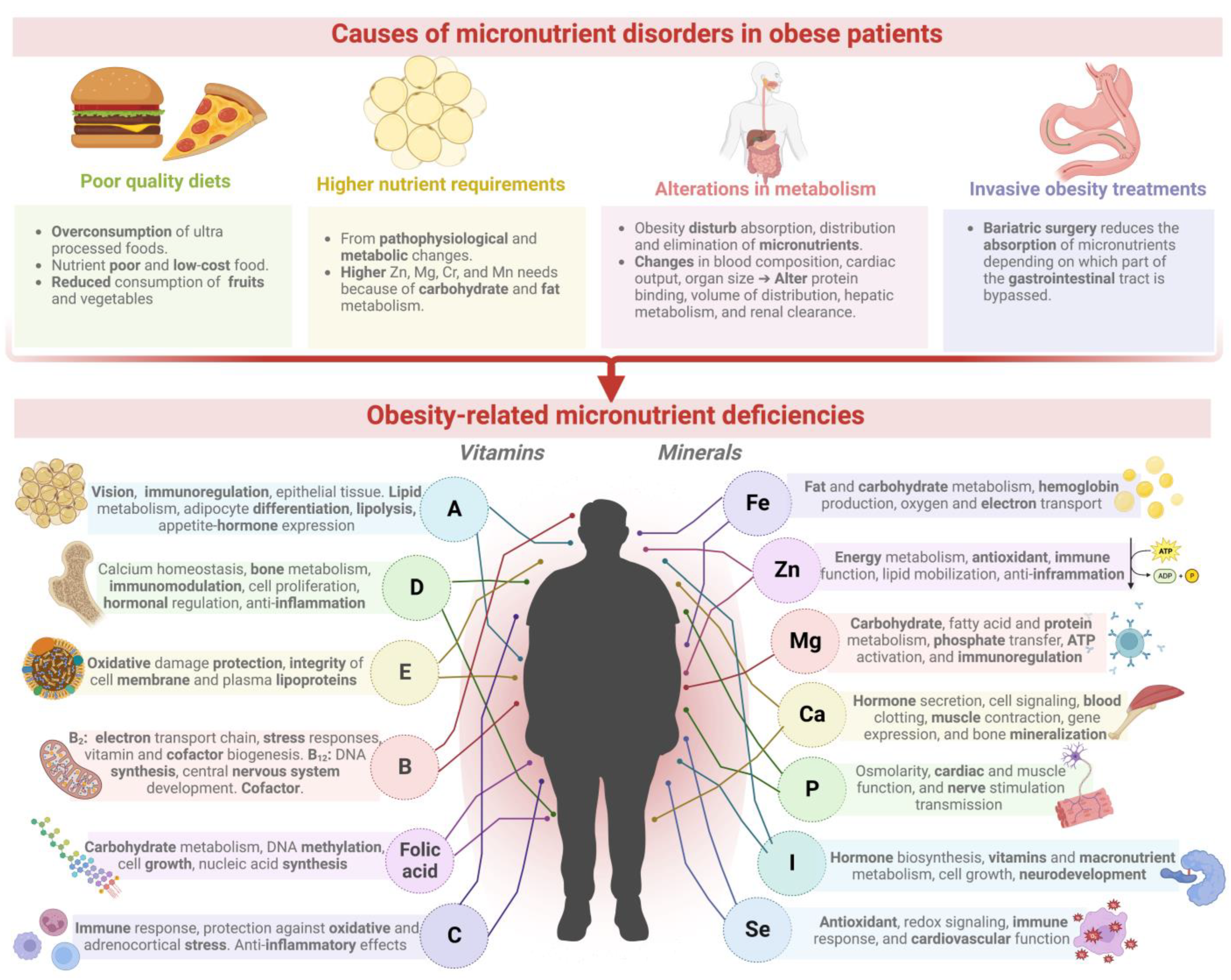
| Micronutrient | Micronutrient Physiologic and Metabolic Function | Deficiency in Obese Patients | Type of Condition | Reference | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vitamin A and carotenoids | Retina and epithelial tissue development, lipid metabolism, immune system function. Inhibition of adipocyte differentiation by enhancing lipolysis. Reduction in leptin and resistin expression [14,47]. | Retina and epithelial tissue development, lipid metabolism, immune system function. Inhibition of adipocyte differentiation by enhancing lipolysis. Reduction in leptin and resistin expression [14][47]. | Carotenoids (α-carotene, β-carotene, ζ-carotene, lutein, and lycopene) ≈ 44.4%. | Male (n = 29) and female (n = 37) individuals between 49 and 58 years old with a body mass index (BMI) > 30 kg/m | 2 | . | [48] | |||
| All evaluated patients presented a deficiency of vitamin A (<30 µg/dL). | Individuals with a BMI over 25 kg/m | 2 | (overweight) and 30 kg/m | 2 | (obesity) aged 18–65 years (n = 127). | [6] | ||||
| Vitamin D | Calcium homeostasis, bone metabolism, immunomodulation, cell proliferation, and control of hormonal systems. Upregulates anti-inflammatory cytokines [49]. | Approximately 16.5% presented a deficiency of serum 25 hydroxy vitamin D (<30 nmol/L). | Danish individuals; 6–18 years old (n = 1484) with overweight/obesity; body mass index standard deviation score (BMI Z-score) > 2.33. | [50] | ||||||
| The prevalence of deficiency (≤20 ng/mL) is around 90%. | Obese individuals class II and III (BMI ≥ 35 and ≥40 kg/m | 2 | ). | [2] | ||||||
| Vitamin E | Protection of cell constituents from oxidative damage, such as polyunsaturated fatty acids found in the membrane and plasma lipoproteins [51]. | Deficiency of 61.5% (11.5 ± 12.2 mg/L), and 47.8% (15.6 ± 12.2 mg/L) in obese and metabolic syndrome patients, respectively. | Individuals 10–16 years old from Central Turkey with obesity (BMI Z-score > 2) (n = 73) or metabolic syndrome (waist circumference ≥ 90 cm (n = 64). | [52] | ||||||
| Vitamin B | 2 | Mitochondrial electron transport chain function and homocysteine metabolism. Its derivatives, flavin mononucleotide and flavin adenine dinucleotide, are implicated in stress responses and vitamin and cofactor biogenesis [53]. | Deficit of 48.9% in the obese group (89.1 ± 35 μg/L); 33.1% in the metabolic syndrome group (116.7 ± 65.2 μg/L). | Individuals 10–16 years old from Central Turkey with obesity (BMI Z-score > 2) (n = 73) or metabolic syndrome (waist circumference ≥ 90 cm (n = 64). | [52] | |||||
| Deficiency of 38.8% (<5 ng/mL). | Children 11–17 years old (n = 50) with obesity (BMI Z-score ≥ 2). | [54] | ||||||||
| Vitamin B | 12 | DNA synthesis, conversion of homocysteine to methionine, and central nervous system development. Cofactor in the one-carbon metabolism and propionate catabolism [55,56]. | DNA synthesis, conversion of homocysteine to methionine, and central nervous system development. Cofactor in the one-carbon metabolism and propionate catabolism [55][56]. | Insufficiency of 23% (< 150 pmol/l) in cohort 1 and 18.3% in cohort 2. | Two cohorts of pregnant women (16–18 weeks) (n = 244 and n = 60) with average BMI = 26.5 ± 5.5 kg/m | 2 | for cohort 1 and BMI = 32.6 ± 11.2 kg/m | 2 | for cohort 2. | [57] |
| Deficiency of around 29% (397.5 ± 26.3 ng/L). | Forty obese adults (BMI > 35 kg/m | 2 | ) aged 21–49 underwent bariatric surgery. | [58] | ||||||
| Folic acid | Well-functioning carbohydrate metabolism (15). DNA methylation, cell growth, and nucleic acid synthesis [56]. | Prevalence of 54% (obese) and 65% (patients after bariatric surgery). | Patients with morbid obesity before (BMI > 30 kg/m | 2 | ) and after bariatric surgery (BMI > 35 kg/m | 2 | ). | [56] | ||
| Inadequacies (<10 nmol/L) per area: America (0.8–2.1%), Europe and Eastern Mediterranean (40.9%), Africa (24.4%), Southeast Asia, and Western Pacific (1.1–3.7%). | Women with a rising prevalence of overweight and/or obesity (BMI > 18.5 kg/m | 2 | ) in reproductive age (15–49 years old) in 17 population surveys. | [59] | ||||||
| Vitamin C | Immune response, protection against oxidative and adrenocortical stress. Anti-inflammatory effects [60]. | Deficit of 24.6%, 32.8%, and 34.6% for sarcopenic, osteopenic, and osteosarcopenic obese individuals. | Korean women (n = 1344) postmenopausal (>50 years old) with osteosarcopenic (BMI = 27.15 kg/m | 2 | ), sarcopenic (BMI = 28.12 kg/m | 2 | ), and osteopenic (BMI = 26.24 kg/m | 2 | ) obesity. | [61] |
| Iron | Fat and carbohydrate metabolism, hemoglobin production, oxygen transport, DNA synthesis, and electron transport [14,62]. | Fat and carbohydrate metabolism, hemoglobin production, oxygen transport, DNA synthesis, and electron transport [14][62]. | Deficiency of 31.8% in male and 25.9% in female patients. | Children 8–9 years old (n = 160) with high body fat (BMI Z-score > 1) in Sri Lanka. | [63] | |||||
| Insufficiency in patients with peripheral (16.9%) and central (10.7%) adiposity. | Overweight and/or obese American young women (23–43 years old; BMI ≥ 25 kg/m | 2 | ; n = 81). | [64] | ||||||
| Zinc | Energy metabolism with antioxidant and immunological properties. Stimulates the function of zinc-α2-glycoprotein (adipokine with lipid mobilizing and anti-inflammatory activity) [65]. | Prevalence of 24–74% after bypass surgery: biliopancreatic bypass (45–91%), gastric bypass (15–21%), laparoscopic sleeve gastrectomy (11–14%). | Patients with morbid obesity before (BMI > 30 kg/m | 2 | ) and after bariatric surgery (BMI > 35 kg/m | 2 | ). | [56] | ||
| Deficiency prevalence of 84.7% (<70 µg/dL fasted). | Women rising prevalence of overweight and/or obesity (BMI > 18.5 kg/m | 2 | ) in reproductive age (15–49 years old). | [59] | ||||||
| Magnesium | Carbohydrate metabolism, phosphate transfer reactions, fatty acid and protein synthesis, ATP activation, and immune system function [62,66]. | Carbohydrate metabolism, phosphate transfer reactions, fatty acid and protein synthesis, ATP activation, and immune system function [62][66]. | Deficiency in males was 6.6%, and, in females, was 7.7%. | Children 8–9 years old (n = 160) with high body fat (BMI Z-score > 1) in Sri Lanka. | [63] | |||||
| Calcium | Hormone secretion, intracellular signaling, blood clotting, muscle contraction, gene expression, and bone mineralization [67,68]. | Hormone secretion, intracellular signaling, blood clotting, muscle contraction, gene expression, and bone mineralization [67][68]. | Deficiency of 50.2% in obese women. | Obese women (35.37 ± 2.09 years old) with average BMI = 34.68 ± 0.61 kg/m | 2 | (n = 70). | [69] | |||
| Potassium | Cellular osmolarity, acid–base equilibrium, cardiac and muscle function, and nerve stimulation transmission [70]. | Deficiency of 59.6% in obese women. | Obese women (35.37 ± 2.09 years old) average BMI= 34.68 ± 0.61 kg/m | 2 | (n = 70) | [69] | ||||
| 100% of patients showed deficiency (<3.5 mmol/L). | Individuals with a BMI over 25 kg/m | 2 | (overweight) and 30 kg/m | 2 | (obesity) aged 18–65 years (n = 127). | [6] | ||||
| Iodine | Thyroid hormones biosynthesis, vitamins, macronutrient metabolism, and cell growth fetal and child neurodevelopment [71,72]. | Thyroid hormones biosynthesis, vitamins, macronutrient metabolism, and cell growth fetal and child neurodevelopment [71][72]. | Insufficiency prevalence of 24.4%. | Overweight (BMI > 25 kg/m | 2 | ) and obese (BMI > 30 kg/m | 2 | ) children (11–13 years old) residing in iodine-sufficient areas (IS) and mildly iodine-deficient areas (ID). | [73] | |
| Selenium | Antioxidant defense, redox signaling, immune response, and cardiovascular function [74]. | Deficiency of 25.9% in plasma and 34.2% in the erythrocyte. | Obese women aged 20–50 years (BMI ≥ 35 kg/m | 2 | , n = 63). | [75] | ||||
| Copper | Electron transport, protein structure, mitochondrial respiratory chain, immune function, antioxidant defense. Cofactor of redox enzymes [56,76]. | Electron transport, protein structure, mitochondrial respiratory chain, immune function, antioxidant defense. Cofactor of redox enzymes [56][76]. | Concentration decreased by 16% 12 months after bariatric surgery. | Norwegian patients (85% women) 27–59 years old, eligible for bariatric surgery (BMI = 42.4 ± 3.6 kg/m | 2 | , n = 46). | [77] | |||
| Prevalence of 46.7%. | Overweight/obese children aged 6–16 years (average BMI = 24.78 ± 3.93 kg/m | 2 | , n = 69). | [78] |
References
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in Adults: A Clinical Practice Guideline. Can. Med. Assoc. J. 2020, 192, E875–E891.
- Astrup, A.; Bügel, S. Overfed but Undernourished: Recognizing Nutritional Inadequacies/Deficiencies in Patients with Overweight or Obesity. Int. J. Obes. 2019, 43, 219–232.
- Upadhyay, J.; Farr, O.; Perakakis, N.; Ghaly, W.; Mantzoros, C. Obesity as a Disease. Med. Clin. N. Am. 2018, 102, 13–33.
- Mureșan Ciobârcă, D.; Cătoi, A.F.; Copăescu, C.; Miere, D.; Crișan, G. Nutritional Status Prior to Bariatric Surgery for Severe Obesity: A Review. Med. Pharm. Rep. 2022, 95, 24–30.
- Barazzoni, R.; Gortan Cappellari, G. Double Burden of Malnutrition in Persons with Obesity. Rev. Endocr. Metab. Disord. 2020, 21, 307–313.
- McKay, J.; Ho, S.; Jane, M.; Pal, S. Overweight & Obese Australian Adults and Micronutrient Deficiency. BMC Nutr. 2020, 6, 12.
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 October 2022).
- WHO. Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 12 October 2022).
- Kobylińska, M.; Antosik, K.; Decyk, A.; Kurowska, K. Malnutrition in Obesity: Is It Possible? Obes. Facts 2022, 15, 19–25.
- Zhou, S.; Ye, B.; Fu, P.; Li, S.; Yuan, P.; Yang, L.; Zhan, X.; Chao, F.; Zhang, S.; Wang, M.Q.; et al. Double Burden of Malnutrition: Examining the Growth Profile and Coexistence of Undernutrition, Overweight, and Obesity among School-Aged Children and Adolescents in Urban and Rural Counties in Henan Province, China. J. Obes. 2020, 2020, 2962138.
- Blaak, E.E. Current Metabolic Perspective on Malnutrition in Obesity: Towards More Subgroup-Based Nutritional Approaches? Proc. Nutr. Soc. 2020, 79, 331–337.
- Pramono, A.; Jocken, J.W.E.; Blaak, E.E. Vitamin D Deficiency in the Aetiology of Obesity-Related Insulin Resistance. Diabetes Metab. Res. Rev. 2019, 35, e3146.
- Botchlett, R.; Wu, C. Diet Composition for the Management of Obesity and Obesity-Related Disorders. J. Diabetes Mellit. Metab. Syndr. 2018, 3, 10.
- Lapik, I.A.; Galchenko, A.V.; Gapparova, K.M. Micronutrient Status in Obese Patients: A Narrative Review. Obes. Med. 2020, 18, 100224.
- Hesham, A.E.-L.; Kaur, T.; Devi, R.; Kour, D.; Prasad, S.; Yadav, N.; Singh, C.; Singh, J.; Yadav, A.N. Current Trends in Microbial Biotechnology for Agricultural Sustainability: Conclusion and Future Challenges. In Current Trends in Microbial Biotechnology for Sustainable Agriculture; Environmental and Microbial Biotechnology; Yadav, A.N., Singh, J., Singh, C., Yadav, N., Eds.; Springer: Singapore, 2021; pp. 555–572.
- Acharya, A.; Pal, P.K. Agriculture Nanotechnology: Translating Research Outcome to Field Applications by Influencing Environmental Sustainability. NanoImpact 2020, 19, 100232.
- Khatoon, Z.; Huang, S.; Rafique, M.; Fakhar, A.; Kamran, M.A.; Santoyo, G. Unlocking the Potential of Plant Growth-Promoting Rhizobacteria on Soil Health and the Sustainability of Agricultural Systems. J. Environ. Manag. 2020, 273, 111118.
- Adisa, I.O.; Pullagurala, V.L.R.; Peralta-Videa, J.R.; Dimkpa, C.O.; Elmer, W.H.; Gardea-Torresdey, J.L.; White, J.C. Recent Advances in Nano-Enabled Fertilizers and Pesticides: A Critical Review of Mechanisms of Action. Environ. Sci. Nano 2019, 6, 2002–2030.
- Elemike, E.E.; Uzoh, I.M.; Onwudiwe, D.C.; Babalola, O.O. The Role of Nanotechnology in the Fortification of Plant Nutrients and Improvement of Crop Production. Appl. Sci. 2019, 9, 499.
- Kumari, R.; Singh, D.P. Nano-Biofertilizer: An Emerging Eco-Friendly Approach for Sustainable Agriculture. Proc. Natl. Acad. Sci. India Sect. B Biol. Sci. 2019, 90, 733–741.
- El-Ghamry, A.; Mosa, A.A.; Alshaal, T.; El-Ramady, H. Nanofertilizers vs. Biofertilizers: New Insights. Environ. Biodiv. Soil. Secur. 2018, 2, 51–72.
- Umar, W.; Hameed, M.K.; Aziz, T.; Maqsood, M.A.; Bilal, H.M.; Rasheed, N. Synthesis, Characterization and Application of ZnO Nanoparticles for Improved Growth and Zn Biofortification in Maize. Arch. Agron. Soil. Sci. 2021, 67, 1164–1176.
- Dapkekar, A.; Deshpande, P.; Oak, M.D.; Paknikar, K.M.; Rajwade, J.M. 3-Getting More Micronutrients from Wheat and Barley through Agronomic Biofortification. In Wheat and Barley Grain Biofortification; Woodhead Publishing Series in Food Science, Technology and Nutrition; Gupta, O.P., Pandey, V., Narwal, S., Sharma, P., Ram, S., Singh, G.P., Eds.; Woodhead Publishing: Duxford, UK, 2020; pp. 53–99.
- Kaur, T.; Rana, K.L.; Kour, D.; Sheikh, I.; Yadav, N.; Kumar, V.; Yadav, A.N.; Dhaliwal, H.S.; Saxena, A.K. Chapter 1—Microbe-Mediated Biofortification for Micronutrients: Present Status and Future Challenges. In New and Future Developments in Microbial Biotechnology and Bioengineering; Rastegari, A.A., Yadav, A.N., Yadav, N., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1–17.
- Prasad, M.; Srinivasan, R.; Chaudhary, M.; Choudhary, M.; Jat, L.K. Chapter Seven-Plant Growth Promoting Rhizobacteria (PGPR) for Sustainable Agriculture: Perspectives and Challenges. In PGPR Amelioration in Sustainable Agriculture; Singh, A.K., Kumar, A., Singh, P.K., Eds.; Woodhead Publishing: Duxford, UK, 2019; pp. 129–157.
- Steiner, G.; Geissler, B.; Schernhammer, E.S. Hunger and Obesity as Symptoms of Non-Sustainable Food Systems and Malnutrition. Appl. Sci. 2019, 9, 1062.
- FAO. Sustainable Food Systems. Available online: https://www.fao.org/3/ca2079en/CA2079EN.pdf (accessed on 19 October 2022).
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022: Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable; The State of Food Security and Nutrition in the World (SOFI); FAO, IFAD, UNICEF, WFP, WHO: Rome, Italy, 2022.
- Salachna, P.; Mizielińska, M.; Płoszaj-Witkowska, B.; Jaszczak, A. Zinc Oxide Nanoparticles Enhanced Biomass and Zinc Content and Induced Changes in Biological Properties of Red Perilla frutescens. Materials 2021, 14, 6182.
- Jha, A.B.; Warkentin, T.D. Biofortification of Pulse Crops: Status and Future Perspectives. Plants 2020, 9, 73.
- van der Straeten, D.; Bhullar, N.K.; De Steur, H.; Gruissem, W.; MacKenzie, D.; Pfeiffer, W.; Qaim, M.; Slamet-Loedin, I.; Strobbe, S.; Tohme, J.; et al. Multiplying the Efficiency and Impact of Biofortification through Metabolic Engineering. Nat. Commun. 2020, 11, 5203.
- Sammauria, R.; Kumawat, S.; Kumawat, P.; Singh, J.; Jatwa, T.K. Microbial Inoculants: Potential Tool for Sustainability of Agricultural Production Systems. Arch. Microbiol. 2020, 202, 677–693.
- Lauriano-Barajas, J.; Vega-Frutis, R. Infectivity and Effectivity of Commercial and Native Arbuscular Mycorrhizal Biofertilizers in Seedlings of Maize (Zea mays). Bot. Sci. 2018, 96, 395–404.
- Sood, G.; Kaushal, R.; Chauhan, A.; Gupta, S. Indigenous Plant-Growth-Promoting Rhizobacteria and Chemical Fertilisers: Impact on Wheat (Triticum aestivum) Productivity and Soil Properties in North Western Himalayan Region. Crop. Pasture Sci. 2018, 69, 460–468.
- Mahapatra, D.M.; Satapathy, K.C.; Panda, B. Biofertilizers and Nanofertilizers for Sustainable Agriculture: Phycoprospects and Challenges. Sci. Total Environ. 2022, 803, 149990.
- Huizar, M.I.; Arena, R.; Laddu, D.R. The Global Food Syndemic: The Impact of Food Insecurity, Malnutrition and Obesity on the Healthspan amid the COVID-19 Pandemic. Prog. Cardiovasc. Dis. 2021, 64, 105–107.
- Tydeman-Edwards, R.; van Rooyen, F.C.; Walsh, C.M. Obesity, Undernutrition and the Double Burden of Malnutrition in the Urban and Rural Southern Free State, South Africa. Heliyon 2018, 4, e00983.
- Monteiro Cordeiro de Azeredo, H.; Monteiro Cordeiro de Azeredo, E. Ultraprocessed Foods: Bad Nutrition or Bad Definition? ACS Food Sci. Technol. 2022, 2, 613–615.
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing Ultra-Processed Foods by Energy Density, Nutrient Density, and Cost. Front. Nutr. 2019, 6, 70.
- Khandpur, N.; Neri, D.A.; Monteiro, C.; Mazur, A.; Frelut, M.-L.; Boyland, E.; Weghuber, D.; Thivel, D. Ultra-Processed Food Consumption among the Paediatric Population: An Overview and Call to Action from the European Childhood Obesity Group. Ann. Nutr. Metab. 2020, 76, 109–113.
- Cunha, D.B.; da Costa, T.H.M.; da Veiga, G.V.; Pereira, R.A.; Sichieri, R. Ultra-Processed Food Consumption and Adiposity Trajectories in a Brazilian Cohort of Adolescents: ELANA Study. Nutr. Diabetes 2018, 8, 28.
- Malik, V.S.; Hu, F.B. The Role of Sugar-Sweetened Beverages in the Global Epidemics of Obesity and Chronic Diseases. Nat. Rev. Endocrinol. 2022, 18, 205–218.
- Guan, B.; Yang, J.; Chen, Y.; Yang, W.; Wang, C. Nutritional Deficiencies in Chinese Patients Undergoing Gastric Bypass and Sleeve Gastrectomy: Prevalence and Predictors. Obes. Surg. 2018, 28, 2727–2736.
- Pellegrini, M.; Rahimi, F.; Boschetti, S.; Devecchi, A.; De Francesco, A.; Mancino, M.V.; Toppino, M.; Morino, M.; Fanni, G.; Ponzo, V.; et al. Pre-Operative Micronutrient Deficiencies in Patients with Severe Obesity Candidates for Bariatric Surgery. J. Endocrinol. Investig. 2021, 44, 1413–1423.
- Asghari, G.; Khalaj, A.; Ghadimi, M.; Mahdavi, M.; Farhadnejad, H.; Valizadeh, M.; Azizi, F.; Barzin, M.; Hosseinpanah, F. Prevalence of Micronutrient Deficiencies Prior to Bariatric Surgery: Tehran Obesity Treatment Study (TOTS). Obes. Surg. 2018, 28, 2465–2472.
- Krzizek, E.-C.; Brix, J.M.; Herz, C.T.; Kopp, H.P.; Schernthaner, G.-H.; Schernthaner, G.; Ludvik, B. Prevalence of Micronutrient Deficiency in Patients with Morbid Obesity Before Bariatric Surgery. Obes. Surg. 2018, 28, 643–648.
- Xiao, S.; Li, Q.; Hu, K.; He, Y.; Ai, Q.; Hu, L.; Yu, J. Vitamin A and Retinoic Acid Exhibit Protective Effects on Necrotizing Enterocolitis by Regulating Intestinal Flora and Enhancing the Intestinal Epithelial Barrier. Arch. Med. Res. 2018, 49, 1–9.
- Harari, A.; Coster, A.C.F.; Jenkins, A.; Xu, A.; Greenfield, J.R.; Harats, D.; Shaish, A.; Samocha-Bonet, D. Obesity and Insulin Resistance Are Inversely Associated with Serum and Adipose Tissue Carotenoid Concentrations in Adults. J. Nutr. 2020, 150, 38–46.
- Apostolakis, M.; Armeni, E.; Bakas, P.; Lambrinoudaki, I. Vitamin D and Cardiovascular Disease. Maturitas 2018, 115, 1–22.
- Plesner, J.L.; Dahl, M.; Fonvig, C.E.; Nielsen, T.R.H.; Kloppenborg, J.T.; Pedersen, O.; Hansen, T.; Holm, J.-C. Obesity Is Associated with Vitamin D Deficiency in Danish Children and Adolescents. J. Pediatr. Endocrinol. Metab. 2018, 31, 53–61.
- Azzi, A. Many Tocopherols, One Vitamin E. Mol. Aspects Med. 2018, 61, 92–103.
- Kardaş, F.; Yücel, A.D.; Kendirci, M.; Kurtoğlu, S.; Hatipoğlu, N.; Akın, L.; Gül, Ü.; Gökay, S.; Üstkoyuncu, P.S. Evaluation of Micronutrient Levels in Children and Adolescents with Obesity and Their Correlation with the Components of Metabolic Syndrome. Turk. J. Pediatr. 2021, 63, 48–58.
- Mosegaard, S.; Dipace, G.; Bross, P.; Carlsen, J.; Gregersen, N.; Olsen, R.K.J. Riboflavin Deficiency—Implications for General Human Health and Inborn Errors of Metabolism. Int. J. Mol. Sci. 2020, 21, 3847.
- Beketova, N.A.; Pavlovskaya, E.V.; Kodentsova, V.M.; Vrzhesinskaya, O.A.; Kosheleva, O.A.; Sokolnikov, A.A.; Strokova, T.V. Biomarkers of vitamin status in obese school children. Vopr. Pitan. 2019, 88, 66–74.
- Lyon, P.; Strippoli, V.; Fang, B.; Cimmino, L. B Vitamins and One-Carbon Metabolism: Implications in Human Health and Disease. Nutrients 2020, 12, 2867.
- Mohapatra, S.; Gangadharan, K.; Pitchumoni, C.S. Malnutrition in Obesity before and after Bariatric Surgery. Dis. Mon. 2020, 66, 100866.
- Adaikalakoteswari, A.; Wood, C.; Mina, T.H.; Webster, C.; Goljan, I.; Weldeselassie, Y.; Reynolds, R.M.; Saravanan, P. Vitamin B12 Deficiency and Altered One-Carbon Metabolites in Early Pregnancy Is Associated with Maternal Obesity and Dyslipidaemia. Sci. Rep. 2020, 10, 11066.
- Haloul, M.; Vinjamuri, S.J.; Naquiallah, D.; Mirza, M.I.; Qureshi, M.; Hassan, C.; Masrur, M.; Bianco, F.M.; Frederick, P.; Cristoforo, G.P.; et al. Hyperhomocysteinemia and Low Folate and Vitamin B12 Are Associated with Vascular Dysfunction and Impaired Nitric Oxide Sensitivity in Morbidly Obese Patients. Nutrients 2020, 12, 2014.
- Williams, A.M.; Guo, J.; Addo, O.Y.; Ismaily, S.; Namaste, S.M.L.; Oaks, B.M.; Rohner, F.; Suchdev, P.S.; Young, M.F.; Flores-Ayala, R.; et al. Intraindividual Double Burden of Overweight or Obesity and Micronutrient Deficiencies or Anemia among Women of Reproductive Age in 17 Population-Based Surveys. Am. J. Clin. Nutr. 2019, 112, 468S–477S.
- Chu, B.A.; Surampudi, V.; Li, Z.; Harris, C.; Seeman, T.; Norris, K.C.; Vijayan, T. Micronutrient Deficiency as a Confounder in Ascertaining the Role of Obesity in Severe COVID-19 Infection. Int. J. Environ. Res. Public Health 2022, 19, 1125.
- Park, S.; Na, W.; Sohn, C. Relationship between Osteosarcopenic Obesity and Dietary Inflammatory Index in Postmenopausal Korean Women: 2009 to 2011 Korea National Health and Nutrition Examination Surveys. J. Clin. Biochem. Nutr. 2018, 63, 211–216.
- Zoroddu, M.A.; Aaseth, J.; Crisponi, G.; Medici, S.; Peana, M.; Nurchi, V.M. The Essential Metals for Humans: A Brief Overview. J. Inorg. Biochem. 2019, 195, 120–129.
- Thillan, K.; Lanerolle, P.; Thoradeniya, T.; Samaranayake, D.; Chandrajith, R.; Wickramasinghe, P. Micronutrient Status and Associated Factors of Adiposity in Primary School Children with Normal and High Body Fat in Colombo Municipal Area, Sri Lanka. BMC Pediatr. 2021, 21, 14.
- Stoffel, N.U.; El-Mallah, C.; Herter-Aeberli, I.; Bissani, N.; Wehbe, N.; Obeid, O.; Zimmermann, M.B. The Effect of Central Obesity on Inflammation, Hepcidin, and Iron Metabolism in Young Women. Int. J. Obes. 2020, 44, 1291–1300.
- Severo, J.S.; Morais, J.B.S.; Beserra, J.B.; Dos Santos, L.R.; de Sousa Melo, S.R.; de Sousa, G.S.; de Matos Neto, E.M.; Henriques, G.S.; do Nascimento Marreiro, D. Role of Zinc in Zinc-ɑ2-Glycoprotein Metabolism in Obesity: A Review of Literature. Biol. Trace Elem. Res. 2020, 193, 81–88.
- Piuri, G.; Zocchi, M.; Della Porta, M.; Ficara, V.; Manoni, M.; Zuccotti, G.V.; Pinotti, L.; Maier, J.A.; Cazzola, R. Magnesium in Obesity, Metabolic Syndrome, and Type 2 Diabetes. Nutrients 2021, 13, 320.
- Podgórska, B.; Wielogórska-Partyka, M.; Godzień, J.; Siemińska, J.; Ciborowski, M.; Szelachowska, M.; Krętowski, A.; Siewko, K. Applications of Metabolomics in Calcium Metabolism Disorders in Humans. Int. J. Mol. Sci. 2022, 23, 10407.
- Sun, M.; Wu, X.; Yu, Y.; Wang, L.; Xie, D.; Zhang, Z.; Chen, L.; Lu, A.; Zhang, G.; Li, F. Disorders of Calcium and Phosphorus Metabolism and the Proteomics/Metabolomics-Based Research. Front. Cell Dev. Biol. 2020, 8, 576110.
- Amin, M.N.; Siddiqui, S.A.; Uddin, M.G.; Ibrahim, M.; Uddin, S.M.N.; Adnan, M.T.; Rahaman, M.Z.; Kar, A.; Islam, M.S. Increased Oxidative Stress, Altered Trace Elements, and Macro-Minerals Are Associated with Female Obesity. Biol. Trace Elem. Res. 2020, 197, 384–393.
- Yamada, S.; Inaba, M. Potassium Metabolism and Management in Patients with CKD. Nutrients 2021, 13, 1751.
- Hatch-McChesney, A.; Lieberman, H.R. Iodine and Iodine Deficiency: A Comprehensive Review of a Re-Emerging Issue. Nutrients 2022, 14, 3474.
- Sorrenti, S.; Baldini, E.; Pironi, D.; Lauro, A.; D’Orazi, V.; Tartaglia, F.; Tripodi, D.; Lori, E.; Gagliardi, F.; Praticò, M.; et al. Iodine: Its Role in Thyroid Hormone Biosynthesis and Beyond. Nutrients 2021, 13, 4469.
- de Angelis, S.; Bagnasco, M.; Moleti, M.; Regalbuto, C.; Tonacchera, M.; Vermiglio, F.; Medda, E.; Rotondi, D.; Di Cosmo, C.; Dimida, A.; et al. Obesity and Monitoring Iodine Nutritional Status in Schoolchildren: Is Body Mass Index a Factor to Consider? Thyroid 2021, 31, 829–840.
- Ying, H.; Zhang, Y. Systems Biology of Selenium and Complex Disease. Biol. Trace Elem. Res. 2019, 192, 38–50.
- Soares de Oliveira, A.R.; Jayanne Clímaco Cruz, K.; Beatriz Silva Morais, J.; Rocha Dos Santos, L.; Rodrigues de Sousa Melo, S.; Fontenelle, L.C.; Santos de Sousa, G.; Costa Maia, C.S.; Oliveira Duarte de Araújo, C.; Leal Mendes, I.; et al. Selenium Status and Oxidative Stress in Obese: Influence of Adiposity. Eur. J. Clin. Invest. 2021, 51, e13538.
- Chen, J.; Jiang, Y.; Shi, H.; Peng, Y.; Fan, X.; Li, C. The Molecular Mechanisms of Copper Metabolism and Its Roles in Human Diseases. Pflugers Arch. 2020, 472, 1415–1429.
- Meyer Mikalsen, S.; Aaseth, J.; Flaten, T.P.; Whist, J.E.; Bjørke-Monsen, A.-L. Essential Trace Elements in Norwegian Obese Patients before and 12 Months after Roux-En-Y Gastric Bypass Surgery: Copper, Manganese, Selenium and Zinc. J. Trace Elem. Med. Biol. 2020, 62, 126650.
- Vivek, S.M.; Dayal, D.; Khaiwal, R.; Bharti, B.; Bhalla, A.; Singh, S.; Kaur, H.; Attri, S.V. Low Serum Copper and Zinc Concentrations in North Indian Children with Overweight and Obesity. Pediatr. Endocrinol. Diabetes Metab. 2020, 26, 79–83.
- PAHO. Micronutrientes. Available online: https://www.paho.org/en/topics/micronutrients (accessed on 3 October 2022).
