Axial spondyloarthritis (axSpA) is a chronic inflammatory disease that can lead to ankylosis by secondary ossification of inflammatory lesions, with progressive disability and a significant impact on quality of life. It is also a risk factor for the occurrence of comorbidities, especially cardiovascular diseases (CVDs), mood disorders, osteoporosis, and malignancies. Early diagnosis and treatment are needed to prevent or decrease functional decline and to improve the patient’s prognosis. In respect of axSpA, there is an unmet need for biomarkers that can help to diagnose the disease, define disease activity and prognosis, and establish personalized treatment approaches. The aim of this review was to summarize the available information regarding the most promising biomarkers for axSpA. It can bWe classified and identified six core categories of biomarkers: (i) systemic markers of inflammation; (ii) molecules involved in bone homeostasis; (iii) HLA-B27 and newer genetic biomarkers; (iv) antibody-based biomarkers; (v) microbiome biomarkers; and (vi) miscellaneous biomarkers. Unfortunately, despite efforts to validate new biomarkers, few of them are used in clinical practice; however, we believe that these studies provide useful data that could aid in better disease management.
1. Axial Spondyloarthritis: Past, Present, and Future
Spondyloarthritis (SpA) comprises a group of chronic immune-mediated inflammatory conditions with overlapping clinical and genetic features but with substantial heterogeneity, as inflammation can affect peripheral and axial joints and also result in extraarticular manifestations (enthesitis, dactylitis, uveitis, inflammatory bowel disease, psoriasis)
[1][2][3][1,2,3].
SpA comprises a spectrum of diseases with significant overlaps between SpA phenotypes, which can be classified according to the Assessment of Spondyloarthritis International Society (ASAS) 2009 classification criteria. These depend on where patients primarily experience symptoms in axial SpA (axSpA) with predominantly axial manifestations, including non-radiographic (nr-axSpA) and radiographic axSpA (r-axSpA) or ankylosing spondylitis (AS) and peripheral SpA (pSpA) with predominant peripheral involvement (psoriatic arthritis, reactive arthritis, enteropathic arthritis, juvenile-onset SpA, and undifferentiated SpA)
[4]. While the spectrum of axSpA extends from early or mild disease through severe or late disease with erosive damage in the sacroiliac joints, this arbitrary division of nr-axSpA and r-axSpA is becoming less clinically relevant.
The symptoms of axSpA create a significant burden for both patients and society. The major disease feature is the progression to ankylosis by secondary ossification of inflammatory lesions, with progressive disability and a significant impact on quality of life.
AxSpA is also a risk factor for the occurrence of comorbidities, especially cardiovascular diseases (CVDs), mood disorders, osteoporosis, and malignancies, which shows that axSpA has a systemic character and influences patient health in a complex manner
[2]. All these characteristics affect quality of life and, because all comorbidity types correlate with axSpA, early diagnosis and treatment are needed to prevent or decrease functional decline and improve the patient’s prognosis.
2. AxSpA and Biomarkers
According to the World Health Organization, a biomarker is a chemical, physical, or biological indicator of disease presence, activity, or severity, which can provide vital information. In respect of axSpA, there is an unmet need for biomarkers that can help to diagnose the disease, define disease activity and prognosis, and establish personalized treatment approaches
[5].
Despite the progress made in the concept of axSpA, its identification remains challenging, frequently resulting in a diagnostic delay for patients. Ideally, the diagnosis should be made before the development of radiographic sacroiliitis, but currently the most sensitive imaging diagnosis method is magnetic resonance imaging (MRI), which is costly and not widely available
[2].
AxSpA disease activity is monitored using the following scores: Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), and Ankylosing Spondylitis Disease Activity Score (ASDAS), which may be subjective. Disease activity is also monitored by measuring of one of the most common inflammatory biomarkers, C-reactive protein (CRP), which is insensitive for this disease
[6].
Although the range of effective modern drugs for axSpA has expanded in recent decades, therapeutic decisions and the response to specific therapies remain challenges in current practice, and further research is therefore required. Adequate evaluation of disease activity, radiographic progression, response to treatment and identification of negative prognostic factors can improve the therapeutic decision. In addition, data regarding the axSpA prognosis obtained in the early disease stages will improve therapeutic management
[2].
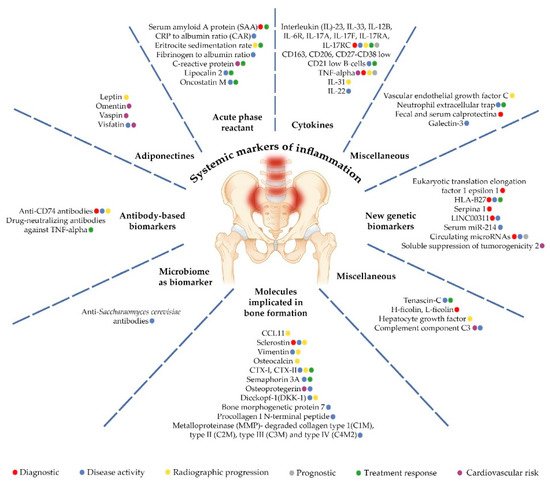
The aim of was to summarize available information regarding the most promising biomarkers for axSpA. The researchers further refer to six core categories of biomarkers: (i) systemic markers of inflammation; (ii) molecules involved in bone homeostasis; (iii) HLA-B27 and newer genetic biomarkers; (iv) antibody-based biomarkers; (v) microbiome biomarkers; and (vi) miscellaneous biomarkers (Table 1, Figure 1). Furthermore, the association between biomarkers and diagnosis, disease activity, structural damage, and treatment response are described below.
Figure 1.
Biomarkers significance in axial spondiloarthtitis.
Table 1.
Biomarkers significance in axial spondyloarthritis.