Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Alexandre Gonzalez-Rodriguez and Version 3 by Rita Xu.
Delusional disorder (DD) has been considered a treatment-resistant disorder, with antipsychotics acknowledged as the best. It is possible that the discovery of the right drug could turn treatment resistance into treatment response.
- optimizing treatment
- schizophrenia spectrum
- pimozide
1. Introduction
The first extensive description of monomania, also called paranoia, was generated by the French psychiatrist Esquirol (1772–1840). He labeled this form of mental illness a partial “délire” (French for delusion), partial because, outside of the one prominent, fiercely defended, idiosyncratic, and unchangeable false belief, the patient was generally described as fully rational [1]. The term paranoia was widely used in psychiatry until the first half of the 20th century, after which it lost its status as a stand-alone diagnosis [2]. In 1987, DSM-III-R (the revision of the third U.S. diagnostic and statistical manual of mental disorders) reintroduced the concept but gave it a new name: delusional disorder [3]. Delusional disorder (DD) is considered a serious mental disorder characterized by the presence of a fixed, preoccupying, illogical belief. It is classified as a psychotic disorder, and belongs to the schizophrenia spectrum of disorders [4]. Characteristically, delusional beliefs are based on the misinterpretation of external reality, and are not, by definition, amenable to extinction by persuasion or education [5]. Delusions in DD are sometimes accompanied by affective symptoms or perception errors; however, even when present, these do not take center stage. Whenever hallucinations do occur in DD, they are congruent with the all-consuming delusional theme [5]. The current diagnostic and statistical manuals for mental disorders classify DD into seven subtypes according to the delusional content: persecutory (belief of being persecuted or conspired against), somatic (delusional parasitosis, hypochondriasis, or body dysmorphic disorder), jealous (Othello’s syndrome), grandiose (delusions of grandeur), erotomanic (de Clérambault’s syndrome), mixed (a combination of delusional themes), and unspecified (vagueness in the expression of delusional content) [5]. These subtypes are not associated in the psychiatric literature with differential responses to available treatments.
The worldwide prevalence of DD is difficult to determine accurately because many persons with DD do not consider themselves ill, and thus, never seek treatment. The condition has been considered rare, representing only 1–4% of all psychiatric admissions. It usually never comes to medical attention until middle or late adult life, although it may begin earlier [2][6][2,6]. There are reports of DD being consistently and cross-culturally most common in low socioeconomic groups and among new immigrants. In fact, DD occurs more frequently in immigrants than schizophrenia or affective disorder [6]; except for specific local syndromes, the sociodemographic profile is consistent across different cultures [7].
2. Treatment of Delusional Disorder Prior to the Widespread Use of Antipsychotic Medications
Before the introduction of antipsychotic medications, patients with schizophrenia and other paranoid psychoses were treated in long-term psychiatric institutions, where the emphasis was on keeping patients safe, calm, and busy. Treatment focused on safety precautions, occupational activities, and nursing care [8][11]. Gardening, art, music, drama, and dance therapies were some of the therapeutic modalities used in mental hospitals. Dance movement therapy was also used to improve psychological and physical well-being [9][12]. The mechanism by which leisure activities could improve psychotic symptoms was understudied. It was assumed that such activities were enjoyable and relaxing, encouraged in-hospital socialization, and kept patients’ minds off pathological preoccupations. Work therapy, rest cures, and a system of rewards for appropriate behavior were also offered in psychiatric asylums. Rest cures included three main elements: rest, seclusion, and good nutrition. Massage treatment was sometimes used [10][13]. Malaria treatment, insulin shock, lobotomy, and electroconvulsive therapy, plus three types of hydrotherapy, were the main treatments for psychosis [11][14]. Hydrotherapy was described as head-out hot showers, adapted cold showers, and colonic hydrotherapy. It was hypothesized that hot and cold showers reduce stress and potentially modulate neurotransmission via the mesolimbic system of the brain. Pharmaceutical compounds such as bromides, chloral hydrate, hyoscine, paraldehyde, barbiturates, and morphine were also used for sedation. Even after the introduction of chlorpromazine, paraldehyde was still in use as a comparator drug, specifically for toxic psychosis and delirium tremens [12][13][15,16]. Table 1 represents the main treatment options used to treat patients with psychosis, including DD, before the widespread use of chlorpromazine and related drugs.Table 1. Treatment of delusional disorder before the introduction of antipsychotics.
| Treatment for Psychosis Prior to Chlorpromazine | ||
|---|---|---|
| Asylum Care | Procedures | Pharmaceuticals |
| Gardening | Malaria treatment | bromides |
| Art/Music | Freeze wraps | chloral hydrate |
| Dance/Theatre | Hydrotherapy | hyoscine |
| Rest cures | Insulin shock | paraldehyde |
| Token economy | Lobotomy | barbiturates |
| Work therapy | Electroconvulsive therapy | morphine |
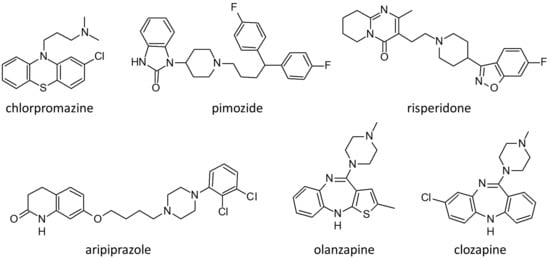
Figure 1. Molecular structure of the main antipsychotics used to treat patients with delusional disorders.
Table 2. Development of first- and second-generation antipsychotic medications.
| First-Generation Antipsychotics |
Second-Generation Antipsychotics, Including Partial D2 Agonists | |||||
|---|---|---|---|---|---|---|
| 1952 | 1960s | 1970s | 1980s | 1990s | 2000s | 2010s |
| CPZ | Halo Perph Fluph Thio Loxap Triflu |
Pimoz | Cloz | Risp Olan Quet Zipr |
Aripip Palip Iloper |
Asena Luras Caripr |
Abbreviations: CPZ–chlorpromazine; Halo–haloperidol; Perph–perphenazine; Fluph–fluphenazine; Thio–thioridazine; Loxap–loxapine; Cloz–clozapine; Risp–risperidone; Olan–olanzapine; Quet–quetiapine; Zipr–ziprasidone; Aripip–aripiprazone; Luras–lurasidone; Caripr-cariprazine.
3. Use of Pimozide in the Treatment of Delusional Disorder
Pimozide is an antipsychotic belonging to the diphenylbutylpiperidine class, synthesized in 1963 by pharmacologic giant, Paul Janssen. After the immense success of haloperidol, the understanding that dopamine receptor blockade was central to antipsychotic action led to the development of more butyrophenones. Serotonin antagonism subsequently emerged as contributory to the alleviation of psychotic symptoms, which led to the synthesis of pimozide, an antagonist at the D2, D3, and D4 receptors and the 5-HT7 receptor [21][24]. In 1975, Riding and Munro treated four cases of monosymptomatic hypochondriacal psychosis (DD somatic type) with pimozide [22][25]. Three of the four responded well, while the fourth showed partial improvement. Canadian psychiatrist Alistair Munro subsequently became a world leader in the treatment of delusional disorder [23][26], and advocated for the use of pimozide because of its specific effectiveness, especially, Munro believed, for somatic delusions such as delusional parasitosis [24][27]. Munro argued that, in DD, no matter the central delusional theme, the core distinction from other forms of psychosis is that the delusions are encapsulated. Though very firmly held, the delusions do not affect the entirety of a person’s life. In that sense, all themes are alike, hence there is no reason for one subtype to respond to a treatment when other subtypes do not. His explanation for the seemingly superior response of the somatic type to pimozide was that persons with somatic symptoms are more likely than others to adhere to treatment. Adherence rather than delusional content, according to Munro, was what determined response. Subsequent studies have generally agreed with this conclusion.
As well as the effects noted above, pimozide also displays actions as an antagonist, inverse agonist, and channel blocker, with relatively lower affinities, at α-adrenergic, muscarinic cholinergic, and histamine receptors and calcium and sodium channels.
Like many other antipsychotics, but more strongly than most, pimozide also inhibits the hERG (human ether-a-go-go-related) K+ channel [25][28]. It is the hERG block that leads to QT interval prolongation and ventricular arrhythmias, including torsades de pointes. Despite its effectiveness and advantages as an antipsychotic medication (relatively little sedation and little weight gain), it is this cardiac effect that has led to its decline in use [26][29]. As for its special effectiveness in delusional disorder, the Cochrane Review of 26 studies on pimozide in 2013 concluded that there were insufficient data to either support or refute this claim [21][24].
4. Use of Second-Generation Antipsychotics in the Treatment of Delusional Disorder
Blocking dopamine transmission at the postsynaptic receptor site is regarded as a critical action of antipsychotics. Another is the blockade of dopamine synthesis at the level of the presynaptic neuron. A longitudinal study carried out by Pomarol-Clotet and colleagues [27][33] examined the latter hypothesis in a group of 11 patients with DD, and 12 with schizophrenia, following a 3 month treatment period with second-generation antipsychotics. Baseline striatal dopamine synthesis was inversely associated with negative symptoms in first-episode schizophrenia, but this was not apparent in DD, which is not surprising since negative symptoms (apathy, avolition, paucity of speech, social isolation) are uncharacteristic of DD. Cheng et al. [28][34] explored dopamine synthesis capacity in 12 patients with schizophrenia, 11 with DD, and 12 diagnosed with other psychotic disorders. They compared results against those of 19 healthy controls. Assessment was performed using 18F-DOPA positron emission tomography (PET) and magnetic resonance imaging (MRI); psychopathological symptoms were assessed with the positive and negative syndrome scale (PANSS). The findings were that DD, schizophrenia, and related disorders all presented similar dysregulated mechanisms of dopamine synthesis, which implies that treatment with dopamine antagonists should affect all psychotic diagnostic categories to the same degree, at least if the blockade of dopamine synthesis is the main mechanism of action.
Recently, as mentioned earlier, Guàrdia et al. [29][10] reviewed studies of DD patients treated with second-generation drugs, and found evidence for effects on both dopamine and serotonin pathways, as well as on the mediation of brain structure impairment, particularly in temporal and parietal lobes, on drug efficacy. The implication is that older age (and thus older brains) among DD patients, compared to those with schizophrenia, may impact the response to specific therapeutic drugs and affect the dose range needed for efficacy and tolerability [3][4][3,4]. The hypothesis that serotonin pathways are important in antipsychotic action was what led to the synthesis of second-generation antipsychotics. Because they are less likely than first-generation drugs to induce extrapyramidal adverse effects, they may be especially useful for older patients.
With a particular focus on late life, Nagendra and Snowdon described consecutive cases of DD in patients referred to an old age psychiatry service [30][35]. Ninety-six patients received second-generation antipsychotics, and the overall response was considered positive. This suggests that second-generation drugs show superior efficacy over first-generation drugs, but these results cannot be considered as evidence. The separation between the two generations is somewhat artificial. Second-generation drugs, as a group, cause minimal extrapyramidal effects and minimal hyperprolactinemia because of greater serotonin receptor blockade and lower duration of time attached to the postsynaptic D2 receptor. Risperidone, however, classed as a second-generation drug, frequently produces extrapyramidal effects and high levels of prolactin, even at low doses.
4.1. Risperidone
The vast majority of evidence on the efficacy of antipsychotic treatment of DD comes from the use of risperidone. Positive response to risperidone has been reported in patients with DD of the somatic type and other DD subtypes [31][32][36,37]. This drug is chiefly metabolized by CYP2D6. A case report by Strauss and collaborators rightly highlighted the relevance of genetic variants of CYP2D6 when treating DD with risperidone [33][38]. The patient was a 37-year-old woman who was a poor metabolizer of risperidone, and in whom a very low dose proved toxic. A previous study investigated the clinical response to risperidone by determining plasma concentrations of the drug, catecholamine metabolites, and CYP2D6 genotypes in a sample of 136 patients with schizophrenia, DD, and schizoaffective disorder [34][39]. This researchtudy found a positive association between plasma levels of risperidone plus 9-hydroxirisperidone (an active metabolite) and Simpson and Angus score (SAS), a measure of extrapyramidal effects. However, no correlations were found between antipsychotic plasma levels and PANSS scores, both of which are measures of effectiveness. Monitoring antipsychotic plasma levels may be useful when patients experience unexpectedly severe side effects from antipsychotics in general [32][37].
4.2. Olanzapine
There are recent studies on the efficacy of olanzapine in DD. Comardelle et al. [35][40] published the case of a 67-year-old woman with a delusion of glass in her hands and fingernails. The patient was successfully treated with olanzapine 5 mg per day in combination with psychotherapy. Freudenmann et al. and Bosmans and Verbanck [36][37][41,42] both reported on patients with DD who responded well to very low doses of olanzapine. Both patients were elderly and suffered from delusional parasitosis. As suggested by Munro, somatic discomfort may have enhanced adherence.
Kulkarni et al. carried out a retrospective analysis of 455 patients suffering from DD [38][43]. The sample was divided into two groups according to the treatment received. The first group consisted of 86 patients on olanzapine, and the second of 280 patients on risperidone. Both risperidone and olanzapine were found to be effective, with no statistically significant differences between the groups in either adherence or response to treatment. Both risperidone and olanzapine are known to have side effects (extrapyramidal symptoms in the case of risperidone, and weight gain in the case of olanzapine), which could interfere with adherence. What often determines adverse effect severity is the pace of dose increase at the beginning of treatment, as well as the daily dose ultimately reached, although individual patient sensitivities to side effects are also important.
Basu et al. reported the case of a 38-year-old woman diagnosed with DD who developed restless leg syndrome (RLS) on olanzapine [39][44], a sleep disorder commonly associated with the use of first-generation antipsychotics. When risperidone was substituted for olanzapine, the RLS improved. This is surprising because extrapyramidal effects are usually more prevalent with risperidone than with olanzapine, which highlights the importance of individual sensitivities. By contrast, a switch from trifluoperazine to olanzapine improved tardive dyskinesia in a 59-year-old man with DD [40][45]; however, the olanzapine daily dose was 17.5 mg/d, which is a high dose that may have ‘covered’ tardive movements. Dose is usually more relevant to side effect severity than the choice of antipsychotic.
4.3. Quetiapine
Quetiapine, another popular second-generation drug, has affinity for D2 receptors, serotonergic receptors, and alpha 1 and histaminergic receptors, but, as with most other antipsychotics, mainly works via dopamine and serotonin pathways. Prakash et al. [41][46] reported on a 29-year-old man suffering from DD and von Hippel–Lindau disease, a hereditary condition associated with tumors in multiple organs. The patient was treated with quetiapine 50 mg daily, which was progressively increased to 200 mg/day. Total remission of delusional symptoms was achieved. It is interesting to note that effective doses of quetiapine for schizophrenia need to be substantially higher than 200 mg/day [42][47], bringing forward the possibility that patients with DD, on average, do not require doses as high as those used in schizophrenia treatment.
4.4. Paliperidone
Paliperidone, or 9-OH-risperidone, is the main metabolite of risperidone, and comes as an extended-release (long-acting) tablet to be taken qAM. Paliperidone palmitate is also available in long-acting injectable form. Altinöz et al. [43][48] reported two cases of elderly patients with delusional parasitosis whose symptoms remitted after treatment with oral paliperidone; neither one experienced side effects. One patient concluded that the paliperidone had “poisoned the parasites”. The reason specific drugs work for specific patients has been attributed to individual genetics.
4.5. Asenapine
Asenapine is a relatively new drug that shows high affinity for serotonergic receptors, adrenoceptors, dopamine receptors, and histamine receptors. A case report by Rajkumar et al. [44][49] described a 44-year-old woman with a chronic and systematized delusion of jealousy. She showed a poor response to aripiprazole (a dopamine partial agonist) at 15 mg a day for 2 months. Consequently, she was changed to ziprasidone, 80–100 mg/day for 10 months. Delusions of jealousy faded, but new persecutory delusions appeared, perhaps precipitated by side effects, i.e., perioral and lingual dyskinetic movements. This combination of new symptoms and dyskinetic movements led to a diagnosis of supersensitivity psychosis, a known complication of long-term antipsychotic treatment, in which patients develop new psychotic symptoms, often accompanied by tardive dyskinesia. The syndrome, first described in 1980 by Canadian psychiatrist Guy Chouinard [45][50], is attributable to prolonged dopamine receptor blockade. Asenapine was chosen as the next treatment based on the belief that, because of its potent serotonin 5-HT2A receptor antagonism, it might be able to reduce D2 receptor supersensitivity. After the switch to asenapine 20 mg/day, the patient went into complete remission of psychotic symptoms, and showed no dyskinetic movements. The trouble with case histories, however, is that only successful cases are reported. Asenapine may or may not be indicated in supersensitivity psychosis. Replication is needed.
4.6. Ziprasidone
Ziprasidone use in DD has been reported in a few cases [44][46][49,51], most often targeted at the somatic subtype of DD. Contreras-Ferrer et al. [47][52] reported the case of a 73-year-old woman referred to dermatology because of deep linear ulcers on the face and arms secondary to pruritis and scratching. Delusional parasitosis was suspected. Outpatient treatment with olanzapine was not effective, thus, a combination of pimozide, ziprasidone, and dantrolene (an anticholinergic for side effects) was started in hospital. After 2 weeks on this regimen, the delusion disappeared. It may have been the separation from her family (who also believed in the parasitic infestation) that effected the cure rather than the pharmaceuticals. De Berardis et al. [48][53] reported the case of a 24-year-old woman who also presented with delusions of parasitosis, and was treated with ziprasidone 120 mg daily. Ziprasidone was chosen because the patient asked for a drug that would not lead to weight gain. After 1 month of treatment, the patient’s delusion began to fade, and she went into complete remission. Ziprasidone has a unique pattern of receptor affinity, and delusional parasitosis has been hypothesized to result from specific pathophysiology [49][54]. A good match between patient and drug could be what led to treatment success. This is contrary to the consensus that all monothematic delusions respond in the same way, but possibilities that correct matching is important to drug efficacy, such as suggested by this case history, deserve further investigation.
