Breast cancer (BC) is the most common cancer among women worldwide and represents one of the leading causes of mortality and morbidity. Neoadjuvant chemotherapy (NACT) is a systemic treatment administered before surgery, whose indications have expanded from inoperable locally advanced to early-stage breast cancer. The pivotal role of magnetic resonance imaging (MRI) with morphological and functional modalities is making headway in the assessment of tumor size in the staging, residual tumor, surgical planning and prediction of response. Radiomics and radiogenomics MRI applications in the setting of breast cancer NACT response prediction are continuously increasing. Tailored systemic therapy strategies allow considerations of treatment de-escalation in excellent responders and avoiding or at least postponing breast surgery in selected patients.
- early-stage breast cancer
- magnetic resonance imaging
- neoadjuvant chemotherapy
- pathological complete response
1. Early Prediction of Pathological Outcome after Neoadjuvant Chemotherapy
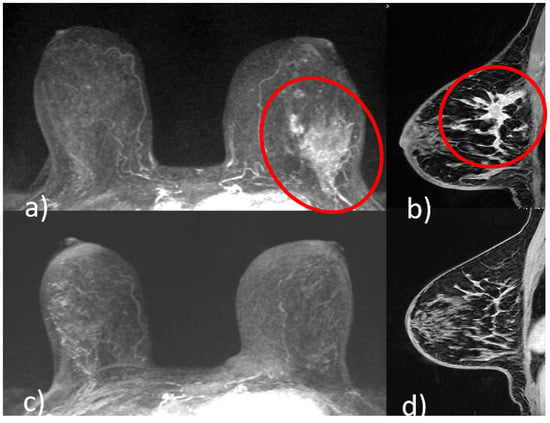
1.1. Morphological Characteristics
1.2. Background Parenchyma Enhancement (BPE)
1.3. Diffusion Weighted Imaging (DWI) and Apparent Diffusion Coefficient (ADC)
1.4. Triple Negative Breast Cancer
1.5. What’s New (Radiomics, Machine Learning and Radiogenomics)
2. The Role of MRI in the Preoperative Assessment of Residual Disease and Pathological Complete Response (pCR)
2.1. Pattern of Tumor Response
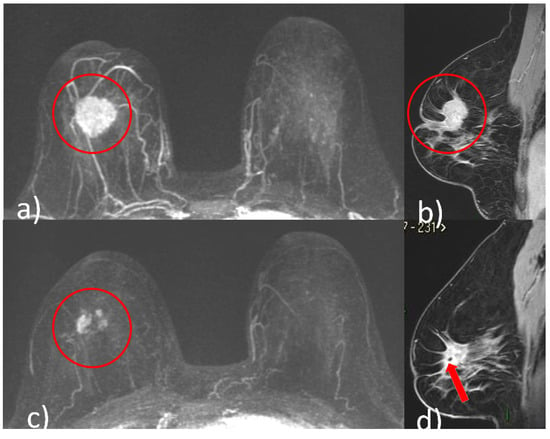
2.2. Impact on Therapy and surgical planning
Moreover, in patients with excellent response to NACT and subsequent pCR, it is oncologically safe to de-escalate treatment [22][61][62]. Accurate tailoring of NACT allows consideration of individualized locoregional treatment strategies. Heil et al. [63] put it to the extreme: they proposed to postpone or avoid breast surgery, trying a “watch and see” strategy, in patients that showed pCR at the end of NACT. This patients are very unlikely to face distant recurrence, indeed; in contrast, minimal residual pathology with subsequent risk of local relapse is still possible. Studies are currently underway to identify pCR, using barely invasive biopsies in women who have had partial/complete radiologic response after treatment, in order to stratify low-risk patients [64].
In addition, there may also be subset of patients who do not benefit from surgery after treatment; however, there is currently insufficient scientific evidence. Therefore, several questions remain unsolved, and it remains a great challenge for the future to conduct high-quality clinical trials that can answer these questions [62].
References
- Romeo, V.; Accardo, G.; Perillo, T.; Basso, L.; Garbino, N.; Nicolai, E.; Maurea, S.; Salvatore, M. Assessment and prediction of response to neoadjuvant chemotherapy in breast cancer: A comparison of imaging modalities and future perspectives. Cancers 2021, 13, 3521.
- Tsunoda-Shimizu, H.; Hayashi, N.; Hamaoka, T.; Kawasaki, T.; Tsugawa, K.; Yagata, H.; Kikuchi, M.; Suzuki, K.; Nakamura, S. Determining the morphological features of breast cancer and predicting the effects of neoadjuvant chemotherapy via diagnostic breast imaging. Breast Cancer 2008, 15, 133–140.
- Tsukada, H.; Tsukada, J.; Schrading, S.; Strobel, K.; Okamoto, T.; Kuhl, C.K. Accuracy of multi-parametric breast MR imaging for predicting pathological complete response of operable breast cancer prior to neoadjuvant systemic therapy. Magn. Reson. Imaging 2019, 62, 242–248.
- Thompson, B.M.; Chala, L.F.; Shimizu, C.; Mano, M.S.; Filassi, J.R.; Geyer, F.C.; Torres, U.S.; Guedes Netto de Mello, G.; da Costa Leite, C. Pre-treatment MRI tumor features and post-treatment mammographic findings: May they contribute to refining the prediction of pathologic complete response in post-neoadjuvant breast cancer patients with radiologic complete response on MRI? Eur. Radiol. 2022, 32, 1663–1675.
- Choi, W.J.; Kim, H.H.; Cha, J.H.; Shin, H.J.; Chae, E.Y.; Yoon, G.Y. Complete response on MR imaging after neoadjuvant chemo- therapy in breast cancer patients: Factors of radiologic-pathologic discordance. Eur. J. Radiol. 2019, 118, 114–121.
- Choi, J.S.; Ko, E.S.; Ko, E.Y.; Han, B.K.; Nam, S.J. Background parenchymal enhancement on preoperative magnetic resonance imaging: Association with recurrence-free survival in breast cancer patients treated with neoadjuvant chemotherapy. Medicine 2016, 95, 1–9.
- Kim, S.A.; Cho, N.; Ryu, E.B.; Seo, M.; Bae, M.S.; Chang, J.M.; Moon, W.K. Background parenchymal signal enhancement ratio at preoperative mr imaging: Association with subsequent local recurrence in patients with ductal carcinoma in situ after breast conservation surgery. Radiology 2014, 270, 699–707.
- Lee, J.; Kim, S.H.; Kang, B.J. Pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: Perfusion metrics of dynamic contrast enhanced MRI. Sci. Rep. 2018, 8, 1–8.
- Preibsch, H.; Wanner, L.; Bahrs, S.D.; Wietek, B.M.; Siegmann-Luz, K.C.; Oberlecher, E.; Hahn, M.; Staebler, A.; Nikolaou, K.; Wiesinger, B. Background parenchymal enhancement in breast MRI before and after neoadjuvant chemotherapy: Correlation with tumour response. Eur. Radiol. 2016, 26, 1590–1596.
- Chen, J.H.; Yu, H.J.; Hsu, C.; Mehta, R.S.; Carpenter, P.M.; Su, M.Y. Background parenchymal enhancement of the contralateral normal breast: Association with tumor response in breast cancer patients receiving neoadjuvant chemotherapy. Transl. Oncol. 2015, 8, 204–209.
- Rella, R.; Bufi, E.; Belli, P.; Scrofani, A.R.; Petta, F.; Borghetti, A.; Marazzi, F.; Valentini, V.; Manfredi, R. Association between contralateral background parenchymal enhancement on MRI and outcome in patients with unilateral invasive breast cancer breast receiving neoadjuvant chemotherapy. Diagn. Interv. Imaging 2022, 103, 486–494.
- Taourel, P.; Pages, E.; Millet, I.; Bourgier, C.; Rouanet, P.; Jacot, W.; Crochet, P.; Azria, D. Magnetic resonance imaging in breast cancer management in the context of neo-adjuvant chemotherapy. Crit. Rev. Oncol. Hematol. 2018, 132, 51–65.
- Choi, B.B. Effectiveness of ADC Difference Value on Pre-neoadjuvant Chemotherapy MRI for Response Evaluation of Breast Cancer. Technol. Cancer Res. Treat. 2021, 20, 153303382110391.
- Park, S.H.; Moon, W.K.; Cho, N.; Song, I.C.; Chang, J.M.; Park, I.; Han, W.; Dong-Young Noh, D.-Y. Diffusion-weighted MR imaging: Pretreatment prediction of response to neoadjuvant chemotherapy in patients with breast cancer. Radiology 2010, 257, 56–63.
- Suo, S.; Yin, Y.; Geng, X.; Zhang, D.; Hua, J.; Cheng, F.; Chen, J.; Zhuang, Z.; Cao, M.; Xu, J. Diffusion-weighted MRI for predicting pathologic response to neoadjuvant chemotherapy in breast cancer: Evaluation with mono-, bi-, and stretched-exponential models. J. Transl. Med. 2021, 19, 1–12.
- Bufi, E.; Belli, P.; Costantini, M.; Cipriani, A.; Di Matteo, M.; Bonatesta, A.; Franceschini, G.; Terribile, D.; Mulé, A.; Nardone, L.; et al. Role of the Apparent Diffusion Coefficient in the Prediction of Response to Neoadjuvant Chemotherapy in Patients with Locally Advanced Breast Cancer. Clin. Breast Cancer 2015, 15, 370–380.
- Richard, R.; Thomassin, I.; Chapellier, M.; Scemama, A.; de Cremoux, P.; Varna, M.; Giacchetti, S.; Espié, M.; de Kerviler, E.; de Bazelaire, C.; et al. Diffusion-weighted MRI in pretreatment prediction of response to neoadjuvant chemotherapy in patients with breast cancer. Eur. Radiol. 2013, 23, 2420–2431.
- Meisamy, S.; Bolan, P.J.; Baker, E.H.; Bliss, R.L.; Gulbahce, E.; Everson, L.I.; Nelson, M.T.; Emory, T.H.; Tuttle, T.M.; Yee, D.; et al. Neoadjuvant chemotherapy of locally advanced breast cancer: Predicting response with in vivo (1) H MR spectroscopy–a pilot study at 4 T. Radiology 2004, 233, 424–431.
- Sah, R.G.; Sharma, U.; Parshad, R.; Seenu, V.; Mathur, S.R.; Jagannathan, N.R. Association of estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 status with total choline concentration and tumor volume in breast cancer patients: An MRI and in vivo proton MRS study. Magn. Reson. Med. 2012, 68, 1039–1047.
- Bolan, P.J.; Kim, E.; Herman, B.A.; Newstead, G.M.; Rosen, M.A.; Schnall, M.D.; Pisano, E.D.; Weatherall, P.T.; Morris, E.A.; Lehman, C.D. ACRIN Trial team ISPY-1 Investigators. MR spectroscopy of breast cancer for assessing early treatment response: Results from the ACRIN 6657 MRS trial. J. Magn. Reson. Imaging 2017, 46, 290–302.
- Houssami, N.; MacAskill, P.; Von Minckwitz, G.; Marinovich, M.L.; Mamounas, E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur. J. Cancer 2012, 48, 3342–3354.
- Van Ramshorst, M.S.; van der Voort, A.; van Werkhoven, E.D.; Mandjes, I.A.; Kemper, I.; Dezentjé, V.O.; Oving, I.M.; Honkoop, A.H.; Tick, L.W.; van de Wouw, A.J.; et al. Dutch Breast Cancer Research Group (BOOG). Neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2 blockade for HER2-positive breast cancer (TRAIN-2): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2018, 19, 1630–1640.
- Bae, M.S.; Shin, S.U.; Ryu, H.S.; Han, W.; Im, S.A.; Park, I.A.; Noh, D.Y.; Moon, W.K. Pretreatment MR imaging features of triple-negative breast cancer: Association with response to neoadjuvant chemotherapy and recurrence-free survival. Radiology 2016, 281, 392–400.
- Harada, T.L.; Uematsu, T.; Nakashima, K.; Sugino, T.; Nishimura, S.; Takahashi, K.; Hayashi, T.; Tadokoro, Y.; Watanabe, J.; Nakamoto, S.; et al. Is the presence of edema and necrosis on T2WI pretreatment breast MRI the key to predict pCR of triple negative breast cancer? Eur. Radiol. 2020, 30, 3363–3370.
- Abdelhafez, A.H.; Musall, B.C.; Adrada, B.E.; Hess, K.; Son, J.B.; Hwang, K.P.; Candelaria, R.P.; Santiago, L.; Whitman, G.J.; Le-Petross, H.T.; et al. Tumor necrosis by pretreatment breast MRI: Association with neoadjuvant systemic therapy (NAST) response in triple-negative breast cancer (TNBC). Breast Cancer Res. Treat. 2021, 185, 1–12.
- Kawashima, H.; Inokuchi, M.; Furukawa, H.; Kitamura, S. Triple-negative Breast Cancer. Are the Imaging Findings Different Between Responders and Nonresponders to Neoadjuvant Chemotherapy? Acad. Radiol. 2011, 18, 963–969.
- Li, Y.; Chen, Y.; Zhao, R.; Ji, Y.; Li, J.; Zhang, Y.; Lu, H. Development and validation of a nomogram based on pretreatment dynamic contrast-enhanced MRI for the prediction of pathologic response after neoadjuvant chemotherapy for triple-negative breast cancer. Eur. Radiol. 2022, 32, 1676–1687.
- Yip, S.S.F.; Aerts, H.J.W.L. Applications and limitations of radiomics. Phys. Med. Biol. 2016, 61, R150–R166.
- Cain, E.H.; Saha, A.; Harowicz, M.R.; Marks, J.R.; Marcom, P.K.; Mazurowski, M.A. Multivariate machine learning models for prediction of pathologic response to neoadjuvant therapy in breast cancer using MRI features: A study using an independent validation set. Breast Cancer Res. Treat. 2019, 173, 455–463.
- Liu, Z.; Li, Z.; Qu, J.; Zhang, R.; Zhou, X.; Li, L.; Sun, K.; Tang, Z.; Jiang, H.; Li, H.; et al. Radiomics of multiparametric mri for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: A multicenter study. Clin. Cancer Res. 2019, 25, 3538–3547.
- Braman, N.M.; Etesami, M.; Prasanna, P.; Dubchuk, C.; Gilmore, H.; Tiwari, P.; Plecha, D.; Madabhushi, A. Intratumoral and peritumoral radiomics for the pretreatment prediction of pathological complete response to neoadjuvant chemotherapy based on breast DCE-MRI. Breast Cancer Res. 2017, 19, 1–14.
- Huang, Y.; Chen, W.; Zhang, X.; He, S.; Shao, N.; Shi, H.; Lin, Z.; Wu, X.; Li, T.; Lin, H.; et al. Prediction of Tumor Shrinkage Pattern to Neoadjuvant Chemotherapy Using a Multiparametric MRI-Based Machine Learning Model in Patients With Breast Cancer. Front. Bioeng. Biotechnol. 2021, 9, 662749.
- Lo Gullo, R.; Daimiel, I.; Morris, E.A.; Pinker, K. Combining molecular and imaging metrics in cancer: Radiogenomics. Insights Imaging 2020, 11, 1.
- Zhang, Y.; You, C.; Pei, Y.; Yang, F.; Li, D.; Jiang, Y.Z.; Shao, Z. Integration of radiogenomic features for early prediction of pathological complete response in patients with triple-negative breast cancer and identification of potential therapeutic targets. J. Transl. Med. 2022, 20, 256.
- Von Minckwitz, G.; Untch, M.; Blohmer, J.-U.; Costa, S.D.; Eidtmann, H.; Fasching, P.A.; Gerber, B.; Eiermann, W.; Hilfrich, J.; Huober, J.; et al. Definition and Impact of Pathologic Complete Response on Prognosis After Neoadjuvant Chemotherapy in Various Intrinsic Breast Cancer Subtypes. J. Clin. Oncol. 2012, 30, 1796–1804.
- Marinovich, M.L.; Houssami, N.; Macaskill, P.; Sardanelli, F.; Irwig, L.; Mamounas, E.P.; von Minckwitz, G.; Brennan, M.E.; Ciatto, S. Meta-analysis of magnetic resonance imaging in detecting residual breast cancer after neoadjuvant therapy. J. Natl. Cancer Inst. 2013, 105, 321–333.
- Khazindar, A.R.; Hashem, D.A.L.; Abusanad, A.; Abusanad, A.; Bakhsh, S.I.; Mahfouz, A.B.; El-Diasty, M.T. Diagnostic Accuracy of MRI in Evaluating Response After Neoadjuvant Systemic Therapy in Operable Breast Cancer. Cureus 2021, 13, e15516.
- Cortazar, P.; Zhang, L.; Untch, M.; Mehta, K.; Costantino, J.P.; Wolmark, N.; Bonnefoi, H.; Cameron, D.; Gianni, L.; Valagussa, P.; et al. Pathological complete response and long-term clinical benefit in breast cancer: The CTNeoBC pooled analysis. Lancet 2014, 384, 164–172.
- Kong, X.; Moran, M.S.; Zhang, N.; Haffty, B.; Yang, Q. Meta-analysis confirms achieving pathological complete response after neoadjuvant chemotherapy predicts favourable prognosis for breast cancer patients. Eur. J. Cancer 2011, 47, 2084–2090.
- Fowler, A.M.; Mankoff, D.A.; Joe, B.N. Imaging Neoadjuvant Therapy Response in Breast Cancer. Radiology 2017, 285, 358–375.
- Chen, J.-H.; Bahri, S.; Mehta, R.S.; Carpenter, P.M.; McLaren, C.E.; Chen, W.P.; Fwu, P.T.; Hsiang, D.J.; Lane, K.T.; Butler, J.A.; et al. Impact of factors affecting the residual tumor size diagnosed by MRI following neoadjuvant chemotherapy in comparison to pathology. J. Surg. Oncol. 2014, 109, 158–167.
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247.
- Lobbes, M.B.; Prevos, R.; Smidt, M.; Tjan-Heijnen, V.C.; van Goethem, M.; Schipper, R.; Beets-Tan, R.G.; Wildberger, J.E. The role of magnetic resonance imaging in assessing residual disease and pathologic complete response in breast cancer patients receiving neoadjuvant chemotherapy: A systematic review. Insights Imaging 2013, 4, 163–175.
- Berg, W.A.; Gutierrez, L.; NessAiver, M.S.; Carter, W.B.; Bhargava, M.; Lewis, R.S.; Ioffe, O.B. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology 2004, 233, 830–849.
- Scheel, J.R.; Kim, E.; Partridge, S.C.; Lehman, C.D.; Rosen, M.A.; Bernreuter, W.K.; Pisano, E.D.; Marques, H.S.; Morris, E.A.; Weatherall, P.T.; et al. MRI, clinical examination, and mammography for preoperative assessment of residual disease and pathologic complete response after neoadjuvant chemotherapy for breast cancer: ACRIN 6657 trial. Am. J. Roentgenol. 2018, 210, 1376–1385.
- Kim, T.H.; Kang, D.K.; Yim, H.; Jung, Y.S.; Kim, K.S.; Kang, S.Y. Magnetic Resonance Imaging Patterns of Tumor Regression After Neoadjuvant Chemotherapy in Breast Cancer Patients. J. Comput. Assist. Tomogr. 2012, 36, 200–206.
- Rosen, E.L.; Blackwell, K.L.; Baker, J.A.; Soo, M.S.; Bentley, R.C.; Yu, D.; Samulski, T.V.; Dewhirst, M.W. Accuracy of MRI in the Detection of Residual Breast Cancer After Neoadjuvant Chemotherapy. Am. J. Roentgenol. 2003, 181, 1275–1282.
- Bollet, M.A.; Thibault, F.; Bouillon, K.; Meunier, M.; Sigal-Zafrani, B.; Savignoni, A.; Diéras, V.; Nos, C.; Salmon, R.; Fourquet, A. Role of Dynamic Magnetic Resonance Imaging in the Evaluation of Tumor Response to Preoperative Concurrent Radio chemotherapy for Large Breast Cancers: A Prospective Phase II Study. Int. J. Radiat. Oncol. 2007, 69, 13–18.
- Reig, B.; Heacock, L.; Lewin, A.; Cho, N.; Moy, L. Role of MRI to Assess Response to Neoadjuvant Therapy for Breast Cancer. J. Magn. Reson. Imaging 2020, 52, 1587–1606.
- Belli, P.; Costantini, M.; Malaspina, C.; Magistrelli, A.; LaTorre, G.; Bonomo, L. MRI accuracy in residual disease evaluation in breast cancer patients treated with neoadjuvant chemotherapy. Clin. Radiol. 2006, 61, 946–953.
- Yeh, E.; Slanetz, P.; Kopans, D.B.; Rafferty, E.; Georgian-Smith, D.; Moy, L.; Halpern, E.; Moore, R.; Kuter, I.; Taghian, A. Prospective Comparison of Mammography, Sonography, and MRI in Patients Undergoing Neoadjuvant Chemotherapy for Palpable Breast Cancer. Am. J. Roentgenol. 2005, 184, 868–877.
- Kim, S.-Y.; Cho, N.; Shin, S.U.; Lee, H.B.; Han, W.; Park, I.A.; Kwon, B.R.; Kim, S.Y.; Lee, S.H.; Chang, J.M.; et al. Contrast-enhanced MRI after neoadjuvant chemotherapy of breast cancer: Lesion-to-background parenchymal signal enhancement ratio for discriminating pathological complete response from minimal residual tumour. Eur. Radiol. 2018, 28, 2986–2995.
- Bahri, S.; Chen, J.H.; Mehta, R.S.; Carpenter, P.M.; Nie, K.; Kwon, S.Y.; Yu, H.J.; Nalcioglu, O.; Su, M.Y. Residual breast cancer diagnosed by MRI in patients receiving neoadjuvant chemotherapy with and without bevacizumab. Ann. Surg. Oncol. 2009, 16, 1619–1628.
- Denis, F.; Desbiez-Bourcier, A.V.; Chapiron, C.; Arbion, F.; Body, G.; Brunereau, L. Contrast enhanced magnetic resonance imaging underestimates residual disease following neoadjuvant docetaxel based chemotherapy for breast cancer. Eur. J. Surg. Oncol. 2004, 30, 1069–1076.
- Bocci, G.; Di Paolo, A.; Danesi, R. The pharmacological bases of the antiangiogenic activity of paclitaxel. Angiogenesis 2013, 16, 481–492.
- Yu, H.J.; Chen, J.-H.; Mehta, R.S.; Nalcioglu, O.; Su, M.Y. MRI measurements of tumor size and pharmacokinetic parameters as early predictors of response in breast cancer patients undergoing neoadjuvant anthracycline chemotherapy. J. Magn. Reson. Imaging 2007, 26, 615–623.
- Woitek, R.; McLean, M.A.; Ursprung, S.; Rueda, O.M.; Manzano Garcia, R.; Locke, M.J.; Beer, L.; Baxter, G.; Rundo, L.; Provenzano, E.; et al. Hyperpolarized Carbon-13 MRI for Early Response Assessment of Neoadjuvant Chemotherapy in Breast Cancer Patients. Cancer Res. 2021, 81, 6004–6017.
- Woitek, R.; McLean, M.A.; Gill, A.B.; Grist, J.T.; Provenzano, E.; Patterson, A.J.; Ursprung, S.; Torheim, T.; Zaccagna, F.; Locke, M.; et al. Hyperpolarized 13C MRI of Tumor Metabolism Demonstrates Early Metabolic Response to Neoadjuvant Chemotherapy in Breast Cancer. Radiol. Imaging Cancer 2020, 2, e200017.
- Straver, M.E.; van Adrichem, J.C.; Rutgers, E.J.T.; Rodenhuis, S.; Linn, S.C.; Loo, C.E.; Gilhuijs, K.G.; Oldenburg, H.S.A.; Wesseling, J.; Russell, N.S.; et al. Neoadjuvant systemic therapy in patients with operable primary breast cancer: More benefits than breast-conserving therapy. Ned. Tijdschr. Geneeskd. 2008, 152, 2519–2525.
- Sardanelli, F.; Boetes, C.; Borisch, B.; Decker, T.; Federico, M.; Gilbert, F.J.; Helbich, T.; Heywang-Köbrunner, S.H.; Kaiser, W.A.; Kerin, M.J.; et al. Magnetic resonance imaging of the breast: Recommendations from the EUSOMA working group. Eur. J. Cancer 2010, 46, 1296–1316.
- Von Minckwitz, G.; Huang, C.S.; Mano, M.S.; Loibl, S.; Mamounas, E.P.; Untch, M.; Wolmark, N.; Rastogi, P.; Schneeweiss, A.; Redondo, A.; et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N. Engl. J. Med. 2019, 380, e617–e628.
- Borstkanker Onderzoek Groep. Image-guided de-escalation of neo-adjuvant chemotherapy in HER2-positive breast cancer: The TRAIN-3 study (TRAIN-3). ClinicalTrials.gov Identifier: NCT03820063. Available online: https://clinicaltrials.gov/ct2/show/NCT03820063 (accessed on 16 November 2022).
- Heil, J.; Kuerer, H.M.; Pfob, A.; Rauch, G.; Sinn, H.P.; Golatta, M.; Liefers, G.J.; Vrancken Peeters, M.J. Eliminating the breast cancer surgery paradigm after neoadjuvant systemic therapy: Current evidence and future challenges. Ann. Oncol. 2020, 31, 61–71.
- Kuerer, H.M.; Vrancken Peeters, M.; Rea, D.W.; Rea, D.W.; Basik, M.; De Los Santos, J.; Heil, J. Nonoperative management for invasive breast cancer after neoadjuvant systemic therapy: Conceptual basis and fundamental international feasibility clinical trials. Ann. Surg. Oncol. 2017, 24, e2855–e2862.
