Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Marina Mat Baki and Version 2 by Vivi Li.
Glottic insufficiency is widespread in the elderly population and occurs as a result of secondary damage or systemic disease. Tissue engineering is a viable treatment for glottic insufficiency since it aims to restore damaged nerve tissue and revitalize aging muscle. After injection into the biological system, injectable biomaterial delivers cost- and time-effectiveness while acting as a protective shield for cells and biomolecules.
- glottic insufficiency
- vocal fold injection
- incorporation
- cell-laden
- biomolecule
1. Introduction
Voice disorders affect 16.9% of the adult population (aged 18 and more) and 13.1% more of the elderly population (aged 85 and more) [1][2][3][1,2,3]. Glottic insufficiency is diagnosed when the vocal fold does not entirely close during phonation [4]. It impairs voice production and the protection of the lower airway, resulting in impaired social function, decreased work performance, and an increased risk of aspiration. Due to the unique characteristics of the human vocal fold and the numerous causes of glottic insufficiency, it is difficult to recommend the optimal treatment for this illness. Tissue engineering has advantages in this field since it strives to enhance regeneration and provides longer-lasting or even permanent vocal fold augmentation [5][6][5,6]. Tissue engineering has been researched extensively in several regenerative techniques, including cartilage, neuron, cardiac, and bone regeneration [7][8][9][10][7,8,9,10]. Nonetheless, previous studies [11][12][13][14][11,12,13,14] have identified vocal fold fibroblasts, muscle progenitor cells, embryonic stem cells (ESCs), bone marrow mesenchymal stem cells (BMMSCs), and adipose stem cells (ASCs) with or without the use of a scaffold as a delivery vehicle for vocal fold regeneration. This enstrudy seeks to outline the most recent advancements in injectable biomaterials that transport biomolecules and cells for regeneration purposes and to identify future directions for tissue engineering–based treatment of glottic insufficiency.
1.1. Structure of Vocal Fold
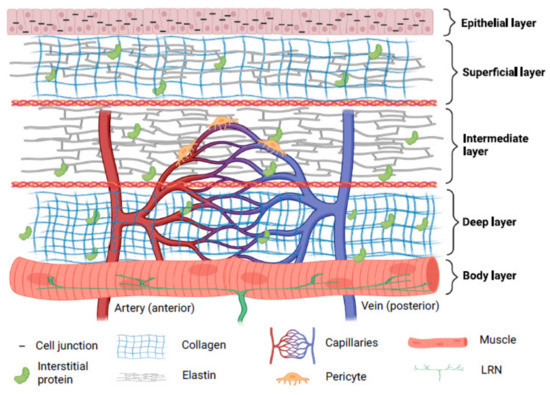
Three layers—cover, transition, and body—are thought to make up a human vocal fold [15]. Collagen, elastin, hyaluronic acid (HA), decorin, and fibronectin make up the majority of the extracellular matrix (ECM) proteins found in the lamina propria [16]. The superficial layers of lamina propria and epithelium in the cover have vibratory qualities which are crucial for phonation. Superficial lamina propria comprises loosely packed connective tissue [17]. The transition layer is made up of an intermediate layer primarily of elastin and deep layer of collagen. Collagen provides mechanical support to the vocal fold while elastin maintains the elasticity of the vocal fold [18][19][18,19]. The vocalis muscle makes up the body layer, which forms the base of this intricate three-dimensional structure [15]. Interestingly, cell junctions hold stratified squamous epithelium, which serves as a protective layer around membranous vocal folds [20]. Compared to newborn epithelial cells, adult epithelial cells displayed more significant intercellular gaps, greater mechanical strength, and more excellent elasticity [21]. In the lamina propria, the vascular network disperses differently. Only capillaries are seen in the superficial lamina propria; arterioles and venules are located in the intermediate and deep lamina propria. In muscular tissue, bigger vessels are more prevalent. Pericytes have been seen on capillaries, and it is thought that pericytes can shield capillaries from lamina propria vibration. Additionally, pericytes are found to be crucial for angiogenesis [22].
The paraglottic area, which houses intrinsic laryngeal muscle, nerve connections, and adipose tissue, is connected laterally to the vocal fold [23]. Intrinsic laryngeal muscles include thyroarytenoid (TA), lateral-cricoarytenoid (LCA) and interarytenoid (IA) muscles for adduction, and the posterior cricoarytenoid (PCA) muscle for abduction [24]. It is suggested that the TA, cricothyroid (CT), and LCA function as a single muscle stimulated by a motor unit [25]. Recurrent laryngeal nerves (RLN) and superior laryngeal nerves (SLN) provide intrinsic and extrinsic impulses, respectively [26]. RLN perform adduction and abduction functions [27]. The inability to change vocal pitch due to CT motor loss is directly related to SLN dysfunction [28]. The RLN innervates the thyroarytenoid-lateral cricoarytenoid (TA-LCA) for adduction, whereas the SLN innervates the CT. It can be summarized that the composition of the vocal fold includes elastic components which enable its phonation properties, mechanically strong components to support its structure, blood capillaries to provide nutrients to cells, and nerves to control its movement. The structure of the human vocal fold is briefly demonstrated in Figure 1.
1.2. Etiologies of Glottic Insufficiency
It is vital for the clinician to differentiate the causes of glottic insufficiency in opting for suitable treatments. The main symptoms of glottic insufficiency include being unable to generate an effective voice and being unable to protect the lower airway during swallowing. The most common cause of glottic insufficiency is vocal fold paralysis/paresis. Simply put, dysfunctional nerves or muscles are the primary causes of the vocal fold’s inadequate closure. Figure 2 explains the physiological characteristics of the normal condition and glottic insufficiency.
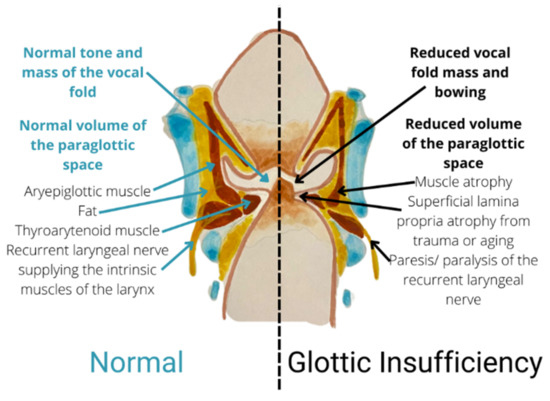
Figure 2.
Coronal section showing a comparison between normal condition and glottic insufficiency.
Vocal fold paralysis/paresis is identified when the RLN or SLN are damaged, causing the inability of the intrinsic laryngeal muscles to contract [24][29][30][24,29,30], contributing to the inability to move the vocal fold. Vocal fold paresis is defined when the nerve is partially damaged, causing incomplete signaling or abnormal signaling of nerve; paralysis is diagnosed when the vocal fold is not able to move completely [26]. Vocal fold paresis/paralysis has many etiologies, including scarring, iatrogenic disorders, malignancy, central nervous system pathology, and systemic illnesses [31]. An idiopathic cause is searched for when an aetiology cannot be determined after a comprehensive study.
Vocal fold atrophy is characterized when there is dissipation of muscle and loss of intonation even though the TA-LCA complex is mobile within a certain range [32]. Presbyphonia, child/adolescent, and inborn vocal fold scar are the three distinct types of vocal fold atrophy [33][34][35][36][33,34,35,36]. Commonly, the decreased sensitivity or malfunction of the contractile components inside the TA muscle is linked to the pathophysiology of vocal fold atrophy [1]. One of the possible causes of an ageing voice is structural changes in the vocal fold’s lamina propria [37]. The lamina propria became stiffer from increased collagen density and decreased elastin and HA density. Additionally, it was discovered that the activity of collagenase decreased in ageing vocal folds [16][38][16,38].
2. Tissue Engineering as a Promising Treatment for Glottic Insufficiency
2.1. Tissue Engineering in Vocal Fold Injection
Regenerative medicine is the approach of reinstating human cells, tissue or organs to their usual role [39][52]. Tissue engineering is application of biomaterial with or without cell transplantation to encourage endogenous regeneration and regain functional tissues or organs [40][53]. Fillers such as Teflon, polydimethysilicone and calcium hydroxyapatite are commonly injected into the vocal folds to improve glottal closure but are linked with the risk of inflammation, migration, and granuloma development [41][54]. Moreover, current clinical trial research for vocal fold injection focuses primarily on biomaterial alone (ClinicalTrials.gov number: NCT04700566, NCT03790956, NCT02163772) or direct injection of biomolecules or cells (ClinicalTrials.gov number: NCT05354544, NCT05385159, NCT03749863, NCT02622464, NCT02120781, NCT02904824, NCT04839276). It is suggested that combining biomaterials with biomolecules such as growth factors can improve the efficacy [42][55]. The combination of biomolecules, cells, and a scaffold serves as a unique delivery system. As cells proliferate to generate new tissue, biomolecules promote the growth of new tissue, and the scaffold serves as an environment for the regeneration of new tissue [43][44][56,57]. The comparison between injection of cells and biomolecules without and with a scaffold is shown in Figure 3.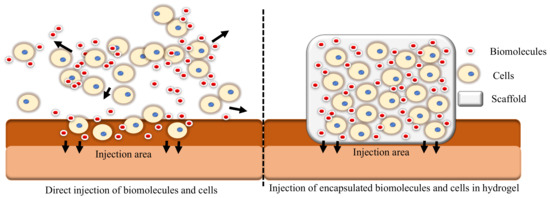
Figure 3.
A comparison between direct injection of cells and biomolecules versus injection of cells and biomolecules encapsulated in a hydrogel.
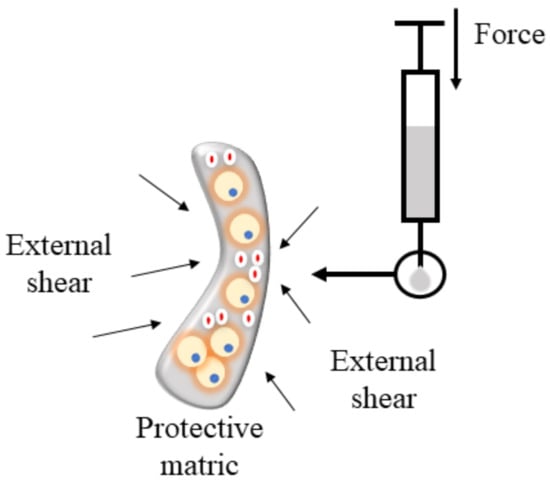
Figure 4.
Hydrogel protects cells during injection.
2.2. Injectable Hydrogel as Cell Delivery Vehicle
The majority of research develops encapsulation techniques for broad regeneration objectives. Muscle regeneration is followed by angiogenesis, nerve regeneration, and adipose tissue engineering in terms of the number of relevant studies. Comparatively, more research tried to encapsulate cells alone in biomaterials, followed by encapsulation of growth factor, MSC-extracellular vehicle (EV), and siRNA (siRNA). As illustrated in Supplementary Figure S3, three major categories of cells were examined. In clinical studies, direct injection of adipose-derived stem cells (ASCs) improved voice outcomes in patients with vocal fold scarring and glottic insufficiency [56][57][84,85]. Numerous in vivo investigations involving direct injection of ASCs have shown that ASCs can upregulate HA while downregulating collagen type I, type III, matrix metalloproteinase (Mmp1), and Mmp8 expression [58][59][60][86,87,88]. ASCs were also intimately linked to the secretion of FGF2, HGF, and basic fibroblast growth factor (bFGF). However, with direct injection, ASCs were only able to survive for 14 days; encapsulation helps to circumvent this problem [61][62][89,90]. It is uncertain whether ASCs or BMMSCs are more effective for augmenting vocal folds. Hiwatashi and colleagues recommended ASCs because they would increase HA control more effectively than BMMSCs [63][91]. Bartlett and colleagues recommended otherwise [64][92]. By stimulating BMMSCs with transforming growth factor beta (TGF-β), differentiation of vocal fold fibroblast into myofibroblast is inhibited [65][93]. Few investigations demonstrated that the qualities of ASCs are superior to those of BMMSCs because they are more stable, anti-inflammatory, proliferative, and have the same capacity to differentiate into various lineages [66][67][68][69][94,95,96,97]. The anti-fibrosis function of ASCs is depicted in Figure 5.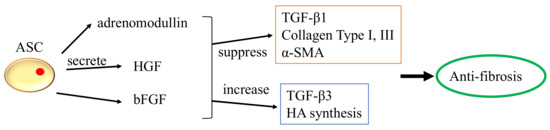
Figure 5.
The anti-fibrosis function of ASCs.
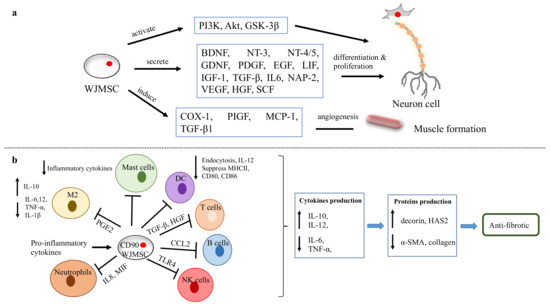
Figure 6.
WJMSC functions. (
a
) The function of WJMSCs in neuronal and muscular regeneration. (
b
) Immunomodulatory properties of WJMSCs in preventing fibrosis.
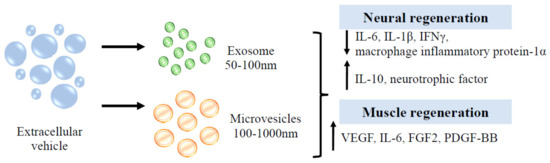
Figure 7.
Function of EVs in neuron and muscle regeneration.
2.3. Injectable Hydrogel as Biomolecule Delivery Vehicle
As hydrogel has a special affinity for water, it can be used as a hydrophilic growth factor delivery system. Based on the application (slow and extended or fast and short release), protein retention and delivery can be modified [79][117]. A hydrogel with low crosslinking, small particle size and susceptibility to enzymatic degradation will result in quicker growth factor release [80][118]. Growth factor incorporation will increase the bioactivity of the hydrogel [81][119]. For instance, Walters and colleagues demonstrated [82][120] that combining platelet-derived growth factor AB (PDGF-AB) and TGF-1 in collagen hydrogel promotes the differentiation of ASCs into smooth muscle cells. The thermosensitive heparin-poloxamer hydrogel containing bFGF and NGF enhances Schwann cell proliferation via the PI3K/Akt, JAK/STAT and MAPK/ERK signalling pathways [83][121]. To provide multiple regenerative aims, three different types of growth factors, namely VEGF, PDGF and BMP2, were released from a collagen hydrogel over a 28-day period in order to stimulate angiogenesis in a rat model [84][122]. TAs described in Supplementary Figure S4, the biomolecules employed in biomaterials can be categorised into four categories: neurotrophic growth factor, growth factor, proteins, and extracellular vesicles. In a rabbit model, a collagen scaffold containing NGF and human umbilical MSC was administered. After eight weeks, a positive response was obtained in the RLN injury model [72][100]. In vocal fold regeneration, brain-derived neurotrophic factor (BDNF), ciliary neurotrophic factor (CNF), and stromal cell-derived factor-1 (SDF-1) have not been researched. The SDF-1/CXCR4-mediated FAK/PI3K/Akt pathway [85][123] is thought to protect neuron tissue by avoiding cell death and inflammation. Following nerve damage, BDNF and SDF-1 increase in order to repair and modulate cells [86][124]. Ciliary neurotrophic factor enhances axon regeneration by binding to ciliary neurotrophic factor receptor α and then activating STAT3 [87][125]. Glottic insufficiency may have various causes, including muscle atrophy, nerve degeneration or damage, and anatomical alterations to the lamina propria. Consequently, treatment with just nerve growth factor may not yield optimal results. As the vocal fold is composed of epithelium and fibroblasts, EGF can reconstitute functional mucosa by promoting epithelium regeneration and HA synthesis. Several clinical trials [88][89][90][126,127,128] have demonstrated that direct injection of bFGF into the vocal fold has a beneficial effect on functional voice results. The most effective therapeutic impact on vocal fold atrophy was produced by this treatment. As the majority of instances were caused by ageing, bFGF use was shown to increase fibroblast synthesis of HA, hence lowering collagen deposition It was believed that bFGF treatment was more effective than biomaterial implantation because it altered the vibratory characteristics of the vocal fold and increased its volume [91][129]. bFGF was not only able to restore the flexibility of the vocal fold but also increased the density of the thyroarytenoid muscle in aged vocal folds [92][130]. Hepatocyte growth factor (HGF) has anti-fibrotic and angiogenesis properties and is produced by mesenchymal cells such as fibroblasts, macrophages, renal mesangium, etc. A clinical investigation demonstrated the efficacy and regeneration potential of HGF in patients with vocal fold scarring and sulcus. By repeatedly injecting the vocal fold with HGF, the patients exhibited a considerably improved outcome while maintaining a high level of safety. An earlier pre-clinical investigation demonstrated that HGF could boost fibroblast synthesis of HA and decrease collagen deposition [93][131]. In a second in-vitro study of a damaged vocal fold in rabbits, HGF delivered in a hyaluronic/alginate hydrogel was more effective than HGF injection alone [94][132]. With immediate treatment of HGF after vocal fold injury, collagen synthesis was decreased and angiogenesis was stimulated [95][133]. There is paucity of data on the effect of PDGF-BB on vocal fold regeneration. One study, however, showed that PDGF-BB can stimulate vessel development in rat models [96][134]. Similar to PDGF-BB, angiogenin has not been researched in the regeneration of vocal folds. By blocking the TGF-1/Smad pathway, it has been shown to alter fibroblast scar formation [97][135]. VEGF stimulates the development of blood vessels, which is essential for tissue regeneration. Then, numerous investigations on VEGF in various areas, including skeletal, peripheral nerve, dental pulp, and heart regeneration, were conducted [98][99][100][101][102][136,137,138,139,140]. VEGF promotes the development of HUVEC and neurite cells through the Erk/Akt pathway [103][141]. IGF-1 is one of the key proteins that regulate skeletal muscle metabolism pathways such as PI3K/Akt/mTOR and PI3K/Akt/GSK3β. IGF-1 suppresses cytokines that produce muscle atrophy and myostatin via these signalling pathways by suppressing nuclear factor-kappa beta (NF-ĸB) and Smad pathways. It can also promote skeletal muscle stem cells for the regeneration of skeletal muscle [104][142]. Insulin growth factor-1 (IGF-1) was induced by myokine/cytokine Meteorin-like that promotes myogenesis [105][143]. Researchers are currently interested in the exosome from umbilical cord MSC, since it can prevent tumorigenic concerns. It has great promise for use in a variety of conditions, including wounds, type 2 diabetes, inflammatory bowel disease, Alzheimer’s disease, spinal cord injury, myocardial ischemia injury, and graft-versus-host disease [106][144]. Extracellular vesicles (EVs) can be subdivided into numerous categories. Microvesicles and exosomes are among the subgroups. Microvesicles transport phosphatidylserine-containing proteins, mRNAs, miRNAs, and lipids, while exosomes transport DNA, lipids, RNAs, and proteins [107][145]. Human umbilical cord EVs have been demonstrated to exert anti-inflammatory qualities (interleukin-10, IL-10) and reduced pro-inflammatory responses (IL-1β, IL-6), followed by improved motor, axon, and Schwann cell regeneration [108][146]. Myoblasts release EVs containing HGF, IGF-1, TGF-3, VEGF, fibroblast growth factor-β3 (TGF-β3) and fibroblast growth factor 2 (FGF2). These secretions promote cell interaction between myoblasts for proliferation [109][147]. EVs enhance cross-talk in skeletal muscle to induce glucose release and adipose dissociation [110][148]. Interestingly, EVs that are secreted by astrocyte support a variety of tasks that range from delivering angiogenic factors such as FGF2, and VEGF to heat shock proteins, synapsin 1 and apolipoprotein-D, which aid in neuronal protection in hazardous settings [111][149]. EVs play a role in neuronal cell communication and in response to external stimuli such as inflammatory responses and the central nervous system [112][150]. Although EV can be created from a variety of cell sources, EV derived from MSC is persuasive in its ability to regenerate the central nervous system [113][151]. Figure 8 summarises the regenerative properties of EVs in neuronal and muscular tissue.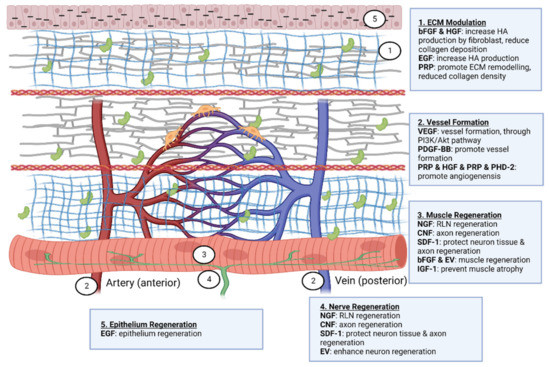
Figure 8.
Therapeutic effect of biomolecules on vocal fold regeneration. Created with Biorender.com (accessed on 24 October 2022).