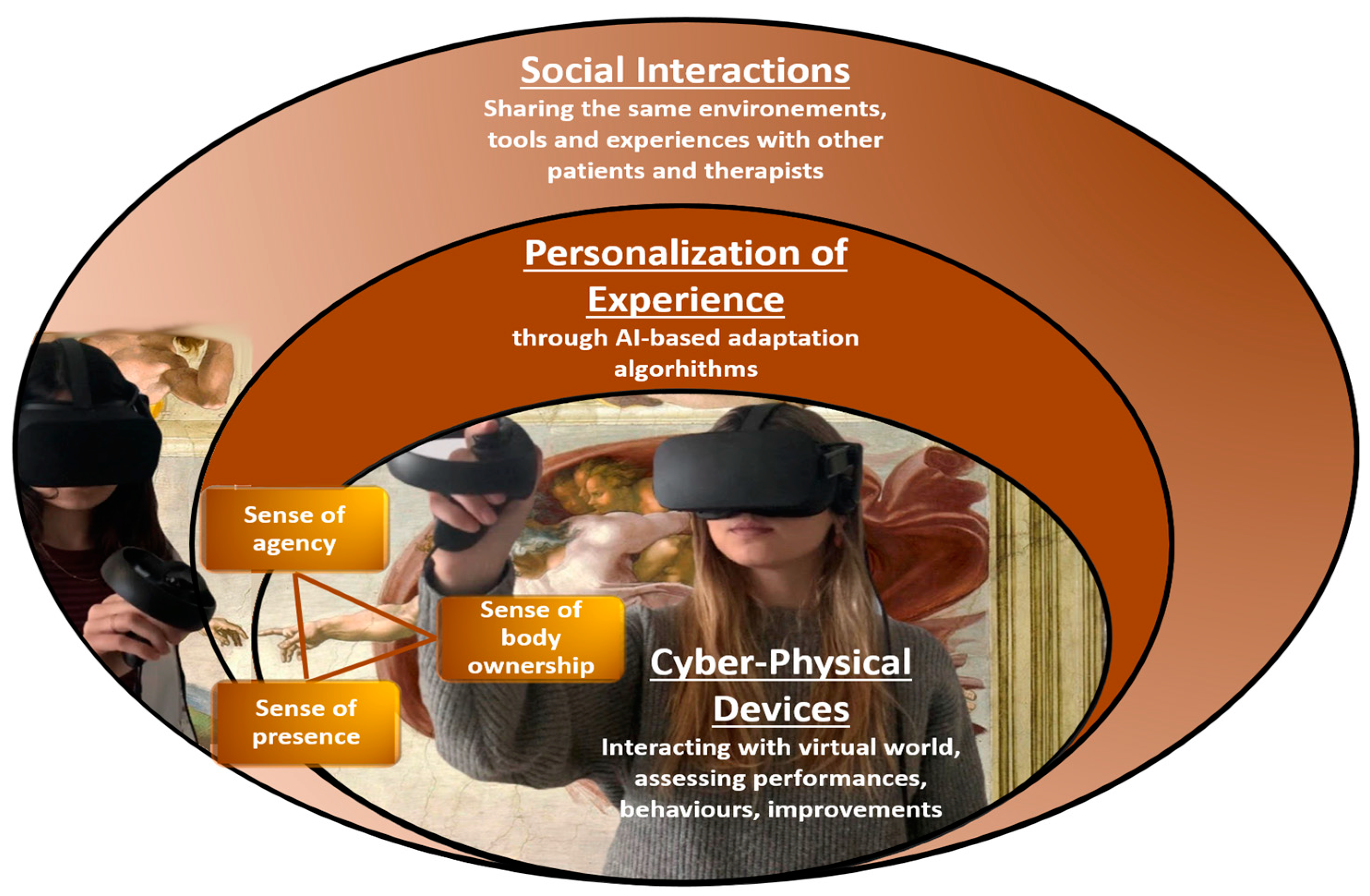
The metaverse is a new technology thought to provide a deeper, persistent, immersive 3D experience combining multiple different virtual approaches in a full continuum of physical–digital interaction spaces. Different from virtual reality (VR) and augmented reality (AR), the metaverse has a service-oriented solid model with an emphasis on social and content dimensions. The fundamental innovations that could be brought about by the metaverse rely on the evolution of immersive experience and on the employment of multiple technologies—artificial intelligence, internet of things, blockchain, etc.—to facilitate the virtuality–reality interconnection by mimicking brain functioning. In particular, AI tools (i.e., deep learning) will bring insights into new treatment approaches, leading to a profound impact on personalized medicine for mental health conditions. The complexity of the metaverse is discussed, which could be considered the future of neurorehabilitation.
- metaverse
- neurorehabilitation
- VR
1. The Basis for Applying Metaverse-Related Technology in Neurological Rehabilitation
1.1. Movement Disorders
1.2. Cognitive Disorders
1.3. Other Neurological Diseases
1.4. Psychosocial Rehabilitation
2. The Metaverse Could Enhance the Translation to the Holistic Neurorehabilitation Approach
References
- Matamala-Gomez, M.; Maselli, A.; Malighetti, C.; Realdon, O.; Mantovani, F.; Riva, G. Virtual Body Ownership Illusions for Mental Health: A Narrative Review. J. Clin. Med. 2021, 10, 139.
- Winter, D.; Malighetti, C.; Cipolletta, S.; Ahmed, S.; Benson, B.; Röhricht, F. Construing and body dissatisfaction in chronic depression: A study of body psychotherapy. Psychiatry Res. 2018, 270, 845–851.
- Maggio, M.G.; Piazzitta, D.; Andaloro, A.; Latella, D.; Sciarrone, F.; Casella, C.; Naro, A.; Manuli, A.; Calabrò, R.S. Embodied cognition in neurodegenerative disorders: What do we know so far? A narrative review focusing on the mirror neuron system and clinical applications. J. Clin. Neurosci. 2022, 98, 66–72.
- Huang, J.; Lin, M.; Fu, J.; Sun, Y.; Fang, Q. An Immersive Motor Imagery Training System for Post-Stroke Rehabilitation Combining VR and EMG-based Real-Time Feedback. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2021, 2021, 7590–7593.
- Yoshimura, M.; Kurumadani, H.; Hirata, J.; Osaka, H.; Senoo, K.; Date, S.; Ueda, A.; Ishii, Y.; Kinoshita, S.; Hanayama, K.; et al. Virtual reality-based action observation facilitates the acquisition of body-powered prosthetic control skills. J. Neuroeng. Rehabil. 2020, 17, 113.
- Köyağasıoğlu, O.; Özgürbüz, C.; Bediz, C.Ş.; Güdücü, Ç.; Aydınoğlu, R.; Akşit, T. The Effects of Virtual Reality Nonphysical Mental Training on Balance Skills and Functional Near-Infrared Spectroscopy Activity in Healthy Adults. J. Sport Rehabil. 2022, 31, 428–441.
- Morone, G.; Ghanbari Ghooshchy, S.; Palomba, A.; Baricich, A.; Santamato, A.; Ciritella, C.; Ciancarelli, I.; Molteni, F.; Gimigliano, F.; Iolasconc, G.; et al. Differentiation among bio- and augmented- feedback in technologically assisted rehabilitation. Expert Rev. Med. Devices 2021, 18, 513–522.
- Johnson, L.; Burridge, J.H.; Demain, S.H. Internal and external focus of attention during gait re-education: An observational study of physical therapist practice in stroke rehabilitation. Phys. Ther. 2013, 93, 957–966.
- Daniel, R.; Radulescu, A.; Niv, Y. Intact Reinforcement Learning But Impaired Attentional Control During Multidimensional Probabilistic Learning in Older Adults. J. Neurosci. 2020, 40, 1084–1096.
- Kirsch-Darrow, L.; Tsao, J.W. Cognitive Rehabilitation. Behav. Neurol. Psychiatry 2021, 27, 1670–1681.
- Maier, M.; Ballester, B.R.; Verschure, P.F.M.J. Principles of Neurorehabilitation After Stroke Based on Motor Learning and Brain Plasticity Mechanisms. Front. Syst. Neurosci. 2019, 13, 74.
- Gao, Y.; Ma, L.; Lin, C.; Zhu, S.; Yao, L.; Fan, H.; Gong, J.; Yan, X.; Wang, T. Effects of Virtual Reality-Based Intervention on Cognition, Motor Function, Mood, and Activities of Daily Living in Patients With Chronic Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Aging Neurosci. 2021, 13, 766525.
- Chen, X.; Liu, F.; Lin, S.; Yu, L.; Lin, R. Effects of Virtual Reality Rehabilitation Training on Cognitive Function and Activities of Daily Living of Patients With Poststroke Cognitive Impairment: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2022, 103, 1422–1435.
- Moeinzadeh, A.M.; Calder, A.; Petersen, C.; Hoermann, S.; Daneshfar, A. Comparing virtual reality exergaming with conventional exercise in rehabilitation of people with multiple sclerosis: A systematic review. Neuropsychol. Rehabil. 2022; online ahead of print.
- Zhu, S.; Sui, Y.; Shen, Y.; Zhu, Y.; Ali, N.; Guo, C.; Wang, T. Effects of Virtual Reality Intervention on Cognition and Motor Function in Older Adults With Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Front. Aging Neurosci. 2021, 13, 586999.
- Lu, Y.; Ge, Y.; Chen, W.; Xing, W.; Wei, L.; Zhang, C.; Yang, Y. The effectiveness of virtual reality for rehabilitation of Parkinson disease: An overview of systematic reviews with meta-analyses. Syst. Rev. 2022, 11, 50.
- Ogourtsova, T.; Souza Silva, W.; Archambault, P.S.; Lamontagne, A. Virtual reality treatment and assessments for post-stroke unilateral spatial neglect: A systematic literature review. Neuropsychol. Rehabil. 2017, 27, 409–454.
- Cavedoni, S.; Cipresso, P.; Mancuso, V.; Bruni, F.; Pedroli, E. Virtual reality for the assessment and rehabilitation of neglect: Where are we now? A 6-year review update. Virtual Real. 2022; online ahead of print.
- Gorelik, V.; Filippova, S.N.; Belyaev, V.S.; Karlova, E.V. Efficiency of image visualization simulator technology for physical rehabilitation of children with cerebral palsy through play. Bull RSMU 2019, 4, 39–46.
- Choi, J.Y.; Yi, S.; Ao, L.; Tang, X.; Xu, X.; Shim, D.; Yoo, B.; Park, E.S.; Rha, D. Virtual reality rehabilitation in children with brain injury: A randomized controlled trial. Dev. Med. Child Neurol. 2020, 63, 480–487.
- Iosa, M.; Verrelli, C.M.; Gentile, A.E.; Ruggieri, M.; Polizzi, A. Gaming Technology for Pediatric Neurorehabilitation: A Systematic Review. Front. Pediatr. 2022, 10, 775356.
- Alrashidi, M.; Wadey, C.A.; Tomlinson, R.J.; Buckingham, G.; Williams, C.A. The efficacy of virtual reality interventions compared with conventional physiotherapy in improving the upper limb motor function of children with cerebral palsy: A systematic review of randomized controlled trials. Disabil. Rehabil. 2022; online ahead of print.
- Gerber, C.N.; Kunz, B.; van Hedel, H.J. Preparing a neuropediatric upper limb exergame rehabilitation system for home-use: A feasibility study. J. Neuroeng. Rehabil. 2016, 13, 33.
- Bernhardt, J.; Dewey, H.; Thrift, A.; Donnan, G. Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke 2004, 35, 1005–1009.
- Janssen, H.; Ada, L.; Bernhardt, J.; McElduff, P.; Pollack, M.; Nilsson, M.; Spratt, N.J. An enriched environment increases activity in stroke patients undergoing rehabilitation in a mixed rehabilitation unit: A pilot non-randomized controlled trial. Disabil. Rehabil. 2014, 36, 255–262.
- Beauchet, O.; Matskiv, J.; Galery, K.; Goossens, L.; Lafontaine, C.; Sawchuk, K. Benefits of a 3-month cycle of weekly virtual museum tours in community dwelling older adults: Results of a randomized controlled trial. Front. Med. 2022, 9, 969122.
- Dinh, A.; Furukawa, L.; Caruso, T.J. The virtual visit: Using immersive technology to visit hospitals during social distancing and beyond. Paediatr. Anaesth. 2020, 30, 954–956.
- Kye, B.; Han, N.; Kim, E.; Park, Y.; Jo, S. Educational applications of metaverse: Possibilities and limitations. J. Educ. Eval. Health Prof. 2021, 18, 32.
- Mäntynen, A.; Rosti-Otajärvi, E.; Hämäläinen, P. Neuropsychological rehabilitation should not aim only at better cognitive task scores: A reply to the letter of Cerasa, Tomaiuolo and Quattrone. Mult. Scler. 2014, 20, 126–127.
- Feys, P.; Giovannoni, G.; Dijsselbloem, N.; Centonze, D.; Eelen, P.; Lykke Andersen, S. The importance of a multi-disciplinary perspective and patient activation programmes in MS management. Mult. Scler. 2016, 22 (Suppl. 2), 34–46.
- Kesselring, J. Neurorehabilitation in Multiple Sclerosis—Resilience in Practice. Eur. Neurol. Rev. 2017, 12, 31–36.
- World Health Organization. How to Use ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF); Exposure Draft for Comments; WHO: Geneva, Switzerland, 2013.
- Polnay, A.; James, V.A.; Hodges, L.; Murray, G.D.; Munro, C.; Lawrie, S.M. Group therapy for people with bulimia nervosa: Systematic review and meta-analysis. Psychol. Med. 2014, 44, 2241–2254.
