You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 3 by Vivi Li and Version 2 by Vivi Li.
The ultimate goal of nanomedicine has always been the generation of translational technologies that can ameliorate current therapies. Cancer disease represented the primary target of nanotechnology applied to medicine, since its clinical management is characterized by very toxic therapeutics. In this effort, nanomedicine showed the potential to improve the targeting of different drugs by improving their pharmacokinetics properties and to provide the means to generate new concepts of treatments based on physical treatments and biologics.
- nanomedicine
- targeted therapies
- EPR
- SPION
- Abraxane
- Doxil
- micelles
- exosomes
1. Introduction
Nanotechnology development for the medical field has always been focused primarily on translational purposes [1]. Nanomedicine was conceived to increase the safety of very toxic drugs, providing the therapeutics a means for targeting the sick tissues [2]. For this reason, nanotherapeutics were tested extensively to improve chemotherapy performances. Most of the investigations, in fact, were dedicated to enhance the antitumor power of drugs that were already approved in clinics, but characterized by severe adverse effects limiting their use [3]. Liposomal formulation of Doxorubicin (DOX) [4] and Daunorubicin [5] were the first FDA approved nanotherapies in 1995 and 1996, respectively. First generation of nanoparticles targeted the cancer lesions by exploiting leaky tumor vasculature and the lack of an efficient tumor lymphatic system, a phenomenon known as enhanced permeability and retention effect (EPR) [6]. In this case, the nanoparticles were designed with high circulation properties to facilitate their accumulation in the tumor tissue, where they could release their therapeutic payload. Here, surface modifications like polyethylene glycol (PEG) could minimize particle sequestration in the elements of the mononuclear phagocytic system (MPS), inhibiting particle opsonization and internalization [7]. Second generation of nanomedicine provided the carriers with more complex surface modifications [8] or particular shapes [9] that alone or in combination with “stealthing” molecules allowed for active targeting. Most of these modifications were based on peptides, antibodies or ligand moieties that could be recognized by surface receptors over-expressed on cancer cells [10]. This strategy allowed for a more stable interaction of the NPs with cancer cells and favored their internalization [10]. In these technologies, cancer lesion targeting still occurs via EPR, even though some surface modification can impart the carriers with trafficking properties that can enhance their active accumulation in the sick tissue. A recent review by Anselmo et al. [11], showed that in the last 3 decades, a little more 30 than nanoformulations were approved and less than half of them were designed for cancer treatment. The translation of nanomedicine to the clinic has been hindered by the formidable ability of our body to recognize foreign bodies [12], tumor organization [13], and concerns derived from systemic toxicity and immune system activation [3]. Further efforts in facing this issue generated more and more complex surface modifications, as well as carriers derived from natural sources like exosomes [14]. Unfortunately, while in preclinical settings these technologies provided promising results, their clinical translation was hampered by their high costs of production and sometimes by issues of generating nanoformulations in large scale [15][16]. However, the research in the field is still very active and supported by the exploration of alternative administration routes other than intravenous [17][18] and by the development of other applications, including diagnosis.
2. Inorganic NPs
2.1. AGuIX
A promising approach to overcome current therapies limitations is the use of new therapeutic agents (molecules or nanoparticles) that sensitize cancer cells to radiotherapy (RT) also known as dose enhancers and radiosensitizers. This enhanced radiation local absorption in combination with the accumulation of high Z-elements in the irradiated cancer tissue results in a larger production of harmful diffused photons, photoelectrons, Auger electrons, Compton electrons, and radical species [19]. AGuIX particles were firstly synthesized in 2011 [20] to increase the radiobiological effect of high-energy radiation in the tumor. This technology is composed of very small (average size 5 nm diameter) polysyloxane particles with chelated cyclic gadolinium covalently grafted into the inorganic matrix [21] (Figure 1). In preclinical experiments, AGuIX NPs showed high radiosensitizing and anti-tumor properties [22] that combined with a solid and reproducible synthesis process favored their evaluation in clinical settings.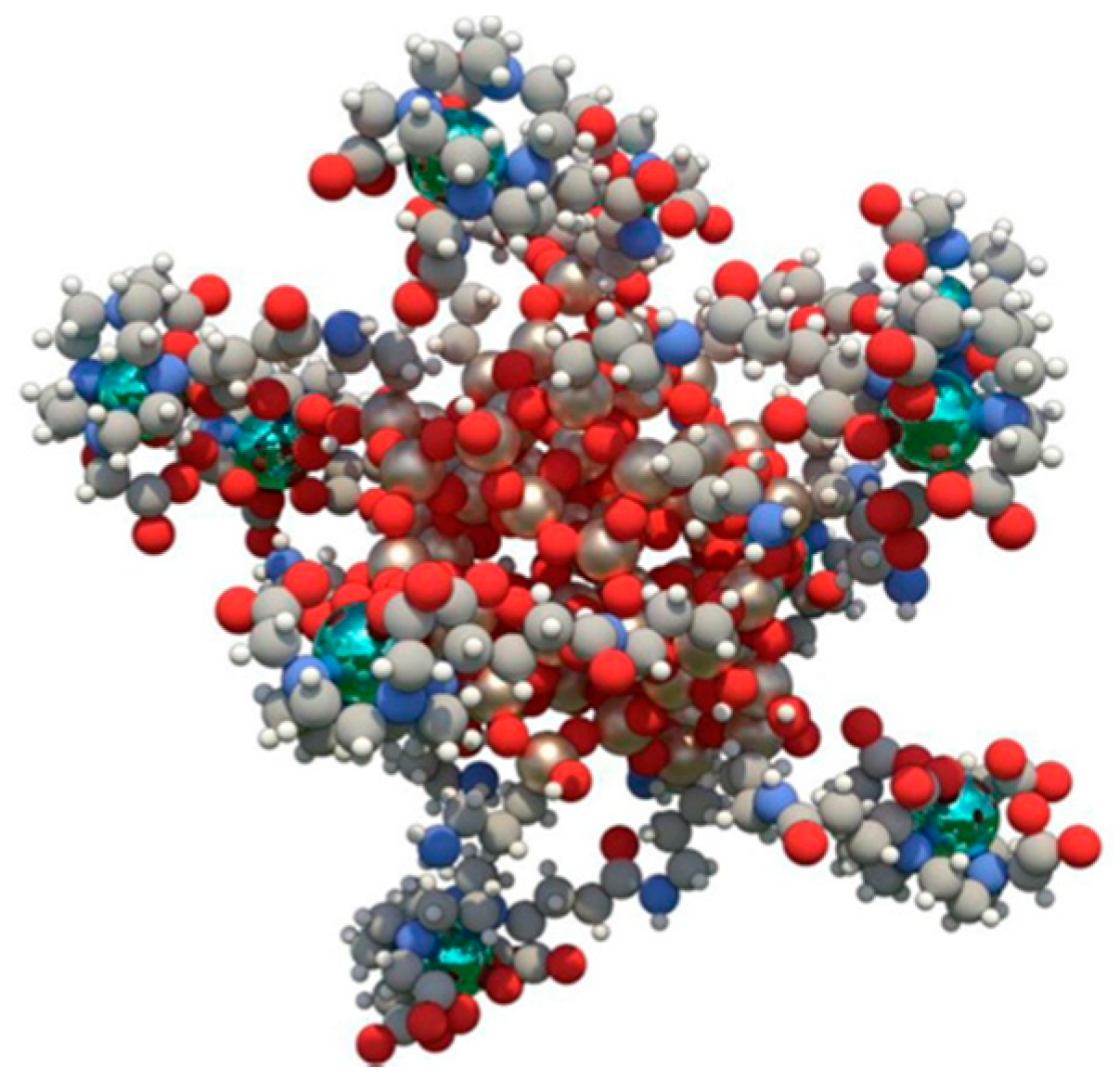
Figure 1. AGuIX structure: Polysiloxane structure of AGuIX chelating gadolinium (green) via dodecane tetraacetic acid ligands. Figure reprinted from Lux et al. [21].
2.2. NBTXR3
NBTXR3 technology is a novel radio sensitizer comprising crystalized hafnium oxide (HfO2) nanoparticles, locally injected into tumor tissue and activated by RT. HfO2 nanoparticles possess excellent x-ray absorption coefficient because of the high electron-density elements composing the particles and acceptable safety. The particles are 50 nm in size and negatively charged thanks to a phosphate coating applied to maintain colloidal stability [36]. NBTXR3 followed by RT could improve the treatment of advanced or borderline-resectable cancers compared to RT alone [36]. Preclinical studies have shown that NBTXR3 working mechanism is mostly physical without targeting specific biological pathways, and its use could be extended to many types of cancer. The system was tested in patients with head and neck squamous cell carcinoma exploring a dose escalation setting [37]. Within 7 weeks after NBTXR3 injection, nanoparticles in the surrounding tissues disappeared, showing that the system was well tolerated. Additionally, this entry [37] showed that one intratumor administration of NBTXR3 before radiotherapy could yield remarkable local tolerance, homogeneous dispersion of the particles in the tumor tissue, no leakage, and showed promising signs of anticancer activity in terms of pathological responses. In another study [38] dose optimization and side effects were evaluated for NBTXR3 in association with RT for recurrent and inoperable non-small cell lung cancer patients. The purpose of NCT04484909 [39] and NCT04615013 [40] trials (phase I) was to determine the recommended phase 2 dose and safety profile of NBTXR3 activated by radiation therapy to treat metastatic, borderline-resectable pancreatic cancers and esophageal adenocarcinoma, respectively. NBTXR3 nanoparticles have become the subject of many clinical trials to treat solid tumor with metastases to lung and/or liver [41], head and neck cancer [42][43] and soft tissue sarcoma [44]. Here, the patients underwent radiotherapy with or without a previous local injection of the radiosensitizer. The presence NBTXR3 doubled the pathological complete response of the patients with no occurrence of important adverse effect [45]. Promising results were collected also in a Phase 1 trial investigating the safety and efficacy of this technology in elderly patient affected by oropharynx and oral cavity cancer [46].2.3. Super Magnetic Iron Oxide
Superparamagnetic iron oxide nanoparticles (SPION) found their application in the biomedical field because of their theranostic properties, since they can allow for MRI and thermo-ablation. SPION working mechanism depends on an external alternate magnetic field determining their action only in the sick tissue. The synthesis of these particles is based on the nanomanipulation of magnetite and maghemite [47] and their dispersion is obtained through surface modifications (capping) based on organic molecules [48] and polymeric (i.e., polyethylene glycol) [49] surface functionalization. Their size ranges from 20 to 150 nm [47] and the mechanism of tumor accumulation is based on intratumoral injection [50] or EPR [51] following IV administration. However, in preclinical studies they were object of intense studies to engineering their surface with targeting molecules [52] to increase their residence time and internalization in cancer cells. These manipulations focused also on conjugating therapeutic agents on their surface comprising both small molecules [53] and biologics [50]. Attempts at exploiting polarized magnetic fields to increase their tumor targeting were proposed as well [54]. Finally, they were often used to implement the properties of other delivery platforms in hybrid synthetic settings [55]. Their translational use was deeply investigated mostly for their ability to enhance the MRI resolution, even though their toxicity related to DNA damage and reactive oxygen species formation limited their large application [56]. FDA-approved formulations of SPION are currently intended as iron replacement and they are secondarily used as contrast agents for kidney imaging [57][58]. In this scenario, the only phase 3 and 4 trial focused on this technology aimed at understanding the SPION ability to detect lymphatic metastases in breast [59] and pancreatic cancer [60] after IV infusion. The latter trial showed, in comparison with traditional histology, a matching of the 2 methods higher than the 80%. Ongoing clinical trials aim to investigate the efficacy of locally injected SPION magnetic hyperthermia against brain and prostate tumors. In a phase I clinical trial, the authors showed the effect of thermoablation to treat prostate cancer by local injection of SPION and further thermoablation induction under magnetic field application [61]. Untargeted SPION (Ferumoxytol) are currently evaluated for treatment of primary and metastatic hepatic cancers [62]. The radiotherapy with SPION supported by magnetic resonance imaging guided linear accelerator allowed to detect and maximize avoidance of residual functionally active hepatic parenchyma from over-the-threshold irradiation thus minimizing SBRT liver damages because of stereotactic body radiation therapy in patients with pre-existing hepatic conditions. The safety, efficacy and tolerability of SPION in combination with spinning magnetic field (SMF) and neoadjuvant chemotherapy in osteosarcoma patients is currently evaluated in a Phase I clinical trial [63]. The study comprises intra-tumor injection of SPIONs followed by SMF and conventional neoadjuvant chemotherapy from day 1. The authors declare a synergistic effect of SPIONs/SMF with neoadjuvant chemotherapy in increasing cancer cell killing and improving the ratio of limb retention (amputation).2.4. Gold Nanoparticles
Besides their use for increasing the sensitivity of current diagnostic and prognostic tests [64], NU-0129 gold nanoparticles were tested in a Phase 0 clinical trial against gliosarcoma and glioblastoma [65][66]. The particles were modified covalently with a spherical RNAi corona targeting BCL2L12 messenger. The author could detect the accumulation of the particles in the tumor and a decrease in the BCL2L12 expression. However, the authors of this work could not find more information of this technology in terms of size and surface charge, speculating that the ability of this technology to overcome the blood–brain barrier is probably due to their small size, as demonstrated in other pre-clinical studies [67]. On the other hand, the overcoming of the blood–brain barrier could be favored by the nucleic acid coating of the particles since spherical RNAi could be trafficked via transcytosis, with the gold core fundamental to avoid the fast clearance of the system [66].2.5. ELU001 (Folic-Acid Functionalized C’Dot-Drug-Conjugate)
The folate receptor alpha (FRα) represents a promising target in oncology because of its over-expression in tumors (i.e., ovarian, breast and lung cancers), low and restricted distribution in normal tissues [68], emerging insights about its tumor promoting functions, and association with patient prognosis. ELU001 is a new molecular C’Dot Drug Conjugate (CDC). ELU001 comprises a very small silica core (6 nm) functionalized with ~12 folic acid targeting moieties and ~22 exatecan topoisomerase-1 inhibitor payloads linked to via Cathepsin-B cleavable linkers covalently bound to the surface of the nanoparticles. Because of their small size, ELU001 are characterized by tumor penetration ability via receptor-mediated endocytosis and are rapidly eliminated by the kidneys. ELU001 high avidity is believed to promote internalization into FRα over-expressing cancer cells, selectively delivering its therapeutic payload. The first Phase I/II clinical trial [69] dedicated to ELU-FRα-1 is under recruiting phase for advanced, recurrent or refractory FRα over-expressing tumors, considered being topoisomerase 1 inhibitor-sensitive [70] and with no other therapeutic options available. The study will focus on dose escalation and safety to determine the recommended Phase 2 dose and on the expansion of the patient cohort, where specific cancer types will be evaluated for efficacy and safety of this technology.3. Polymeric Particles
3.1. CALAA-01
CALAA-01 is considered the first targeted polymeric carrier designed for delivering siRNA tested in human [71]. A positively charged cyclodextrin core allows the loading the negative nucleic acid payload. Polydispersity, stability, circulation, and targeting properties depend on surface PEGylation and transferrin modification (Figure 2) [72].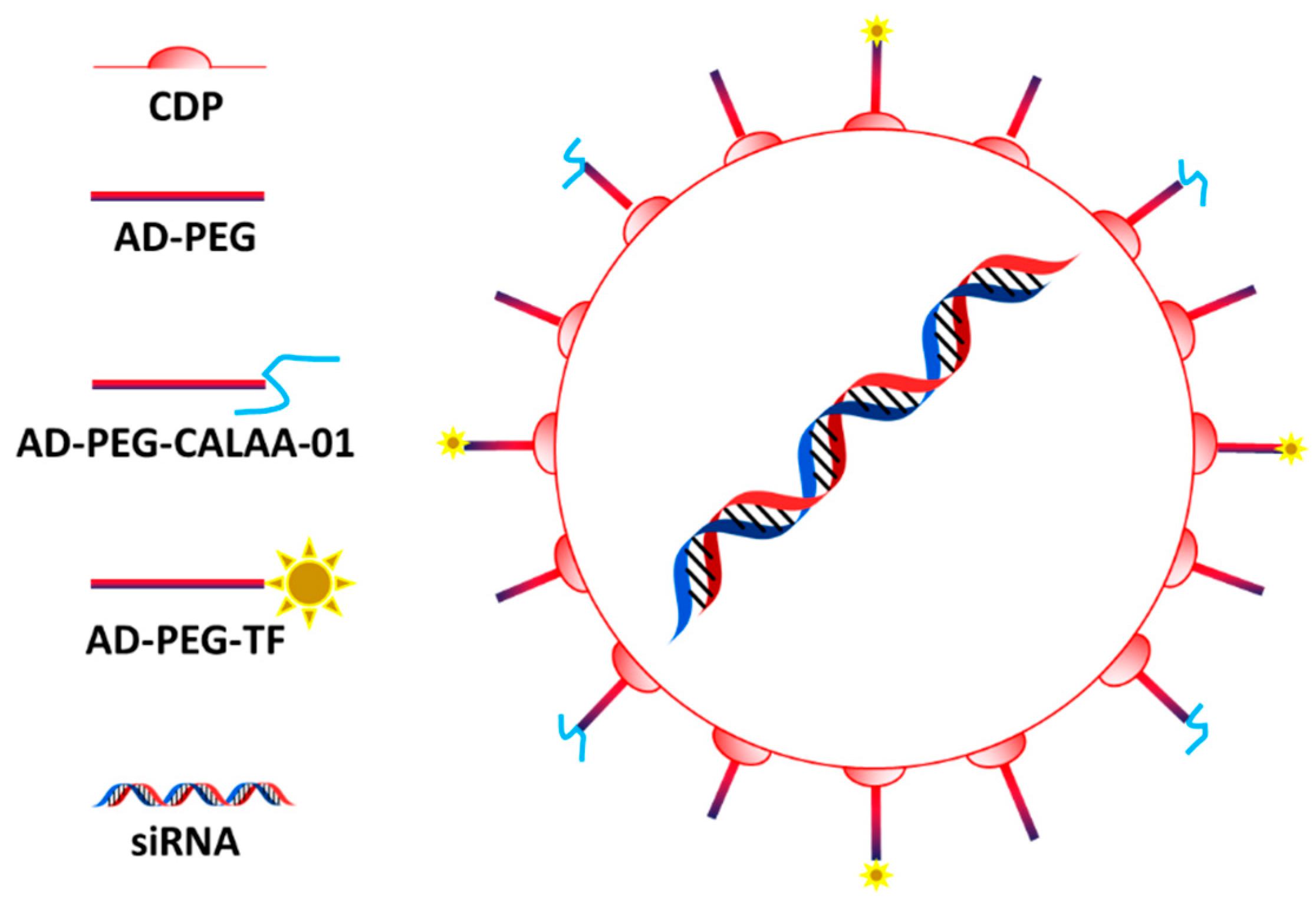
Figure 2. CALAA-01 structure: The system is composed by a core of cyclodestrin encapsulating the siRNA and functionalized with PEG bearing adamantine (AD-PEG) and transferrin (AD-PEG-TF). Figure from Kurreck et al. [72].
3.2. Micelles
Polymeric micelles are nanocarriers composed of a core–shell structure that can be generated via self-assembly of amphiphilic block copolymers [77]. Because of their self-assembly and amphiphilic nature, micelles are relatively easy to synthesize compared to other technologies and for this reason they are often studied as drug delivery vehicles for poor water-soluble compounds [78]. Hydrophilic polymers including (but not limited to) PEG, polyoxazolines, chitosan, dextran, and hyaluronic acids can wrap their hydrophobic core, while the therapeutic payloads can be also chemically conjugated to these structures [79]. Micelle surface can be easily modified in function of the number of monomers used in their fabrication and conjugation of tumor-specific ligands is easy and reproducible [79][80]. Regarding their clinical translation, one of the major limitations of micelles is represented by their low mechanical properties and re-assembly when their amount in aqueous solution is below the so-called critical micellar concentration [77]. Currently, there are several micellar-based nanoformulations approved for improving cancer treatment, and others are in advanced clinical trials. The chemotherapeutic drug Paclitaxel (PTX) that has a very low solubility in water (less than 0.1 µg/mL) is often used in micellar-based systems to avoid Cremophor-EL and ethanol formulations, resulting in adverse reactions like dyspnea, hypotension, angioedema, and generalized hives (2–4% of patients). Genexol-PM, a monomethoxy-poly (ethylene glycol)-block-poly(D,L-lactide) with a mean size of 20–50 nm was approved in clinics in several Asian countries (South Korea, Philippines, India, and Vietnam) for breast cancer, lung cancer, and ovarian cancer [78]. In Genexol-PM, PTX is physically incorporated into the inner core of the micelles that target the tumors via EPR effect. Currently, Genexol-PM in combination with carboplatin is tested for its safety as an adjuvant treatment in patients with newly diagnosed ovarian cancer that underwent cytoreductive surgery [81]. Other polymeric micelles represent a promising vehicle for PTX delivery, and they show similarity with Genexol-PM including a core–shell structure with physical entrapment of PTX, PEG coating, small size, and passive targeting through the EPR mechanism. Despite there are limited evidence of superior efficacy of polymeric-PTX compared to Cremophor-PTX, micelles allow administration of an increased PTX dose and offer improved patient safety. Similar platforms worth to mention are Apalea/Paclical (mean size 20–30 nm) and pm-Pac (mean size 20 nm) that target the tumor via EPR [82][83]. Apalea/Paclical contains retinoic acid to solubilize PTX and is approved in different countries (Russian Federation, Kazakhstan, and European Union) against platinum-sensitive ovarian, peritoneal, and fallopian tube cancer [84][85]. Finally, pm-Pac (mean size 20 nm) successfully passed a Phase III study as first-line treatment in combination with cisplatin for advanced non-small cell lung cancer (NSCLC) [86][87]. Trials (Phase 1–3) dedicated to investigate the benefits of micellar-based technologies are currently ongoing in China [88] and Japan [89] where they showed similar therapeutic benefits compared to PTX, but less toxicity in treating metastatic or recurrent breast cancer. Docetaxel (DTX) is another taxane with solubility issues. An analog of Genexol-PM, called Nanoxel-PM micelles loaded with DTX [90] is currently under clinical trial for efficacy evaluation against different cancers [91]. Additionally, it is tested as neoadjuvant in patients with breast cancer in combination with DOX and cyclophosphamide [92] and against salivary duct carcinoma in combination with anti-HER2 monoclonal antibody [93]. Other versions of this therapeutic formulation are tested in trials as well [93]. Micelle-based technologies are under clinical trial also for evaluating their ability to deliver cisplatin. NC-6004 micelles have an average size of 30 nm and are composed by PEG and poly-glutamic acid copolymers (PGlu). NC-6004 combination with gemcitabine (GEM) has been studied in NSCLC patients, biliary tract, and bladder cancer patients [94] resulting in long-lasting antitumor activity and favorable safety profile. Similar data were registered in combination with Pembrolizumab in the treatment of head and neck cancer [95] and in combination with GEM against advanced solid tumors [96]. Similar formulations are widely investigated [97] including the NK012 where the payload SN-38 is covalently attached to the PGlu structure. Here, the efficacy of NK012 was tested in patients with not-resectable colon cancer, but more data are necessary to evaluate its benefits in comparison with the common treatment irinotecan [98][99]. A novel epirubicin drug conjugated polymeric micelle (NC-6300; 40–80 nm in diameter) was developed by conjugating the payload to PEG polyaspartate block copolymer through a pH-sensitive linker which enables the selective epirubicin release in tumor. This technology exploits tumor pH as targeting, representing a perfect example of smart technology in clinics in the treatment of cutaneous and not cutaneous angiosarcoma [100] and advanced, metastatic, or unresectable solid tumors, including soft-tissue sarcomas [101].3.3. EP0057
EP0057 (formerly known as CRLX101) is a formulation of camptothecin (CPT) conjugated with a cyclodextrin polymer backbone and is currently being evaluated clinically in multiple refractory solid tumors [102][103][104][105][106]. The micelles have a size of approximately 30–40 nm and significantly increase CPT (topoisomerase I inhibitor) solubility while preserving its active lactone form [107]. EP0057 also exhibits better patient tolerance than other CPT analogs. The nanoparticles-drug conjugate is administered via intravenous infusions, and nanoparticles preferentially accumulate in the tumors through EPR [107]. EP0057 has been shown to inhibit significantly also hypoxia-inducible factor-1 alpha (HIF-1α) and therefore serving as a radiosensitizer with the potential to improve the efficacy of chemoradiation therapy [108][109][110]. Prior studies showed EP0057 efficacy in recurrent or persistent, epithelial ovarian, fallopian tube or colorectal, peritoneal, and gastroesophageal cancer [111][112], where it showed promising results [112]. Ongoing clinical trials are designed to evaluate the efficacy and safety (Phase 1/2) of this therapeutic in lung [102], gastric [113] and ovarian [103] cancer in combination with Olaparib, as well as to evaluate its pharmacokinetics properties (PK) [102][114] using a population model. From the data obtained from 27 patients enrolled on two-Phase II clinical trials, the release of CPT was characterized by an initial rapid clearance, which decreased via first-order decay to the steady-state value by 4 h after the infusion. A second Phase I/IIa clinical study involved 22 efficacy-evaluable patients with metastatic renal cell carcinoma, who received increasing doses of EP0057 combined with bevacizumab [106]. Partial response or stable disease was observed in 86% of the patients, with a median progression free survival (mPFS) of 9.9 months. Most patients achieved a reduction of tumor and increased the progression-free survival compared to their previous therapy [115]. In addition, a Phase Ib/II study of EP0057 combined with PTX in women with recurrent epithelial ovarian cancer reported a 31.6% overall response rate, including one complete response with a 5.4 month median progression-free survival [105]. However, the analysis of trials including data highlights the need of more investigation to evaluate the clinical benefits of this therapeutic also because of the onset of considerable side effects [116][117][118][119].3.4. NanoPac
Other attempts to formulate PTX in nanostructure to avoid the use of Cremophore-EL were performed. NanoPac (also known as, Nanotax) are pure PTX nanoparticles generated in supercritical carbon oxide environment in the presence of organic solvents. These particles have a size of 600–800 nm inhibiting their clearance and making their use helpful for topical and local administration (i.e., inhalation) [120], with no targeting mechanism associated. A Phase 2 trial focused on investigating the effects of different concentration of NanoPac against prostate cancer directly injected into the prostate. Interestingly, the lower dose of drug showed higher benefits in terms of tumor reduction compared to higher doses. The drug showed reasonable side effects, also at the highest dose used [121]. In similar experimental settings, other trials measured the ability of intra-cystic injected Nanopac to contrast the progress of pancreatic cancer [122] and of intraperitoneal administration against ovarian cancer [123]. Additionally, in these cases, lower doses of NanoPac showed higher clinical benefits even though the occurrence of side effect was significantly more pronounced.References
- Lammers, T.; Ferrari, M. The success of nanomedicine. Nano Today 2020, 31, 100853.
- Wu, L.-P.; Wang, D.; Li, Z. Grand challenges in nanomedicine. Mater. Sci. Eng. C 2020, 106, 110302.
- Gabizon, A.A.; de Rosales, R.T.; La-Beck, N.M. Translational considerations in nanomedicine: The oncology perspective. Adv. Drug Deliv. Rev. 2020, 158, 140–157.
- Barenholz, Y.C. Doxil®—the first FDA-approved nano-drug: From an idea to a product. In Handbook of Harnessing Biomaterials in Nanomedicine; Jenny Stanford Publishing: Dubai, United Arab Emirates, 2021; pp. 463–528.
- Petre, C.E.; Dittmer, D.P. Liposomal daunorubicin as treatment for Kaposi’s sarcoma. Int. J. Nanomed. 2007, 2, 277.
- Shi, Y.; Van der Meel, R.; Chen, X.; Lammers, T. The EPR effect and beyond: Strategies to improve tumor targeting and cancer nanomedicine treatment efficacy. Theranostics 2020, 10, 7921.
- Chen, L.; Zang, F.; Wu, H.; Li, J.; Xie, J.; Ma, M.; Gu, N.; Zhang, Y. Using PEGylated magnetic nanoparticles to describe the EPR effect in tumor for predicting therapeutic efficacy of micelle drugs. Nanoscale 2018, 10, 1788–1797.
- Agrawal, P.; Singh, R.P.; Kumari, L.; Sharma, G.; Koch, B.; Rajesh, C.V.; Mehata, A.K.; Singh, S.; Pandey, B.L.; Muthu, M.S. TPGS-chitosan cross-linked targeted nanoparticles for effective brain cancer therapy. Mater. Sci. Eng. C 2017, 74, 167–176.
- Adriani, G.; de Tullio, M.D.; Ferrari, M.; Hussain, F.; Pascazio, G.; Liu, X.; Decuzzi, P. The preferential targeting of the diseased microvasculature by disk-like particles. Biomaterials 2012, 33, 5504–5513.
- Attia, M.F.; Anton, N.; Wallyn, J.; Omran, Z.; Vandamme, T.F. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 2019, 71, 1185–1198.
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic: An update post COVID-19 vaccines. Bioeng. Transl. Med. 2021, 6, e10246.
- Evangelopoulos, M.; Parodi, A.; Martinez, J.O.; Tasciotti, E. Trends towards biomimicry in theranostics. Nanomaterials 2018, 8, 637.
- Santagiuliana, R.; Milosevic, M.; Milicevic, B.; Sciumè, G.; Simic, V.; Ziemys, A.; Kojic, M.; Schrefler, B.A. Coupling tumor growth and bio distribution models. Biomed. Microdevices 2019, 21, 33.
- He, C.; Zheng, S.; Luo, Y.; Wang, B. Exosome theranostics: Biology and translational medicine. Theranostics 2018, 8, 237.
- Yamashita, T.; Takahashi, Y.; Takakura, Y. Possibility of exosome-based therapeutics and challenges in production of exosomes eligible for therapeutic application. Biol. Pharm. Bull. 2018, 41, 835–842.
- Bosetti, R.; Jones, S.L. Cost–effectiveness of nanomedicine: Estimating the real size of nano-costs. Nanomedicine 2019, 14, 1367–1370.
- Borodina, T.; Kostyushev, D.; Zamyatnin, A.A., Jr.; Parodi, A. Nanomedicine for Treating Diabetic Retinopathy Vascular Degeneration. Int. J. Transl. Med. 2021, 1, 306–322.
- Parodi, A.; Buzaeva, P.; Nigovora, D.; Baldin, A.; Kostyushev, D.; Chulanov, V.; Savvateeva, L.V.; Zamyatnin, A.A. Nanomedicine for increasing the oral bioavailability of cancer treatments. J. Nanobiotechnol. 2021, 19, 354.
- McMahon, S.J.; Hyland, W.B.; Muir, M.F.; Coulter, J.A.; Jain, S.; Butterworth, K.T.; Schettino, G.; Dickson, G.R.; Hounsell, A.R.; O’sullivan, J.M. Biological consequences of nanoscale energy deposition near irradiated heavy atom nanoparticles. Sci. Rep. 2011, 1, 18.
- Lux, F.; Mignot, A.; Mowat, P.; Louis, C.; Dufort, S.; Bernhard, C.; Denat, F.; Boschetti, F.; Brunet, C.; Antoine, R. Ultrasmall rigid particles as multimodal probes for medical applications. Angew. Chem. 2011, 123, 12507–12511.
- Lux, F.; Tran, V.L.; Thomas, E.; Dufort, S.; Rossetti, F.; Martini, M.; Truillet, C.; Doussineau, T.; Bort, G.; Denat, F. AGuIX® from bench to bedside—Transfer of an ultrasmall theranostic gadolinium-based nanoparticle to clinical medicine. Br. J. Radiol. 2019, 92, 20180365.
- Sancey, L.; Lux, F.; Kotb, S.; Roux, S.; Dufort, S.; Bianchi, A.; Cremillieux, Y.; Fries, P.; Coll, J.-L.; Rodriguez-Lafrasse, C. The use of theranostic gadolinium-based nanoprobes to improve radiotherapy efficacy. Br. J. Radiol. 2014, 87, 20140134.
- Gimenez, Y.; Busser, B.; Trichard, F.; Kulesza, A.; Laurent, J.; Zaun, V.; Lux, F.; Benoit, J.-M.; Panczer, G.; Dugourd, P. 3D imaging of nanoparticle distribution in biological tissue by laser-induced breakdown spectroscopy. Sci. Rep. 2016, 6, 29936.
- Kotb, S.; Detappe, A.; Lux, F.; Appaix, F.; Barbier, E.L.; Tran, V.-L.; Plissonneau, M.; Gehan, H.; Lefranc, F.; Rodriguez-Lafrasse, C. Gadolinium-based nanoparticles and radiation therapy for multiple brain melanoma metastases: Proof of concept before phase I trial. Theranostics 2016, 6, 418.
- Le Duc, G.; Roux, S.; Paruta-Tuarez, A.; Dufort, S.; Brauer, E.; Marais, A.; Truillet, C.; Sancey, L.; Perriat, P.; Lux, F. Advantages of gadolinium based ultrasmall nanoparticles vs molecular gadolinium chelates for radiotherapy guided by MRI for glioma treatment. Cancer Nanotechnol. 2014, 5, 4.
- Lux, F.; Detappe, A.; Dufort, S.; Sancey, L.; Louis, C.; Carme, S.; Tillement, O. Nanoparticules ultrafines en radiothérapie: Le cas des AguIX. Cancer/Radiothérapie 2015, 19, 508–514.
- Mowat, P.; Mignot, A.; Rima, W.; Lux, F.; Tillement, O.; Roulin, C.; Dutreix, M.; Bechet, D.; Huger, S.; Humbert, L. In vitro radiosensitizing effects of ultrasmall gadolinium based particles on tumour cells. J. Nanosci. Nanotechnol. 2011, 11, 7833–7839.
- Luchette, M.; Korideck, H.; Makrigiorgos, M.; Tillement, O.; Berbeco, R. Radiation dose enhancement of gadolinium-based AguIX nanoparticles on HeLa cells. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 1751–1755.
- Radiosensitization of Multiple Brain Metastases Using AguIX Gadolinium Based Nanoparticles. Available online: https://ClinicalTrials.gov/show/NCT02820454 (accessed on 1 October 2022).
- Verry, C.; Dufort, S.; Villa, J.; Gavard, M.; Iriart, C.; Grand, S.; Charles, J.; Chovelon, B.; Cracowski, J.-L.; Quesada, J.-L. Theranostic AguIX nanoparticles as radiosensitizer: A phase I, dose-escalation study in patients with multiple brain metastases (NANO-RAD trial). Radiother. Oncol. 2021, 160, 159–165.
- Radiotherapy of Multiple Brain Metastases Using AguIX®. Available online: https://ClinicalTrials.gov/show/NCT02820454 (accessed on 1 October 2022).
- AguIX Nanoparticles with Radiotherapy Plus Concomitant Temozolomide in the Treatment of Newly Diagnosed Glioblastoma. Available online: https://ClinicalTrials.gov/show/NCT04881032 (accessed on 1 October 2022).
- Stereotactic Brain-directed Radiation with or without Aguix Gadolinium-Based Nanoparticles in Brain Metastases. Available online: https://ClinicalTrials.gov/show/NCT04899908 (accessed on 1 October 2022).
- AguIX Gadolinium-based Nanoparticles in Combination with Chemoradiation and Brachytherapy. Available online: https://ClinicalTrials.gov/show/NCT03308604 (accessed on 1 October 2022).
- Nano-SMART: Nanoparticles with MR Guided SBRT in Centrally Located Lung Tumors and Pancreatic Cancer. Available online: https://ClinicalTrials.gov/show/NCT04789486 (accessed on 1 October 2022).
- Marill, J.; Anesary, N.M.; Zhang, P.; Vivet, S.; Borghi, E.; Levy, L.; Pottier, A. Hafnium oxide nanoparticles: Toward an in vitropredictive biological effect? Radiat. Oncol. 2014, 9, 150.
- Le Tourneau, C.; Moreno, V.; Salas, S.; Mirabel, X.; Calvo, E.; Doger, B.; Florescu, C.; Thariat, J.; Fijuth, J.; Rutkowski, T. Hafnium oxide nanoparticles NBTXR3 activated by radiotherapy as a new therapeutic option for elderly/frail HNSCC patients. J. Clin. Oncol. 2019, 37, 6069.
- Bilynsky, C.; Millot, N.; Papa, A.L. Radiation nanosensitizers in cancer therapy—From preclinical discoveries to the outcomes of early clinical trials. Bioeng. Transl. Med. 2022, 7, e10256.
- NBTXR3 Activated by Radiation Therapy for the Treatment of Locally Advanced or Borderline-Resectable Pancreatic Cancer. Available online: https://ClinicalTrials.gov/show/NCT04484909 (accessed on 1 October 2022).
- NBTXR3, Chemotherapy, and Radiation Therapy for the Treatment of Esophageal Cancer. Available online: https://ClinicalTrials.gov/show/NCT04615013 (accessed on 1 October 2022).
- NBTXR3, Radiation Therapy, Ipilimumab, and Nivolumab for the Treatment of Lung and/or Liver Metastases from Solid Malignancy. Available online: https://ClinicalTrials.gov/show/NCT05039632 (accessed on 1 October 2022).
- NBTXR3, Radiation Therapy, and Pembrolizumab for the Treatment of Recurrent or Metastatic Head and Neck Squamous Cell Cancer. Available online: https://ClinicalTrials.gov/show/NCT04862455 (accessed on 1 October 2022).
- NBTXR3 with or without Cetuximab in LA-HNSCC. Available online: https://ClinicalTrials.gov/show/NCT04892173 (accessed on 1 October 2022).
- NBTXR3 Crystalline Nanoparticles and Radiation Therapy in Treating Randomized Patients in Two Arms with Soft Tissue Sarcoma of the Extremity and Trunk Wall. Available online: https://ClinicalTrials.gov/show/NCT01433068 (accessed on 1 October 2022).
- Bonvalot, S.; Rutkowski, P.L.; Thariat, J.; Carrère, S.; Ducassou, A.; Sunyach, M.-P.; Agoston, P.; Hong, A.; Mervoyer, A.; Rastrelli, M. NBTXR3, a first-in-class radioenhancer hafnium oxide nanoparticle, plus radiotherapy versus radiotherapy alone in patients with locally advanced soft-tissue sarcoma (Act. In. Sarc): A multicentre, phase 2–3, randomised, controlled trial. Lancet Oncol. 2019, 20, 1148–1159.
- Hoffmann, C.; Calugaru, V.; Borcoman, E.; Moreno, V.; Calvo, E.; Liem, X.; Salas, S.; Doger, B.; Jouffroy, T.; Mirabel, X. Phase I dose-escalation study of NBTXR3 activated by intensity-modulated radiation therapy in elderly patients with locally advanced squamous cell carcinoma of the oral cavity or oropharynx. Eur. J. Cancer 2021, 146, 135–144.
- Dulińska-Litewka, J.; Łazarczyk, A.; Hałubiec, P.; Szafrański, O.; Karnas, K.; Karewicz, A. Superparamagnetic iron oxide nanoparticles—Current and prospective medical applications. Materials 2019, 12, 617.
- Lassenberger, A.; Scheberl, A.; Stadlbauer, A.; Stiglbauer, A.; Helbich, T.; Reimhult, E. Individually stabilized, superparamagnetic nanoparticles with controlled shell and size leading to exceptional stealth properties and high relaxivities. ACS Appl. Mater. Interfaces 2017, 9, 3343–3353.
- Cano, M.; Núñez-Lozano, R.; Lumbreras, R.; González-Rodríguez, V.; Delgado-García, A.; Jiménez-Hoyuela, J.M.; de la Cueva-Méndez, G. Partial PEGylation of superparamagnetic iron oxide nanoparticles thinly coated with amine-silane as a source of ultrastable tunable nanosystems for biomedical applications. Nanoscale 2017, 9, 812–822.
- Zhang, Z.-Q.; Song, S.-C. Multiple hyperthermia-mediated release of TRAIL/SPION nanocomplex from thermosensitive polymeric hydrogels for combination cancer therapy. Biomaterials 2017, 132, 16–27.
- Talluri, S.; Malla, R.R. Superparamagnetic iron oxide nanoparticles (SPIONs) for diagnosis and treatment of breast, ovarian and cervical Cancers. Curr. Drug Metab. 2019, 20, 942–945.
- Li, X.; Taratula, O.; Taratula, O.; Schumann, C.; Minko, T. LHRH-targeted drug delivery systems for cancer therapy. Mini Rev. Med. Chem. 2017, 17, 258–267.
- Onbasli, K.; Erkısa, M.; Demirci, G.; Muti, A.; Ulukaya, E.; Sennaroglu, A.; Acar, H.Y. The improved killing of both androgen-dependent and independent prostate cancer cells by etoposide loaded SPIONs coupled with NIR irradiation. Biomater. Sci. 2022, 10, 3951–3962.
- Liu, J.F.; Lan, Z.; Ferrari, C.; Stein, J.M.; Higbee-Dempsey, E.; Yan, L.; Amirshaghaghi, A.; Cheng, Z.; Issadore, D.; Tsourkas, A. Use of oppositely polarized external magnets to improve the accumulation and penetration of magnetic nanocarriers into solid tumors. ACS Nano 2019, 14, 142–152.
- Alvear-Jiménez, A.; Zabala Gutierrez, I.; Shen, Y.; Villaverde, G.; Lozano-Chamizo, L.; Guardia, P.; Tinoco, M.; Garcia-Pinel, B.; Prados, J.; Melguizo, C. Electrospraying as a Technique for the Controlled Synthesis of Biocompatible Ag2S and SPION Nanocarriers with Drug Release Capability. Pharmaceutics 2022, 14, 214.
- Vakili-Ghartavol, R.; Momtazi-Borojeni, A.A.; Vakili-Ghartavol, Z.; Aiyelabegan, H.T.; Jaafari, M.R.; Rezayat, S.M.; Arbabi Bidgoli, S. Toxicity assessment of superparamagnetic iron oxide nanoparticles in different tissues. Artif. Cells Nanomed. Biotechnol. 2020, 48, 443–451.
- Imaging Kidney Transplant Rejection Using Ferumoxytol-Enhanced Magnetic Resonance. Available online: https://ClinicalTrials.gov/show/NCT02006108 (accessed on 1 October 2022).
- Thakor, A.S.; Jokerst, J.V.; Ghanouni, P.; Campbell, J.L.; Mittra, E.; Gambhir, S.S. Clinically approved nanoparticle imaging agents. J. Nucl. Med. 2016, 57, 1833–1837.
- Delayed Sentinel Lymph Node Biopsy in Ductal Cancer In Situ. Available online: https://ClinicalTrials.gov/show/NCT04722692 (accessed on 6 October 2022).
- Pre-Operative Staging of Pancreatic Cancer Using Superparamagnetic Iron Oxide Magnetic Resonance Imaging (SPIO MRI). Available online: https://ClinicalTrials.gov/show/NCT00920023 (accessed on 6 October 2022).
- Magnetic Nanoparticle Thermoablation-Retention and Maintenance in the Prostate: A Phase 0 Study in Men. Available online: https://ClinicalTrials.gov/show/NCT02033447 (accessed on 6 October 2022).
- Radiotherapy with Iron Oxide Nanoparticles (SPION) on MR-Linac for Primary & Metastatic Hepatic Cancers. Available online: https://ClinicalTrials.gov/show/NCT04682847 (accessed on 6 October 2022).
- A Phase I Clinical Trial of Neoadjuvant Chemotherapy with/without SPIONs/SMF for Patients with Osteosarcoma. Available online: https://ClinicalTrials.gov/show/NCT04316091 (accessed on 6 October 2022).
- Diagnostic and Prognostic Accuracy of Gold Nanoparticles in Salivary Gland Tumours. Available online: https://ClinicalTrials.gov/show/NCT04907422 (accessed on 6 October 2022).
- NU-0129 in Treating Patients with Recurrent Glioblastoma or Gliosarcoma Undergoing Surgery. Available online: https://ClinicalTrials.gov/show/NCT03020017 (accessed on 6 October 2022).
- Kumthekar, P.; Ko, C.H.; Paunesku, T.; Dixit, K.; Sonabend, A.M.; Bloch, O.; Tate, M.; Schwartz, M.; Zuckerman, L.; Lezon, R. A first-in-human phase 0 clinical study of RNA interference–based spherical nucleic acids in patients with recurrent glioblastoma. Sci. Transl. Med. 2021, 13, eabb3945.
- Singh, P.; Mijakovic, I. Advances in gold nanoparticle technology as a tool for diagnostics and treatment of cancer. Expert Rev. Mol. Diagn. 2021, 21, 627–630.
- Boogerd, L.S.; Boonstra, M.C.; Beck, A.-J.; Charehbili, A.; Hoogstins, C.E.; Prevoo, H.A.; Singhal, S.; Low, P.S.; van de Velde, C.J.; Vahrmeijer, A.L. Concordance of folate receptor-α expression between biopsy, primary tumor and metastasis in breast cancer and lung cancer patients. Oncotarget 2016, 7, 17442.
- A Study to Evaluate ELU001 in Patients with Solid Tumors that Overexpress Folate Receptor Alpha (FRα). Available online: https://ClinicalTrials.gov/show/NCT05001282 (accessed on 6 October 2022).
- Criscitiello, C.; Morganti, S.; Curigliano, G. Antibody–drug conjugates in solid tumors: A look into novel targets. J. Hematol. Oncol. 2021, 14, 20.
- Davis, M.E. The first targeted delivery of siRNA in humans via a self-assembling, cyclodextrin polymer-based nanoparticle: From concept to clinic. Mol. Pharm. 2009, 6, 659–668.
- Kurreck, J. Proof of RNA interference in humans after systemic delivery of siRNAs. Angew. Chem. Int. Ed. 2010, 49, 6258–6259.
- Zuckerman, J.E.; Gritli, I.; Tolcher, A.; Heidel, J.D.; Lim, D.; Morgan, R.; Chmielowski, B.; Ribas, A.; Davis, M.E.; Yen, Y. Correlating animal and human phase Ia/Ib clinical data with CALAA-01, a targeted, polymer-based nanoparticle containing siRNA. Proc. Natl. Acad. Sci. USA 2014, 111, 11449–11454.
- Safety Study of CALAA-01 to Treat Solid Tumor Cancers. Available online: https://ClinicalTrials.gov/show/NCT00689065 (accessed on 6 October 2022).
- Parvani, J.G.; Jackson, M.W. Silencing the roadblocks to effective triple-negative breast cancer treatments by siRNA nanoparticles. Endocr. Relat. Cancer 2017, 24, R81–R97.
- Davis, M.E.; Zuckerman, J.E.; Choi, C.H.J.; Seligson, D.; Tolcher, A.; Alabi, C.A.; Yen, Y.; Heidel, J.D.; Ribas, A. Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature 2010, 464, 1067–1070.
- Ghezzi, M.; Pescina, S.; Padula, C.; Santi, P.; Del Favero, E.; Cantù, L.; Nicoli, S. Polymeric micelles in drug delivery: An insight of the techniques for their characterization and assessment in biorelevant conditions. J. Control. Release 2021, 332, 312–336.
- Hwang, D.; Ramsey, J.D.; Kabanov, A.V. Polymeric micelles for the delivery of poorly soluble drugs: From nanoformulation to clinical approval. Adv. Drug Deliv. Rev. 2020, 156, 80–118.
- Ghosh, B.; Biswas, S. Polymeric micelles in cancer therapy: State of the art. J. Control. Release 2021, 332, 127–147.
- Cabral, H.; Miyata, K.; Osada, K.; Kataoka, K. Block copolymer micelles in nanomedicine applications. Chem. Rev. 2018, 118, 6844–6892.
- Safety of Genexol PM and Carboplatin as First-Line Therapy in Ovarian Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT05300828 (accessed on 6 October 2022).
- Borgå, O.; Henriksson, R.; Bjermo, H.; Lilienberg, E.; Heldring, N.; Loman, N. Maximum tolerated dose and pharmacokinetics of paclitaxel micellar in patients with recurrent malignant solid tumours: A dose-escalation study. Adv. Ther. 2019, 36, 1150–1163.
- Vergote, I.; Bergfeldt, K.; Franquet, A.; Lisyanskaya, A.; Bjermo, H.; Heldring, N.; Buyse, M.; Brize, A. A randomized phase III trial in patients with recurrent platinum sensitive ovarian cancer comparing efficacy and safety of paclitaxel micellar and Cremophor EL-paclitaxel. Gynecol. Oncol. 2020, 156, 293–300.
- European Medicines Agency. Assessment Report Apealea; European Medicines Agency: Amsterdam, The Netherlands, 2018.
- Apealea®-Elevar Therapeutics. Available online: https://elevartherapeutics.com/apealea-paclitaxel-micellar-elevar/ (accessed on 1 October 2022).
- Shi, M.; Gu, A.; Tu, H.; Huang, C.; Wang, H.; Yu, Z.; Wang, X.; Cao, L.; Shu, Y.; Yang, R. Comparing nanoparticle polymeric micellar paclitaxel and solvent-based paclitaxel as first-line treatment of advanced non-small-cell lung cancer: An open-label, randomized, multicenter, phase III trial. Ann. Oncol. 2021, 32, 85–96.
- Lu, J.; Gu, A.; Wang, W.; Huang, A.; Han, B.; Zhong, H. Polymeric micellar paclitaxel (pm-Pac) prolonged overall survival for NSCLC patients without pleural metastasis. Int. J. Pharm. 2022, 623, 121961.
- Study of Paclitaxel Micelles for Injection in Chinese Patients with Advanced Solid Tumors. Available online: https://ClinicalTrials.gov/show/NCT04778839 (accessed on 6 October 2022).
- Fujiwara, Y.; Mukai, H.; Saeki, T.; Ro, J.; Lin, Y.-C.; Nagai, S.E.; Lee, K.S.; Watanabe, J.; Ohtani, S.; Kim, S.B. A multi-national, randomised, open-label, parallel, phase III non-inferiority study comparing NK105 and paclitaxel in metastatic or recurrent breast cancer patients. Br. J. Cancer 2019, 120, 475–480.
- Study to Evaluate the Efficacy and Safety of Docetaxel Polymeric Micelle (PM) in Recurrent or Metastatic HNSCC. Available online: https://ClinicalTrials.gov/show/NCT02639858 (accessed on 6 October 2022).
- Study to Evaluate the Safety of Nanoxel M Inj. Available online: https://ClinicalTrials.gov/show/NCT04066335 (accessed on 6 October 2022).
- Compare the Efficacy and the Safety of Doxorubicin and Cyclophosphamide Followed by Taxotere versus Doxorubicin and Cyclophosphamide Nanoxel M as Neoadjuvant Chemotherapy in Breast Cancer. Available online: https://ClinicalTrials.gov/show/NCT05207514 (accessed on 6 October 2022).
- Combination of Nanoxel and Herzuma in Salivary Duct Carcinoma. Available online: https://ClinicalTrials.gov/show/NCT03614364 (accessed on 1 October 2022).
- Volovat, S.R.; Ciuleanu, T.-E.; Koralewski, P.; Olson, J.E.G.; Croitoru, A.; Koynov, K.; Stabile, S.; Cerea, G.; Osada, A.; Bobe, I. A multicenter, single-arm, basket design, phase II study of NC-6004 plus gemcitabine in patients with advanced unresectable lung, biliary tract, or bladder cancer. Oncotarget 2020, 11, 3105.
- Osada, A.; Mangel, L.; Fijuth, J.; Żurawski, B.; Ursulovic, T.; Nikolin, B.; Djan, I.; Olson, J.G. Phase IIa/IIb clinical trial of NC-6004 (Nanoparticle Cisplatin) plus Pembrolizumab in patients with head and neck cancer (HNSCC) who have failed platinum or a platinum-containing regimen. Eur. J. Cancer 2020, 138, S35.
- Subbiah, V.; Grilley-Olson, J.E.; Combest, A.J.; Sharma, N.; Tran, R.H.; Bobe, I.; Osada, A.; Takahashi, K.; Balkissoon, J.; Camp, A. Phase Ib/II Trial of NC-6004 (Nanoparticle Cisplatin) Plus Gemcitabine in Patients with Advanced Solid TumorsNC-6004/Gemcitabine in Patients with Advanced Solid Tumors. Clin. Cancer Res. 2018, 24, 43–51.
- A Study to Evaluate the Safety, Tolerability, Pharmacokinetics, and Antitumor Efficacy of Cisplatin Micelle Injection (HA132) in Patients with Advanced Malignant Solid Tumors. Available online: https://ClinicalTrials.gov/show/NCT05478785 (accessed on 1 October 2022).
- Hamaguchi, T.; Tsuji, A.; Yamaguchi, K.; Takeda, K.; Uetake, H.; Esaki, T.; Amagai, K.; Sakai, D.; Baba, H.; Kimura, M. A phase II study of NK012, a polymeric micelle formulation of SN-38, in unresectable, metastatic or recurrent colorectal cancer patients. Cancer Chemother. Pharmacol. 2018, 82, 1021–1029.
- Ri, M.; Suzuki, K.; Iida, S.; Hatake, K.; Chou, T.; Taniwaki, M.; Watanabe, N.; Tsukamoto, T. A phase I/II study for dose-finding, and to investigate the safety, pharmacokinetics and preliminary efficacy of NK012, an SN-38-incorporating macromolecular polymeric micelle, in patients with multiple myeloma. Intern. Med. 2018, 57, 939–946.
- Riedel, R.F.; Chua, V.S.; Kim, T.; Dang, J.; Zheng, K.; Moradkhani, A.; Osada, A.; Chawla, S.P. Results of NC-6300 (nanoparticle epirubicin) in an expansion cohort of patients with angiosarcoma. Oncologist 2022, 27, 809-e765.
- Chawla, S.P.; Goel, S.; Chow, W.; Braiteh, F.; Singh, A.S.; Olson, J.E.G.; Osada, A.; Bobe, I.; Riedel, R.F. A Phase 1b Dose Escalation Trial of NC-6300 (Nanoparticle Epirubicin) in Patients with Advanced Solid Tumors or Advanced, Metastatic, or Unresectable Soft-tissue SarcomaNanoparticle Epirubicin in Solid Tumors and Sarcoma. Clin. Cancer Res. 2020, 26, 4225–4232.
- Trial of EP0057, a Nanoparticle Camptothecin with Olaparib in People with Relapsed/Refractory Small Cell Lung Cancer. Available online: https://ClinicalTrials.gov/show/NCT02769962 (accessed on 1 October 2022).
- EP0057 in Combination with Olaparib in Advanced Ovarian Cancer. Available online: https://ClinicalTrials.gov/show/NCT04669002 (accessed on 6 October 2022).
- A Study of CRLX101(NLG207) in Combination with Weekly Paclitaxel in Patients with Recurrent or Persistent Epithelial Ovarian, Fallopian Tube or Primary Peritoneal Cancer. Available online: https://ClinicalTrials.gov/show/NCT02389985 (accessed on 1 October 2022).
- Duska, L.; Krasner, C.; O’Malley, D.; Hays, J.; Modesitt, S.; Mathews, C.; Moore, K.; Thaker, P.; Miller, A.; Purdy, C. A phase Ib/II and pharmacokinetic study of EP0057 (formerly CRLX101) in combination with weekly paclitaxel in patients with recurrent or persistent epithelial ovarian, fallopian tube, or primary peritoneal cancer. Gynecol. Oncol. 2021, 160, 688–695.
- Voss, M.H.; Hussain, A.; Vogelzang, N.; Lee, J.; Keam, B.; Rha, S.; Vaishampayan, U.; Harris, W.; Richey, S.; Randall, J. A randomized phase II trial of CRLX101 in combination with bevacizumab versus standard of care in patients with advanced renal cell carcinoma. Ann. Oncol. 2017, 28, 2754–2760.
- Weiss, G.J.; Chao, J.; Neidhart, J.D.; Ramanathan, R.K.; Bassett, D.; Neidhart, J.A.; Choi, C.H.J.; Chow, W.; Chung, V.; Forman, S.J. First-in-human phase 1/2a trial of CRLX101, a cyclodextrin-containing polymer-camptothecin nanopharmaceutical in patients with advanced solid tumor malignancies. Investig. New Drugs 2013, 31, 986–1000.
- Gaur, S.; Chen, L.; Yen, T.; Wang, Y.; Zhou, B.; Davis, M.; Yen, Y. Preclinical study of the cyclodextrin-polymer conjugate of camptothecin CRLX101 for the treatment of gastric cancer. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 721–730.
- Kemp, J.A.; Kwon, Y.J. Cancer nanotechnology: Current status and perspectives. Nano Converg. 2021, 8, 34.
- Tian, X.; Nguyen, M.; Foote, H.P.; Caster, J.M.; Roche, K.C.; Peters, C.G.; Wu, P.; Jayaraman, L.; Garmey, E.G.; Tepper, J.E. CRLX101, a Nanoparticle–Drug Conjugate Containing Camptothecin, Improves Rectal Cancer Chemoradiotherapy by Inhibiting DNA Repair and HIF1αCRLX101 Improves Cancer Chemoradiotherapy. Cancer Res. 2017, 77, 112–122.
- Tian, X.; Nguyen, M.; Foote, H.; Garmey, E.; Eliasof, S.; Wang, A. CRLX101, an Investigational Nanoparticle Drug Conjugate of Camptothecin, as a Potentially Effective Radiosensitizer in Chemoradiation Treatment of Colorectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, S49.
- Chao, J.; Lin, J.; Frankel, P.; Clark, A.J.; Wiley, D.T.; Garmey, E.; Fakih, M.; Lim, D.; Chung, V.; Luevanos, E. Pilot trial of CRLX101 in patients with advanced, chemotherapy-refractory gastroesophageal cancer. J. Gastrointest. Oncol. 2017, 8, 962.
- EP0057 in Combination with Olaparib in Relapsed Advanced Gastric Cancer and Small Cell Lung Cancer. Available online: https://ClinicalTrials.gov/show/NCT05411679 (accessed on 1 October 2022).
- Schmidt, K.T.; Huitema, A.D.; Dorlo, T.P.; Peer, C.J.; Cordes, L.M.; Sciuto, L.; Wroblewski, S.; Pommier, Y.; Madan, R.A.; Thomas, A. Population pharmacokinetic analysis of nanoparticle-bound and free camptothecin after administration of NLG207 in adults with advanced solid tumors. Cancer Chemother. Pharmacol. 2020, 86, 475–486.
- Keefe, S.; Hoffman-Censits, J.; Cohen, R.; Mamtani, R.; Heitjan, D.; Eliasof, S.; Nixon, A.; Turnbull, B.; Garmey, E.; Gunnarsson, O. Efficacy of the nanoparticle–drug conjugate CRLX101 in combination with bevacizumab in metastatic renal cell carcinoma: Results of an investigator-initiated phase I–IIa clinical trial. Ann. Oncol. 2016, 27, 1579–1585.
- Combining CRLX101, a Nanoparticle Camptothecin, with Enzalutamide in People with Progressive Metastatic Castration Resistant Prostate Cancer Following Prior Enzalutamide Treatment. Available online: https://ClinicalTrials.gov/show/NCT03531827 (accessed on 1 October 2022).
- A Phase 2 Study of CRLX101(NLG207) in Patients with Advanced Non-Small Cell Lung Cancer. Available online: https://ClinicalTrials.gov/show/NCT01380769 (accessed on 1 October 2022).
- Neoadjuvant Chemoradiotherapy with CRLX-101 and Capecitabine for Rectal Cancer. Available online: https://ClinicalTrials.gov/show/NCT02010567 (accessed on 1 October 2022).
- Topotecan Hydrochloride or Cyclodextrin-Based Polymer-Camptothecin CRLX101 in Treating Patients with Recurrent Small Cell Lung Cancer. Available online: https://ClinicalTrials.gov/show/NCT01803269 (accessed on 1 October 2022).
- Verco, J.; Johnston, W.; Baltezor, M.; Kuehl, P.J.; Gigliotti, A.; Belinsky, S.A.; Lopez, A.; Wolff, R.; Hylle, L.; diZerega, G. Pharmacokinetic profile of inhaled submicron particle paclitaxel (NanoPac®) in a rodent model. J. Aerosol Med. Pulm. Drug Deliv. 2019, 32, 99–109.
- Trial of NanoPac Focal Therapy for Prostate Cancer. Available online: https://ClinicalTrials.gov/show/NCT03077659 (accessed on 1 October 2022).
- Intracystic Injection of NanoPac® in Subjects with Mucinous Cystic Pancreatic Neoplasms. Available online: https://ClinicalTrials.gov/show/NCT03188991 (accessed on 1 October 2022).
- Phase II Study of Intraperitoneal NanoPac® in Patients with Ovarian Cancer. Available online: ://ClinicalTrials.gov/show/NCT03029585 (accessed on 6 October 2022).
More
