Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Keiso Takahashi and Version 2 by Rita Xu.
Endodontic–periodontal lesions (EPLs) are chronic inflammatory lesions in the mouth caused by multiple factors. Both periapical and marginal periodontitis are characterized by infection and inflammation around the affected teeth, suggesting that the theory of complex systems might describe the progression of EPL.
- endodontic–periodontal lesions
- multifactorial disease
- classification
- risk assessment
1. Introduction
Diagnostic difficulties frequently arise in dental practice. These difficulties can make the optimization of dental treatments unclear, as uncertainties in diagnosis may increase the likelihood of treatment risks and iatrogenic errors. For example, clinical findings in patients with endodontic–periodontal lesions (EPLs) can vary widely and include deep periodontal pockets, bleeding on probing, suppuration, and bone resorption [1][2][3][1,2,3] resulting from inflammation around and the destruction of affected teeth. EPLs might be accompanied by infection with multiple types of bacteria, and microflora in infected root canals and periodontal pockets have been reported to be similar [4][5][4,5].
Periodontitis is characterized by chronic/acute infection and inflammation of tooth-supporting tissues and by the loss of connective tissue and alveolar bone [6]. This disease is multifactorial, with patients and teeth differing in susceptibility and resistance to periodontitis depending on individual causal and risk factors [7]. Simple mathematical formulas cannot determine the progression of periodontitis; rather, it may be determined using the theory of complex systems [8]. Approximately 300,000 to 400,000 periodontal ligament fibers were shown to be present on the surface of each root, with the progression of periodontitis determined using a nonlinear chaotic model [9][10][9,10]. The pathogenesis of aggressive periodontitis has been determined by recursive division analysis and immunological assessment of neural networks [11]. The theory of complex systems may also explain the wide heterogeneity of clinical symptoms and the difficulty of treatment and prognosis in patients with EPLs. In addition, endodontic failure caused by iatrogenic errors can affect the progression of EPLs, making a differential diagnosis of EPLs before treatment more difficult than that of periodontitis alone.
The treatment of EPLs should include the removal of bacterial biofilm and products of infectious agents, both in infected root canals and periodontal pockets. The prognosis of EPL has been reported to be poorer than endodontic lesions in patients without periodontitis [12]. EPL mainly involving periodontitis tends to show a poorer prognosis because regenerative periodontal therapy is essential for teeth that are beyond treatment. Moreover, treatment outcomes are dependent on several factors, including the skill of the dentist, patient compliance, healing ability, and the quality of the supportive periodontal therapy program.
Patient-associated factors, including smoking habits, diabetes, parafunction, and socioeconomic status, are involved in the pathogenesis of periodontitis. Similarly, iatrogenic errors during endodontic treatment can influence the prognosis of affected teeth [13][14][13,14]. The re-evaluation of endodontic healing before nonsurgical and/or surgical periodontal therapy for EPL is therefore important [15]. Algorithms and decision trees for the diagnosis and treatment of EPL have been proposed [16][17][16,17].
Technological advances, including cone beam computed tomography (CBCT), microscopy, mineral trioxide aggregates (MTA), and periodontal regenerative treatment, have improved the diagnosis and treatment of EPL. In addition, pre-treatment risk assessment in patients with EPLs can determine the likelihood of a good prognosis. These technologies may improve precision medicine for patients with EPLs.
2. Definition of EPLs
The relationship between pulpal and periodontal disease was first described in 1964 [2]. That study was the first to use the term “retrograde periodontitis”, which indicated periapical periodontitis or periradicular disease. EPLs could be differentiated from marginal periodontitis, so they were therefore defined as lesions due to varying degrees of inflammatory symptoms in both pulpal and periodontal tissues. The simultaneous occurrence of endodontic problems and periodontitis tends to complicate differential diagnoses. Although EPLs have been defined, this definition is not based on rigid scientific evidence or an exact mechanism. EPLs can be classified by etiologic factors, manifestations, and mechanisms of action, with these classifications likely to improve based on new evidence or consensus.3. Classifications of EPLs
A classification of EPLs is summarized in Table 1 [18][19][20][21][22][23][24][25][26][27][18,19,20,21,22,23,24,25,26,27]. EPLs were originally classified into five patterns based on primary lesions [18], but this classification was pragmatic rather than explanatory, and the exact pathogenesis of each remained unclear. An alternative classification based mainly on etiology included both the cause of disease and treatment needs [19]. This classification also included other problematic conditions, such as root perforations, root resorption, root fractures, and grooves, with clinical symptoms similar to those of EPL. An additional classification was based on treatment needs rather than on possible etiology or diagnostic processes [20].Table 1. Systems for the classification of EPLs.
| Authors | Classification Criteria |
|---|---|
| Simon et al. (1972) | Primary lesion |
| Guldner et al. (1985) | Etiology |
| Weine et al. (1989) | Treatment needs |
| Torabinejad and Trope (1996) | Origin of periodontal pocket |
| Meng (1999) | Primary lesion |
| Abott (2009) | Presence or absence of communication of EPL |
| Singh (2011) | Presence or absence of iatrogenic lesion |
| Al-Fouzan (2014) | Primary disease with its secondary effect |
| Herrera et al. (2018) | Presence or absence of root damage, periodontitis, and three grades |
4. Clinical Manifestations and Examinations
The most common clinical manifestations of EPL include abscess formation, deep periodontal pockets, and bone resorption on X-ray photographs and/or CBCT due to bacterial infection and host inflammatory reactions. Patients may experience discomfort, occlusal and/or spontaneous pain, purulent exudate, sinus tract infection, gingival swelling, and increased mobility of affected teeth. Incomplete or excessive root canal fillings and apical radiolucency on X-ray suggest that periapical periodontitis resulting from inadequate root canal treatment is usually involved in the pathogenesis of EPL. Patients suspected of EPL should be evaluated by endodontic and periodontal examinations, including electric pulp tests, pocket probing, X-ray photographs, CBCT, and medical interviews. Other factors that should be assessed include personal data, such as age, history of the disease, iatrogenic errors, trauma, and susceptibility to periodontitis. A full mouth examination is recommended to evaluate the severity of periodontitis and its risk for progression, and an occlusal examination is required to assess the possible causes of VRF, including parafunction, night bruxism, and tooth-contacting habits. Surgical inspection may reveal tooth cracks, VRF, perforation, and cemental tears, which can cause inflammatory symptoms.5. Risk Assessment of EPLs
Many factors have been associated with each EPL (Figure 1), including factors associated with periapical and marginal periodontitis. Dental caries, trauma, failure of endodontic treatment (iatrogenic factors), and advanced periodontitis, including retrograde pulpitis and furcation involvement, may affect periapical outcomes. Other factors include the clinical experience and skills of the dentist. To date, however, few diagnostic tools are available to determine endodontic failure due to various iatrogenic errors before treatment.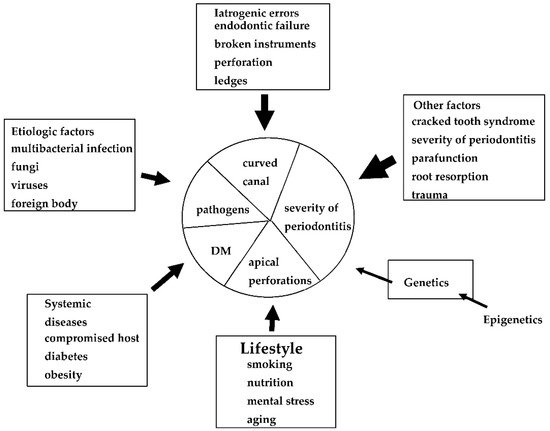
Figure 1. Possible causes, risk factors, and predisposing factors associated with EPLs. These factors may influence the progression and pathogenesis of each EPL.
