Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Jamir Pitton Rissardo and Version 3 by Beatrix Zheng.
Pimavanserin (PMV) is the first approved drug for treating hallucinations and delusions in Parkinson’s disease (PD) psychosis. Psychosis is one of the leading causes of nursing home placement in people with PD. Furthermore, hallucinations are a more frequent cause of institutionalization than motor disability or dementia related to PD. The management of PD psychosis involves antipsychotic medications. Most of the drugs in this class directly block dopamine D2 receptors, leading to significantly worsening motor symptoms in patients with PD. The most commonly used medications for managing PD psychosis are quetiapine, clozapine, and PMV.
- pimavanserin
- Nuplazid
- ACP-103
- Parkinson’s disease
- psychosis
1. Pimavanserin Clinical Trials
The results of the clinical trials related to the PMV indicated for PD psychosis are summarized in Table 13 [1][2][16,25]. A table was uploaded in the SupplementarySupplementary Materials Materials (https://www.mdpi.com/article/10.3390/brainsci12101286/s1) with all the clinical trials related to pimavanserin registered on ClinicalTrials.gov (Supplementary Material S3). Moreover, a figure is provided with the conditions assessed in these clinical trials (Figure 13) [3][4][5][6][7][8][37,38,39,40,41,42]. Refer to the SupplementarySupplementary Materials Materials for the mechanism proposed by 5-HT2A and schizophrenia, Tourette syndrome, depressive disorder, impulsivity, dyskinesia, and insomnia (Supplementary Material S4).
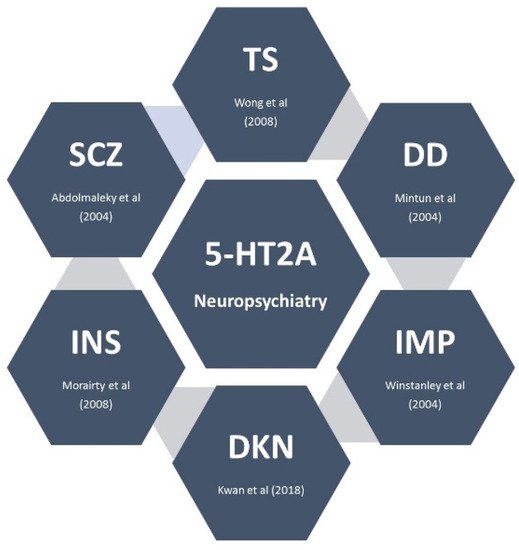
Figure 13. Neuropsychiatric disorders and 5-HT2A receptor. This figure summarizes the conditions studied in the clinical trials with pimavanserin. Abbreviations: IMP: impulsivity; INS: insomnia; DD: depressive disorder; DKN: dyskinesia; SCZ: schizophrenia; TS: Tourette syndrome [3][4][5][6][7][8][37,38,39,40,41,42].
Table 13.
Clinical trials of pimavanserin in the management of Parkinson’s disease psychosis.
| Study | NCT00658567 | NCT00477672 | Meltzer et al. | Cumming et al. (NCT01174004) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
Table 24.
Pimavanserin clinical experience by Dashtipour et al. adapted by Rissardo et al.
| 1. Low PMV dose (17 mg/day; 10 mg/day) may be effective in some patients | ||||||||||
| 2. PMV may be added without disrupting or adversely affecting other multidrug PD regimens | ||||||||||
| 3. PMV may be effective for managing PD psychosis in individuals with deep brain stimulation | ||||||||||
| 4. PMV and another antipsychotic may be necessary to manage PD psychosis | ||||||||||
| 5. After controlling PD psychosis symptoms with PMV, clinicians can increase the dose of dopaminergic drugs for better motor control | ||||||||||
| Year | 2009 | 2009 | 2010 | 2014 | ||||||
| Type of study | Randomized parallel assignment, quadruple masking | Randomized parallel assignment, quadruple masking | Multicenter, randomized, placebo-controlled, double-blind | Randomized parallel assignment, quadruple masking | ||||||
| Total number of participants | 123 | 298 | 60 | 199 | ||||||
| Intervention | Pimavanserin 10–20 mg and placebo | Pimavanserin 10–40 mg and placebo | Pimavanserin 20–60 mg | Pimavanserin 40 mg and placebo | ||||||
| Primary outcome | Change in SAPS score from baseline to day 42 | Change in SAPS score from baseline to day 42 | Change in SAPS score from baseline to day 28 | Change in SAPS score from baseline to day 43 | ||||||
| Secondary outcome | Change in UPDRS II/III score from baseline to day 42 | Change in UPDRS II/III score from baseline to day 42 | Change in UPDRS II/III score from baseline to day 28 | Change in UPDRS II/III score from baseline to day 43 | ||||||
| Groups | PMV10 | PMV20 | Pla | PMV10 | PMV40 | Pla | PMV | Pla | PMV | Pla |
| N | 41 | 41 | 39 | 99 | 98 | 98 | 29 | 31 | 95 | 90 |
| Age mean (SD) | 71 (7.4) | 72.1 (8.2) | 73 (7.9) | 69.0 (8.6) | 69.4 (7.8) | 69.6 (9.7) | 72.3 (1.4) | 69.6 (1.6) | 72.4 (6.6) | 72.4 (7.9) |
| Sex (male) | 26 | 24 | 27 | 63 | 74 | 51 | 26 | 20 | 64 | 52 |
| Race (white) | - | - | - | - | - | - | 28 | 31 | 90 | 85 |
| Primary endpoint | - | −6.5 | −4.4 | −5.8 | −6.7 | −5.9 | −1.9 | −0.2 | −5.7 | −2.7 |
| Secondary endpoint | - | −3.9 | −1.8 | −1.4 | −3.1 | −2.9 | −3.0 | −3.8 | −1.6 | −1.4 |
SAPS: Scale for the Assessment of Positive Symptoms. UPDRS: Unified Parkinson’s Disease Rating Scale (UPDRS) Part II (Activities of Daily Living) and Part III (Motor Examination) PMV: pimavanserin; Pla: placebo. NCT00658567 and NCT00477672 data extracted from ClinicalTrials.gov.
Eight clinical trials of PMV and PD psychosis are registered: NCT02762591, NCT00477672, NCT00658567, NCT01174004, NCT01518309, NCT00550238, NCT04292223, and NCT04373317. The total number of enrolled people with PD psychosis is estimated at 1529. However, thwe researchers only have complete results already published in four studies. NCT02762591 was registered to provide patients with PD psychosis access to pimavanserin until the product received marketing approval from the US FDA and is commercially available.
The primary outcome of the clinical trials involved two types of SAPS scales. NCT00658567, NCT00477672, and Meltzer et al. assessed SAPS-H+D. On the other hand, NCT01174004 assessed SAPS-PD. The secondary outcome of the clinical trials was the influence of PMV on motor symptoms, which was investigated with the Unified Parkinson’s Disease Rating Scale (UPDRS) Part II (Activities of Daily Living) and Part III (Motor Examination).
Meltzer et al. also studied other scales such as Parkinson’s Psychosis Rating Scale (PPRS), Clinical Global Impression—Severity (CGI-S), and Epworth Sleepiness Scale (ESS). Cummings et al. assessed Mini-Mental Status Examination (MMSE), Neuropsychiatric Inventory (NPI), Clinical Global Impression—Severity (CGI-S), and Caregiver burden scale (CBS). Refer to the SupplementarySupplementary Materials Materials for a complete description of the scales used for the clinical trials related to PMV and PD psychosis (Supplementary Material S5) [9][10][11][12][13][14][15][16][17][18][43,44,45,46,47,48,49,50,51,52].
2. Pimavanserin Clinical Experience
2.1. Pimavanserin Efficacy
The approval of PMV by the FDA with only one “pivotal trial” and modified scales for psychosis assessment left some experts in doubt about the effectiveness of PMV [1][16]. However, the clinical trial for approval was not the only study that showed efficacy. Two other clinical trials developed simultaneously showed significant results for PMV in PD psychosis management. Moreover, the changes in scales were probably needed due to their low specificity for PD symptoms and broad range scoring system, which went from zero to 20 items. Furthermore, SAPS-H+D was aimed at assessing psychotic symptoms of schizophrenia [15][49]. Additionally, this scale assesses various types of hallucinations and delusions that are not commonly associated with PD [13][47]. The new SAPS-PD scale ranges from zero to nine items and is specifically designed for psychosis associated with PD [16][50].
Mansuri et al. aimed to evaluate the safety and efficacy of PMV in treating PD psychosis on the basis of data from four clinical trials with complete published results [19][53]. They observed that PMV was associated with a significant reduction in psychosis (SAPS, mean difference: –1.55 [–2.71, –0.379], p = 0.009). The groups had similar composite scores for motor symptoms. Interestingly, PMV was protective against orthostatic hypotension (risk ratio: 0.33 [0.30, 0.37], p < 0.001).
Currently, no clinical trials have compared atypical antipsychotics and PMV to manage PD psychosis. In this way, a network meta-analysis between clozapine and PMV was performed to assess the efficacy and safety of PMV compared to atypical antipsychotics for psychosis in PD [20][54]. The researchtudy involved 17 clinical trials and showed that clozapine is efficacious with a low impact on motor functions. An important fact is that PMV efficacy is inferior to clozapine. Notwithstanding, PMV has a favorable profile for treating psychosis in PD.
Isaacson et al. evaluated the efficacy and tolerability of PMV in an open-label extension study for a more extended period [21][55]. They observed that the beneficial effects of PMV in the 6 week core study were maintained, supporting the durability of response to PMV. Sellers et al. showed similar results with clinical improvement in psychosis in 76% of the individuals, which was maintained for a long-term follow-up of 2 years [22][56]. Moreover, cognitive impairment and deep brain stimulation do not alter the effect of PMV. However, subjects with earlier PD psychosis onset may respond better to PMV [23][57].
2.2. Switching from Off-Label Antipsychotics to Pimavanserin
Some patients might require switching from off-label antipsychotics to PMV due to inefficacy in improving psychotic symptoms or emergence of severe side-effects. Black et al. published a consensus recommending adding PMV 34 mg daily to the continuous quetiapine dose for 4 weeks and continuing clozapine for 6 weeks, followed by tapering antipsychotics [24][58]. High-dose quetiapine (>100 mg/day) should be reduced by 50% weekly until reaching 12.5 mg/day and then withdrawn. Low-dose quetiapine (<100 mg/day) should be reduced by 25% weekly until reaching 12.5 mg/day and then removed. High-dose clozapine (>100 mg/day) should be reduced by 25 mg weekly until discontinued. Low-dose clozapine (<100 mg/day) should be reduced by 6.25 mg weekly until discontinued. While tapering the antipsychotics, if the patient has an emergence of psychosis, the prescriber can return to the previous dose level, and the tapering should be attempted again after 1 week.
2.3. Post-Marketing Surveillance and Experience
Concerns about PMV safety have been expressed by consumer watchdogs such as the Institute for Safe Medical Practices and the popular press [25][59]. Moreover, a study assessing the Medicare database showed that patients taking PMV for PD psychosis, compared to those with no treatment over 1 year, had an increased risk for death [26][60]. Nevertheless, another study of the Medicare database revealed that mortality was about 35% lower with PMV during the first 6 month follow-up period than with atypical antipsychotics for managing PD psychosis [27][61].
Brown et al. retrospective analyzed the adverse event case reports submitted to the FDA’s Adverse Event Reporting System (FAERS) from 2016 through 2019 [28][62]. They aimed to compare PMV with treatment alternatives and other atypical antipsychotics within a population of people with PD psychosis. Their results showed that PMV was not associated with excess reports of death. Additionally, Brown et al. noticed a substantial bias related to reports of PMV adverse events in 2018, probably associated with consumer safety groups and media reports, raising concerns based on the absolute numbers of death reports in individuals receiving PMV.
Ballard et al. performed a multiyear, open-label study assessing the long-term safety and tolerability of PMV [29][63]. Long-term treatment with pimavanserin 34 mg once daily demonstrated a favorable benefit/risk profile with no unexpected safety concerns. Mortality rates suggested no increased risk following long-term therapy. The study was performed for 11 years and revealed that the most common side-effects were falls, urinary tract infections, and hallucinations.
A recent cohort study after sensitive statistical analysis demonstrated a decreased risk of falls and fractures in patients with PD psychosis treated with PMV versus atypical antipsychotics [30][64]. The incidence ratio estimated was 0.55 (95% CI 0.34–0.86). Therefore, additional research is warranted when PMV is more widely used among patients with PD psychosis.
2.4. Pimavanserin Clinical Experience
PMV, when available, should be the first-line therapy for managing PD psychosis. Furthermore, this drug should be started at symptom onset since PD psychosis progression is unpredictable. Atypical antipsychotics are recommended as a second choice for PMV when PD psychosis is not sufficiently controlled. Low-dose quetiapine may be a second-line agent in an initial trial [31][15].
Dashtipour et al. reported a case series of PMV treatment for PD psychosis with clinical tips. Table 24 was adapted from the study of Dashtipour et al. [32][65]. It is worth mentioning that US prescribers of PMV must provide medical documentation of psychosis and the reason for its indication, which can sometimes affect the use of PMV for behavioral management [33][66].
In cases of PMV-resistant psychosis, one possible approach is PMV tapering and clozapine titration. Lake et al. reported an elderly female with PD psychosis resistant to quetiapine and PMV monotherapy regimen. A trial of clozapine after a suboptimal response to PMV led to further symptom improvement [34][67]. Noteworthily, the decision should have a patient-centered approach due to the high potential side-effect burden.
PMV was first approved with the recommended swallowing of the entire capsule or tablet. Recent studies revealed that food does not affect PMV bioavailability. Moreover, PMV can be given orally by emptying the capsule contents into soft foods or liquids. Some examples of the tested products in which PMV capsules were opened and the contents sprinkled are applesauce, orange juice, and water [35][68].
Another important clinical topic is the possible interactions of PMV with medicines used in the pharmacotherapy of patients with PD. PMV could have a synergistic effect on the prolongation of QT when combined with other drugs that affect QT. However, Bugarski-Kirola et al. showed that this theoretical adjunctive PMV effect with background antipsychotic treatments is not clinically significant [36][69].
