Ventricular assist devices (VADs) have been considered a reasonable alternative strategy in advanced heart failure (HF), widely used as a bridge to heart transplantation or candidacy. Mechanical unloading supports the function of a failing heart and the perfusion of vital organs through reduced workload placed on the ventricles. In clinical practice, it might initiate a healing response with even myocardial recovery, making heart transplantation and mechanical support no longer required [7].
- heart failure
- therapy
- VADs
- LVAD
- mechanical unloading
- myocardial recovery
- cardiomyocytes
- mitochondria
- metabolism
1. Mechanical Unloading of Failing Heart
1.1. Ventricular Assist Devices (VADs)
1.2. The Current Status of Left Ventricular Assistance Devices (LVADs) Therapy in Heart Failure
Over the past decade in the United States, 25,551 patients with heart failure underwent continuous-flow LVADs placement [2]. According to the 2021 European Society of Cardiology (ESC) Guidelines, LVAD implantation may be recommended when symptoms persist, despite optimal medical treatment, and the absence of severe right ventricular dysfunction and/or tricuspid regurgitation [3]. Furthermore, a potential patient must have at least one of the following: LVEF < 25% and unable to exercise or able but with peak VO2 < 12 mL/kg/min and/or <50% predicted value, ≥3 HF hospitalizations without an obvious precipitating cause (during 12 months), dependence on inotropic therapy or temporary MCS, and progressive end-organ dysfunction. Great emphasis is also put on stable psychosocial background and support from society. Living alone and having poor overall mental health is a contraindication to the same extent as infection, severe renal dysfunction, and ventricular arrhythmias. Currently, there are three therapeutic goals for LVAD implantation: bridge to transplantation (BTT), bridge to candidacy (BTC), and destination therapy (DT). In the BTT regimen, the device supports the patient and improves physiology until a donor becomes available. In turn, BTC provides time for the patient to become eligible for cardiac transplantation by, for example, decreasing body mass index, achieving a required cancer-free period, or securing financial and family support. The last alternative option is DT for patients with end-stage HF and transplantation contraindications, which allows for discharge from the hospital and improves the quality of life. The annual report from Interagency Registry for Mechanically Assisted Circulatory Support (Intermacs) has shown that DT is currently the most common form of therapy [2]. The importance of BTT has decreased and become the rarest therapeutic target (8,9% of total implantations). The advantage of long-term use started in 2015 (nearly 50% of total implantations), reaching its peak in 2019 (73,1%) [2][4]. Interestingly, the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (RE-MATCH) showed that patients randomized to receive LVAD as DT lived longer in better health in comparison to the subjects with optimal pharmacological treatment [5]. Moreover, the main cause of death was not terminal HF as in the medical group but systemic infection and device malfunction.1.3. Bridge to Recovery
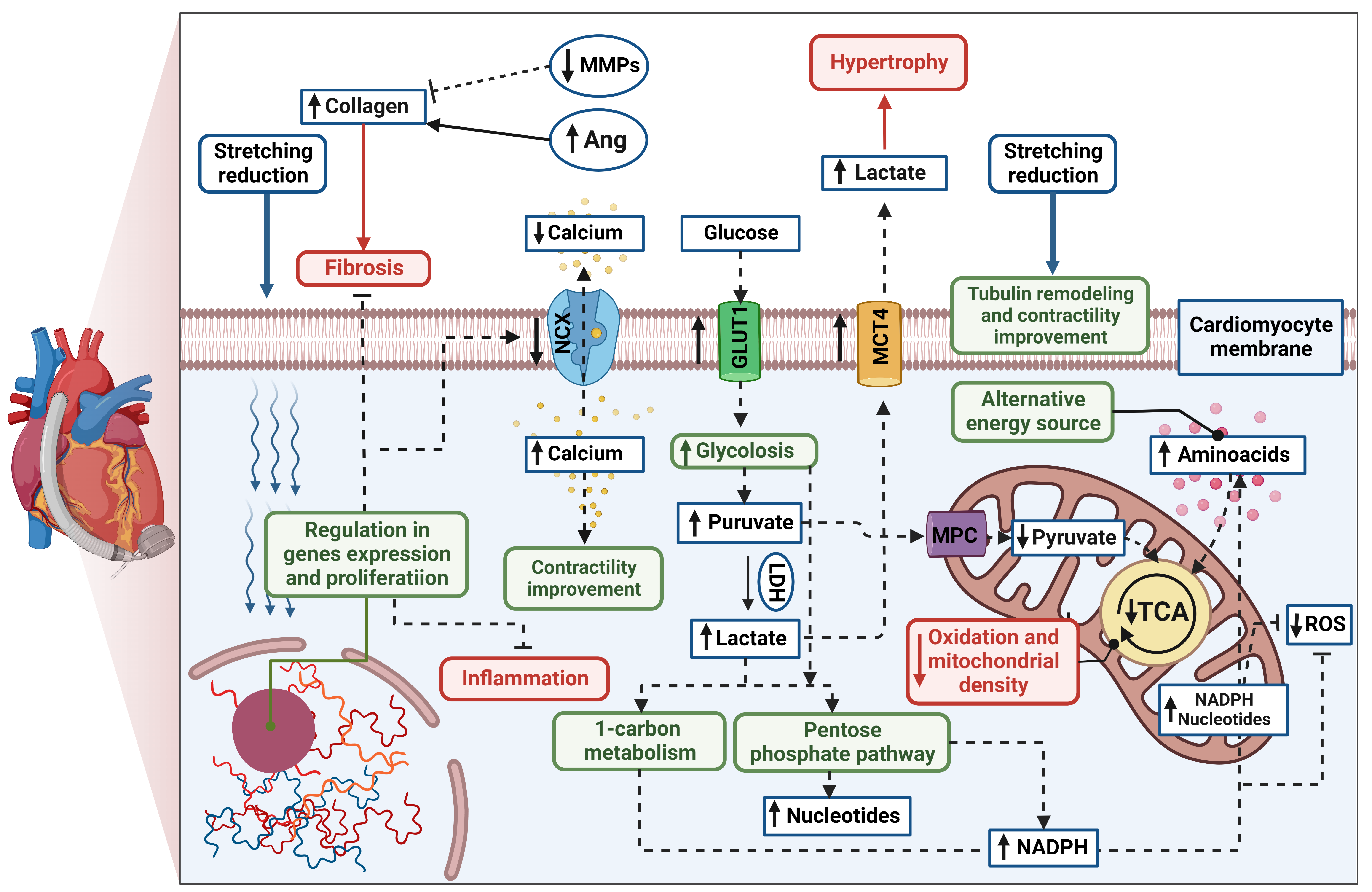
A growing body of evidence has shown that, in respondent patients, LVAD induces structural and functional changes at the cellular, molecular, and whole-heart levels, known as reverse remodelling [6][7][8]. The cellular processes are thought to be more profound and more significant than the changes observed in cardiac function. The potential mechanism of cardiomyocyte remodelling is irreversibly connected to its stretching reduction (Figure 1). Hemodynamic support stimulates karyokinesis and favours the ability to divide, which was confirmed by increasing diploid cardiomyocytes in myocardial samples [9]. An increased number of circulating progenitor cells might correlate to ongoing cardiac recovery; however, their number seems to be transient over time [10][11]. Particular attention has been paid to the specific gene expression in human unloaded hearts, such as expression of profibrotic, contractile, involved in Ca2+ cycling, and proinflammatory proteins [12][13][14]. Reduced level of cytokines was found both in serum and myocardial tissue in patients with improved cardiac function after LVAD implantation compared to the non-responder group [15]. Interestingly, the signal transducer and activator of transcription 3 (STAT3) was responsible for modulating the immune response. Moreover, pre- and post-intervention levels of cytokine were correlated with further LV improvement, suggesting inflammation is an essential factor of LVAD response. It has been highlighted that levels of cytokines in the myocardium, especially tumour necrosis factor (TNF), might predict patients’ recovery [15][16]. The systolic function improvement is thought to be initiated by preserving the abundance of key regulatory proteins (sarcoplasmic reticulum calcium adenosine triphosphatase, SERCA) and a decrease in the Na+/Ca2+ exchanger (NCX) during LVAD therapy [17]. It results in greater calcium uptake and contributes to greater cardiac contractility [18]. Furthermore, mechanical unloading has improved Ca2+ handling through significant tubule remodelling [19]. It has been shown that the density and activity of L-type Ca2+ channels and transverse tubules (t-tubule) have been normalized in the rodent model of mechanical unloading compared to unfavourable outcomes from only HF rats. T-system defects and related-Ca2+ handling aberration are features of heart failure progression and, hence, are thought to be the key to the proper functioning of cardiomyocytes and novel predictors for functional cardiac recovery after mechanical unloading [19][20]. Mechanical support also plays an ambiguous role in extracellular matrix (ECM) remodelling. Lower profibrotic gene expression might contribute to reduced collagen content [21][22]; however, some studies indicated increased fibrosis in heart samples after LVAD support. It can be explained by the decreased breakdown (through decreased activity matrix metalloproteinases activity, MMPs) and increased synthesis of collagen (via increased activity of angiotensin I and II; Ang), which were reported [23][24]. However, ECM turnover is highly related to the aetiology of the injury, RV function, patient’s age, or type of LVAD support, making the influence of mechanical support difficult to determine [25]. Metabolic changes and cellular pathways play a pivotal role in reverse remodelling. It has been reported that effective hemodynamic support induces glycolysis and increases glycolytic metabolites without directing them through the tricarboxylic acid cycle (TCA) [26]. To provide an alternative energy source, the increased level of amino acids was found as a compensatory mechanism. Mitochondrial volume density and mitochondrial DNA (mtDNA), although significantly lower at implantation time compared to the healthy control, have slightly increased during mechanical unloading. Similar results were confirmed in further study, where up-regulated glycolysis initiated activation of protective pathways, such as the pentose phosphate pathway and 1-carbon metabolism in post-LVAD responders [27]. This specific mechanism protects cells against reactive oxygen species (ROS) and increases the synthesis of nucleotides. Furthermore, restoration of the pyruvate–lactate axis was recently highlighted as a predictor of myocardial recovery [28]. Overall, mechanical support causes cascades of reactions in which gene expression, proliferation, apoptosis, fibrosis, immune response, and cardiomyocyte metabolism are modulated. Some of these changes provide prognostic value, and others are the reason why not all LVAD patients achieve myocardial recovery.
1.4. LVAD Limitations
Limitations regarding myocardial recovery might be divided into two categories: adverse events and unfavourable changes in cardiomyocytes, both associated with prolonged mechanical unloading. In the first case, LVAD patients struggle with many post-implantation complications, with bleeding being the most frequent but not the most dangerous [29]. Multisystem organ failure (16.4%), stroke (15.6%), heart failure (12.5%), and major infection (5.7%) cause half of the deaths in the LVAD population [2]. Continuous flow is thought to increase the risk of gastrointestinal bleeding, lack of pulse, and thromboembolic complications [30]. Despite technological progress and novel medical solutions, adverse events, such as bleeding, right heart failure, and infections, continue to be limiting factors in sustained recovery. LVAD patients should routinely assess predictor factors by echocardiographic assessment and biochemical parameters in their referring centre, which has become difficult due to the COVID-19 pandemic [31]. Noteworthily, LVAD is not fully implantable, and the external system controller with a driveline protruding from the patient’s abdomen might negatively affect physical and mental health, requiring the patient’s acceptance. Secondarily, the prolonged hemodynamical support might produce an “atrophic”, proinflammatory, and profibrotic response, with mitochondrial dysfunction as well. Therefore, clinical improvement might occur early during LVAD or not, with/without time regression [32]. Overall, mechanical unloading is speculated not to be sufficient to achieve total heart recovery without amelioration of detrimental factors. Thus, the development of a novel target treatment is urgently needed.2. Combination of Mechanical Unloading and Pharmacotherapy for Chronic Heart Failure Treatment
2.1. Potential Benefits
The effectiveness of LVAD therapy is evidenced by a sufficient myocardial recovery that allows device explantation and life without mechanical support [33]. To increase the number of patients who achieved those goals, combination therapy was first proposed in 2001 to “maximize the efficacy of LVAD as BTR” [34]. The basis of combination therapy has become the drive to reverse cardiac remodelling, followed by the stimulation of physiological cardiomyocyte growth. This formed the “Harefield protocol” in which LVAD therapy was enlarged by clenbuterol [35]. After 5 years, the Harefield protocol was tested as a combination of mechanical unloading with specific drug therapy for 15 patients with severe HF due to nonischaemic cardiomyopathy [36]. In the pharmacological regimen, four HF medications reduced LV remodelling, and then clenbuterol was administered to prevent myocardial atrophy, which had been proven in prior studies [37][38][39]. The examination showed significant cellular and functional improvement, which translated into a high rate of survival and recovery with combination treatment. This is of particular note given that, at that time, LVAD therapy was associated with only a small percentage of recovery sufficient for device explantation (5% [40], 8% [41]) and an equal chance of 1-year survival [5]. Further, the same strategy was enlarged to 20 patients with dilated cardiomyopathy and demonstrated great utility and effectiveness [42]. Concentrating on survival and durability of recovery, Birks et al. demonstrated a significantly high rate of heart failure reversal. The promotion of reversed remodelling has also been described in another pharmacologic regimen. In the study of Grupper et al., patients who had ischemic cardiomyopathy were randomly assigned to the neurohormonal blockade (NHB) therapy (receiving ACE, ARB, BB, or AA) or the control group without any NHB drug after LVAD implantation[43]. Achieving progressive normalization, the NHB patients experienced greater myocardial recovery and down-regulation of neurohormones after 6 months. A different strategy might be the pre-operative use of sacubitril–valsartan (ARNI: angiotensin receptor antagonist and neprilysin inhibitor) to reduce post-operative mortality in patients undergoing LVAD implantation. Heder et al. reported an association with better survival outcomes after cardiac surgery (LVAD or HTx) [44]. According to Kaplan and Meier’s analysis, the lowest rate of death was observed in ARNI (13.6%), then ACEi, ARB (19.4%), and, lastly, the no-vasoactive group, with the worst 30-day survival rate (62.5%; p = 0.043). It has been previously reported that angiotensin–neprilysin inhibition reduces NT-proBNP levels in patients with acute HF, with no greater incidence of renal dysfunction, hyperkalaemia, and symptomatic hypotension [45]. A combined approach was also examined in a rodent model of HF using the established and reproducible procedure of LV unloading [46]. Since chronic support might cause alteration in Ca2+ cycling, increase fibrosis, and induce myocardial atrophy [47][48], Navaratnarajah et al. selected ivabradine (Iva) as a proven agent to counteract these deleterious effects [46]. It has been reported that 4 weeks of combined treatment was successful in two of three key determinants but did not prevent myocardial atrophy. In summary, The Harefield protocol was one of the first studies to successfully combine pharmacological agents with LVAD. Particularly interesting are higher rates of recovery when adjuvant medical therapy is included in the LVAD strategy. Therefore, this strategy could modulate the detrimental effects of prolonged mechanical unloading and promote reverse remodelling.2.2. Novel Pharmacotherapies for Cardiomyocyte Regeneration during LVAD Support
2.2.1. Stimulation of Cardiomyocyte Proliferation
Mechanical unloading is associated with cardiomyocyte atrophy, resulting in a decline in myocyte densities and LV mass continuously [49][50]. The hypertrophy regression is speculated to attenuate heart recovery, but it is not fully proven whether it is related to mechanical unloading or the pathophysiology of HF itself [51][52]. However, a few clinical strategies in which cardiomyocyte proliferation is successfully stimulated might be beneficial for durable cardiac recovery. Regenerative therapy is based on embryonal or adult stem cells as an effective therapeutic target for cardiogenesis and angiogenesis. The main goal of this strategy is to boost cell production directly and then indirectly to improve cardiac function by injecting stem cells into a wounded region of the heart [53]. In prior experimental studies, the function and volume of LV, as well as the size of the infarction, have been improved after receiving millions of potential heart cells [54][55][56].. In turn, clinical trials are not entirely consistent on whether stem-cell-based therapy could promote cardiac recovery in HF [57][58] or the LVAD population only [59][60][61].2.2.2. Regulators of Cardiac Substrate Metabolism
Cardiac metabolism plays a central role in the pathophysiology of HF [62]. Its alterations profoundly impair cardiac function and develop further progression. Metabolic modulators are recently thought to display therapeutic potential in cardiovascular diseases [63][64]. The reduction in fatty acid (FA) oxidation is one of the starting points. In normoxia, FA breakdown is the main source of ATP (about 70%), alongside glucose and lactate [65]. It should be noted that energy production from glucose requires less oxygen than FA, which is crucial in ischemia conditions [66]. Therefore, decreased FA metabolism has been reported in many animal models, also related to left ventricle dysfunction, and it is mainly observed not in an early but advanced stage of HF [67][68][69]. It might be caused by the lower energy demand and optimized ATP production or, as previously mentioned, directing glucose into alternative and more beneficial pathways. Thus, the new therapeutic approach for LVAD patients might be the regulation of FA oxidation in favour of glycolysis to generate biomolecules promoting the normal energy state of cardiomyocytes [70]. Perhexiline, a drug developed for angina, was proven to be simultaneously favourable for hemodynamic and metabolic cardiac function in cardiovascular disease [71][72][73]. It raises glucose utilization and decreases beta-oxidation through inhibition of fatty acids mitochondrial transporter (carnitine palmitoyltransferase-1) [71][74]. It has been shown that perhexiline increases the energetic state (PCr/ATP ratio; 1.16 to 1.51) and left ventricular systolic function (LVEF; 24% to 34%) in HF [71][75]. Another mitotrope, trimetazidine, is also thought to have potential cytoprotective effects in HF treatment [76]. It might enhance cardiac function by preventing cardiomyocytes from many deleterious events, such as apoptosis, fibrosis, and inflammation [77][78][79]. Therefore, trimetazidine has been clinically investigated, and an increase of EF by 3.9% [80] or 7% alongside 17 ml left ventricular end-systolic volume decreasing has been reported [81]. Sodium/glucose cotransporter 2 (SGLT2) inhibitors are thought to be promising cardioprotective agents in cardiovascular diseases. SGLT2 inhibitors are speculated to not only regulate glucose concentration but also homeostasis and associated parameters (blood pressure, haematocrit, and sodium level) [82][83][84]. All these changes act favourably on circulatory unload and ventricular stress, reducing the likelihood of cardiovascular death. Since volume overload impairs right ventricle function, leading to hypertrophy and fibrosis, these specific inhibitors might prevent right ventricular failure and promote myocardial recovery after LVAD implantation. The selective agonists of peroxisome-proliferator-activated receptors (PPARs) regulate the expression of specific genes in lipid or glucose metabolism [85][86]. The PPARs family belongs to three isoforms of nuclear receptors (PPARα, PPARβ/δ, and PPARγ) with different locations, biological effects, and medical purposes. PPAR agonists are considered to prevent cardiomyocytes from ATP depletion and enhance mitochondrial biogenesis [87][88], important therapeutic targets in LVAD remodelling (Figure 1) .2.2.3. Mitochondria-Targeted Treatment
Mitochondrial biogenesis, structure, and function have been of special interest with wide clinical testing since their improvement is thought to ameliorate cardiac function directly [89]. The reduction in pathological ROS production is one of the therapeutic targets and is believed to restore energetic balance in cardiomyocytes. To find the optimal antioxidant, supplementation of coenzyme Q (CoQ) was proposed for chronic HF patients in NYHA classification III or IV [90]. CoQ plays a significant role in the mitochondrial electron transport chain as an electron acceptor, thereby contributing to ROS reductions. At week 106 of supplementation, the outcomes were positive and treated patients showed a significantly lower risk of cardiovascular deaths (p = 0.026) and HF hospitalization (p = 0.033) in comparison to the placebo group. These results are in line with a more recent meta-analysis, where reduced mortality and improved exercise capacity were noted in HF patients with CoQ supplementation [91]. Moreover, the CoQ with better mitochondrial bioavailability (MitoQ) was reported to restore mitochondrial respiration and membrane potential in an animal model of heart failure induced by pressure overload [92]. Another rationale for therapeutic use might be decreased endogenous synthesis of CoQ with age [93] and its efficacy in lowering proBNP and improving cardiac systolic function in an elderly population [94]. In turn, the Szeto–Schiller (SS) peptides, especially SS-31, have demonstrated protective properties to cardiolipin, maintaining electron carrying function and ROS utilization [95]. SS-31 safety and toleration have been accepted in two clinical trials, whilst a single infusion in a high dose was beneficial for LV volume [96] but, in the long-term, did not decrease myocardial infarct size [97]. Decreased content of cardiolipin and its mitochondrial decomposition was reported in the myocardium after LVAD support, suggesting that cardiolipin is a potential therapeutic target [98].
To prevent pathological heart remodelling, it is proposed to maintain the nicotinamide adenine dinucleotide (NAD+) pool and NADH (reduced form of NAD+)/NAD+ ratio [99]. An elevated ratio of NADH/NAD+ with cytosolic protein hyperacetylation, including malate–aspartate shuttle proteins and oligomycin-sensitive conferring protein in ATP synthase complex, contributed to the worsening HF in humans and in an animal model of mitochondrial complex-I deficiency. Furthermore, Lee et al. highlighted that elevating the NAD+ level might normalize redox status and improve cardiac function, predicting the high translational potential of the NAD+ precursors. In blood, nicotinamide riboside (NR) was confirmed to successfully increase the level of circulating NAD+ in healthy human voluntaries without serious side effects [100]. Therapeutic opportunities of NR were recently investigated in HF patients undergoing LVAD implantation and showed that oral administration was associated with reduced pro-inflammatory activation [101].
2.2.4. Inhibition of Inflammation
The anti-inflammatory approach originated from the strong need to counteract high mortality and morbidity, along with a better understanding of protective or harmful immune mechanisms in heart failure progression [102]. It has been reported that levels of circulating cytokines, such as interleukin (IL) 1, 2, or 6, and TNF, are increasing simultaneously with the worsening status of HF patients [103][104]. It might be caused by LV dysfunction (via hypertrophy and further fibrosis) and endothelial dysfunction (through apoptosis and reduced NO synthesis), overall contributing to myocardial failure [105]. Hence, lowering the level of proinflammatory cytokines is thought to initiate a healing response. Patients with LVAD might be at particular risk of a higher level of serum TNF-α levels compared to only HF or HTx subjects [106]. Tabit et al. suggested that elevated levels of TNF-α directly stimulate thrombin-induced angiopoietin-2 (Ang2) expression and jointly induce pathological angiogenesis, leading to angiodysplasia and increasing the risk of non-surgical bleeding. Therefore, TNF-α blockade could prevent LVAD patients from high risk of these complications. In a prior study, TNF-α inhibition failed to show improvement in symptoms and quality of life whilst increasing the risk of hospitalization for worsening heart failure [107]. In contrast, administration of pentoxifylline has improved cardiac function (LVEF increased by 32%) and reduced markers of inflammation (CRP, TNF-α) with a preserved pool of circulating TNF in ischemic cardiomyopathy [108]. It is noteworthy that TNF might improve post-ischemic functional recovery; therefore, the use of strong inhibition reduces the cardioprotective effect [109]. Anakinra is a recombinant human receptor for IL-1 and blockades successfully both isoforms (α/β) from proinflammatory signalling. Concordant with prior studies, IL-1 inhibition has effectively dealt with an inflammatory response in acute myocardial infarction [110] and LV dysfunction [111]. Moreover, lowering IL-1 levels is believed to boost cardiac function by restoring calcium handling and preventing cardiomyocytes from abnormal contractility and hypotrophy [112]. Therefore, Anakinra is also considered to be an adjuvant agent in the LVAD area. The first outcomes from the clinical trial have convincingly demonstrated therapeutic potential [113]. Healy et al. have shown not only CRP reduction (about 76%) but also a 67% increase in EF after 6 months of a short course of Anakinra (2 weeks).2.2.5. Other Strategies for Cardiac Regeneration
Restoration of SERCA2a expression is thought to prevent severe systolic and diastolic dysfunction equally to mechanical assist devices in advanced HF treatment [114]. Down-regulation of SERCA2a was observed in failing heart samples, which translated to dysregulation in Ca2+ homeostasis and impaired myocardial contractility through increased intracellular calcium concentrations [115]. Therefore, therapy based on SERCA2a gene delivery was proposed to reverse HF progression as a novel modality for treatment. A signal of potential opportunities to reduce the number and recurrence of cardiovascular events has been described following a single dose of adeno-associated virus serotype 1 (AAV1) vector carrying SERCA2a (AAV1/SERCA2a) in patients with advanced heart failure [116]. However, the combination of gene therapy with mechanical circulatory support did not show positive outcomes in the SERCA-LVAD trial due to the small cohort of patients and safety concerns [117]. In turn, istaroxime demonstrates both rapid calcium return with myocardial relaxation via SERCA2 stimulation and contractility improvement by Na+/K+-AT P-ase inhibition [118]. Therefore, it has also been clinically tested to examine the occurrence of cardiac adverse events, such as arrhythmia [119]. ]. The 24 h infusion has shown beneficial changes in echocardiography parameters, with a lack of major cardiac adverse effects in the acute HF patients’ cohort. These results are in line with the recent study by Metra et al., where the inotropic effect of istaroxime increased cardiac index with blood pressure changes and reduced left ventricular and atrial dimensions [120] Many studies highlighted the cardioprotective effect of oestrogen receptors (ER) agonists and suggested therapeutic opportunities in HF treatment [121][122]. ER activation mediates several protective pathways, including vasculature, fibrosis, energy metabolism in mitochondria, ROS production, and cardiomyocyte survival. Recently, Iorga et al. reported a decreased local heart concentration of oestradiol (E2) and cardiac aromatase transcript levels in the mice model of HF (induced by TAC). Moreover, exogenous treatment of E2 in the same male and female mice improved systolic function, stimulated cardiac angiogenesis, and suppressed fibrosis [123]. Interestingly, the cardioprotective effect of oestrogen has been demonstrated in other animal models of HF [124][125], including right ventricular failure caused by pulmonary hypertension [126]. In light of these results, hormone therapy could represent an interesting direction in HF treatment; however, the lack of knowledge and clinical practice limits its usefulness.3. Conclusions
LVAD therapy is an effective rescue in acute and especially chronic cardiac failure. In several scenarios, it provides a platform for regeneration and sustained myocardial recovery. While unloading seems to be a key element, pharmacotherapy may provide powerful tools to enhance effective cardiac regeneration. A strategy of combining LVAD with intensive pharmacotherapy has demonstrated more favour in cardiac, clinical, and survival outcomes, with a higher likelihood of myocardial recovery than any other form of HF treatment. In this context, progressively more clinical trials provide credibility to combining the benefits of LVAD therapy with novel pharmacotherapies. Considerable potential exists in stem cell therapy, regulators of substrate oxidation, treatment targeted to mitochondrial biogenesis, structure, and function, as well as inhibitors of a harmful immune response. Despite sustained progress in the engineering, experimental, and clinical fields, further investigation is needed to discover mechanisms of reverse remodelling and increase the effectiveness of the bridge to recovery strategy.References
- Kadakia, S.; Moore, R.; Ambur, V.; Toyoda, Y. Current status of the implantable LVAD. Gen. Thorac. Cardiovasc. Surg. 2016.Grupper, A.; Zhao, Y.M.; Sajgalik, P.; Joyce, L.D.; Park, S.J.; Pereira, N.L.; Stulak, J.M.; Burnett, J.C.; Edwards, B.S.; Daly, R.C.; et al. Effect of Neurohormonal Blockade Drug Therapy on Outcomes and Left Ventricular Function and Structure After Left Ventricular Assist Device Implantation. Am. J. Cardiol. 2016, 117, 1765–1770. https://doi.org/10.1016/j.amjcard.2016.03.011.
- Iii, W.K.C.; Copeland, H.; Takeda, K.; Fernandez, F.G.; Badhwar, V.; Habib, R.H.; Jacobs, J.P.; Koehl, D.; Kirklin, J.K.; Pagani, F.D.; et al. The Society of Thoracic Surgeons Intermacs 2020 Annual Report. Ann. Thorac. Surg. 2021, 111, 778–792.
- Task, A.; Members, F.; Mcdonagh, T.A.; United, C.; Gardner, R.S.; Force, T.; United, C.; Baumbach, A.; Kingdom, U.; Bo, M.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 3599–3726.
- Kirklin, J.K.; Pagani, F.D.; Kormos, R.L.; Stevenson, L.W.; Blume, E.D.; Myers, S.L.; Miller, M.A.; Baldwin, J.T.; Young, J.B.; Naftel, D.C. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J. Heart Lung Transplant. 2017, 36, 1080–1086.
- Rose, E.A.; Moskowitz, A.J.; Packer, M.; Sollano, J.A.; Williams, D.L.; Tierney, A.R.; Heitjan, D.F.; Meier, P.; Ascheim, D.D.; Levitan, R.G.; et al. The REMATCH trial: Rationale, design, and end points. Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure. Ann. Thorac. Surg. 1999, 67, 723–730.
- Birks, E.J.; Drakos, S.G.; Patel, S.R.; Lowes, B.D.; Selzman, C.H.; Starling, R.C.; Trivedi, J.; Slaughter, M.S.; Alturi, P.; Goldstein, D.; et al. Prospective Multicenter Study of Myocardial Recovery Using Left Ventricular Assist Devices (RESTAGE-HF ): Medium-Term and Primary End Point Results. Circulation 2020, 142, 2016–2028.
- Matkovich, S.J.; Van Booven, D.J.; Youker, K.A.; Torre-Amione, G.; Diwan, A.; Eschenbacher, W.H.; Dorn, L.E.; Watson, M.A.; Margulies, K.B.; Dorn, G.W. 2nd Reciprocal regulation of myocardial microRNAs and messenger RNA in human cardiomyopathy and reversal of the microRNA signature by biomechanical support. Circulation 2009, 119, 1263–1271.
- Canseco, D.C.; Kimura, W.; Garg, S.; Mukherjee, S.; Bhattacharya, S.; Abdisalaam, S.; Das, S.; Asaithamby, A.; Mammen, P.P.A.; Sadek, H.A. Human ventricular unloading induces cardiomyocyte proliferation. J. Am. Coll. Cardiol. 2015, 65, 892–900.
- Wohlschlaeger, J.; Schmitz, K.J.; Schmid, C.; Schmid, K.W.; Keul, P.; Takeda, A.; Weis, S.; Levkau, B.; Baba, H.A. Reverse remodeling following insertion of left ventricular assist devices (LVAD): A review of the morphological and molecular changes. Cardiovasc. Res. 2005, 68, 376–386.
- Manginas, A.; Tsiavou, A.; Sfyrakis, P.; Giamouzis, G. Increased Number of Circulating Progenitor Cells After Methods: Results. J. Heart Lung Transplant. 2009, 28, 710–717.
- Ivak, P.; Netuka, I.; Kralova-Lesna, I.; Wohlfahrt, P.; Pitha, J. Changes in circulating stem cells and endothelial progenitor cells over a 12-month period after implantation of a continuous-flow left ventricular assist device. Arch. Med. Sci. 2020, 16, 1440–1443.
- Farris, S.D.; Don, C.; Helterline, D.; Costa, C.; Plummer, T.; Steffes, S.; Mahr, C.; Mokadam, N.A.; Stempien-Otero, A. Cell-Specific Pathways Supporting Persistent Fibrosis in Heart Failure. J. Am. Coll. Cardiol. 2017, 70, 344–354.
- Dhar, K.; Moulton, A.M.; Rome, E.; Qiu, F.; Kittrell, J.; Raichlin, E.; Zolty, R.; Um, J.Y.; Moulton, M.J.; Basma, H.; et al. Targeted myocardial gene expression in failing hearts by RNA sequencing. J. Transl. Med. 2016, 14, 327.
- Heerdt, P.M.; Holmes, J.W.; Cai, B.; Barbone, A.; Madigan, J.D.; Reiken, S.; Lee, D.L.; Oz, M.C.; Marks, A.R.; Burkhoff, D. Chronic unloading by left ventricular assist device reverses contractile dysfunction and alters gene expression in end-stage heart failure. Circulation 2000, 102, 2713–2719.
- Diakos, N.A.; Taleb, I.; Kyriakopoulos, C.P.; Shah, K.S.; Javan, H.; Richins, T.J.; Yin, M.Y.; Yen, C.-G.; Dranow, E.; Bonios, M.J.; et al. Circulating and Myocardial Cytokines Predict Cardiac Structural and Functional Improvement in Patients With Heart Failure Undergoing Mechanical Circulatory Support. J. Am. Heart Assoc. 2021, 10, e020238.
- Torre-Amione, G.; Stetson, S.J.; Youker, K.A.; Durand, J.B.; Radovancevic, B.; Delgado, R.M.; Frazier, O.H.; Entman, M.L.; Noon, G.P. Decreased expression of tumor necrosis factor-alpha in failing human myocardium after mechanical circulatory support: A potential mechanism for cardiac recovery. Circulation 1999, 100, 1189–1193.
- Chaudhary, K.W.; Rossman, E.I.; Piacentino, V., 3rd; Kenessey, A.; Weber, C.; Gaughan, J.P.; Ojamaa, K.; Klein, I.; Bers, D.M.; Houser, S.R.; et al. Altered myocardial Ca2+ cycling after left ventricular assist device support in the failing human heart. J. Am. Coll. Cardiol. 2004, 44, 837–845.
- Terracciano, C.M.N.; Harding, S.E.; Adamson, D.; Koban, M.; Tansley, P.; Birks, E.J.; Barton, P.J.R.; Yacoub, M.H. Changes in sarcolemmal Ca entry and sarcoplasmic reticulum Ca content in ventricular myocytes from patients with end-stage heart failure following myocardial recovery after combined pharmacological and ventricular assist device therapy. Eur. Heart J. 2003, 24, 1329–1339.
- Ibrahim, M.; Navaratnarajah, M.; Siedlecka, U.; Rao, C.; Dias, P.; Moshkov, A.V.; Gorelik, J.; Yacoub, M.H.; Terracciano, C.M. Mechanical unloading reverses transverse tubule remodelling and normalizes local Ca2+-induced Ca2+ release in a rodent model of heart failure. Eur. J. Heart Fail. 2012, 14, 571–580.
- Seidel, T.; Navankasattusas, S.; Ahmad, A.; Diakos, N.A.; Xu, W.D.; Tristani-Firouzi, M.; Bonios, M.J.; Taleb, I.; Li, D.Y.; Selzman, C.H.; et al. Sheet-Like Remodeling of the Transverse Tubular System in Human Heart Failure Impairs Excitation-Contraction Coupling and Functional Recovery by Mechanical Unloading. Circulation 2017, 135, 1632–1645.
- Thohan, V.; Stetson, S.J.; Nagueh, S.F.; Rivas-Gotz, C.; Koerner, M.M.; Lafuente, J.A.; Loebe, M.; Noon, G.P.; Torre-Amione, G. Cellular and hemodynamics responses of failing myocardium to continuous flow mechanical circulatory support using the DeBakey-Noon left ventricular assist device: A comparative analysis with pulsatile-type devices. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2005, 24, 566–575.
- Müller, J.; Wallukat, G.; Weng, Y.G.; Dandel, M.; Spiegelsberger, S.; Semrau, S.; Brandes, K.; Theodoridis, V.; Loebe, M.; Meyer, R.; et al. Weaning from mechanical cardiac support in patients with idiopathic dilated cardiomyopathy. Circulation 1997, 96, 542–549.
- Li, Y.Y.; Feng, Y.; McTiernan, C.F.; Pei, W.; Moravec, C.S.; Wang, P.; Rosenblum, W.; Kormos, R.L.; Feldman, A.M. Downregulation of matrix metalloproteinases and reduction in collagen damage in the failing human heart after support with left ventricular assist devices. Circulation 2001, 104, 1147–1152.
- Klotz, S.; Foronjy, R.F.; Dickstein, M.L.; Gu, A.; Garrelds, I.M.; Danser, A.H.J.; Oz, M.C.; D’Armiento, J.; Burkhoff, D. Mechanical unloading during left ventricular assist device support increases left ventricular collagen cross-linking and myocardial stiffness. Circulation 2005, 112, 364–374.
- Miyagawa, S.; Toda, K.; Nakamura, T.; Yoshikawa, Y.; Fukushima, S.; Saito, S.; Yoshioka, D.; Saito, T.; Sawa, Y. Building a bridge to recovery: The pathophysiology of LVAD-induced reverse modeling in heart failure. Surg. Today 2016, 46, 149–154.
- Diakos, N.A.; Navankasattusas, S.; Abel, E.D.; Rutter, J.; McCreath, L.; Ferrin, P.; McKellar, S.H.; Miller, D.V.; Park, S.Y.; Richardson, R.S.; et al. Evidence of Glycolysis Up-Regulation and Pyruvate Mitochondrial Oxidation Mismatch During Mechanical Unloading of the Failing Human Heart: Implications for Cardiac Reloading and Conditioning. JACC. Basic to Transl. Sci. 2016, 1, 432–444.
- Badolia, R.; Ramadurai, D.K.A.; Abel, E.D.; Ferrin, P.; Taleb, I.; Shankar, T.S.; Krokidi, A.T.; Navankasattusas, S.; McKellar, S.H.; Yin, M.; et al. The Role of Nonglycolytic Glucose Metabolism in Myocardial Recovery Upon Mechanical Unloading and Circulatory Support in Chronic Heart Failure. Circulation 2020, 142, 259–274. https://doi.org/10.1161/CIRCULATIONAHA.119.044452.
- Cluntun, A.A.; Badolia, R.; Lettlova, S.; Mckellar, S.H.; Rutter, J.; Drakos, S.G. Article The pyruvate-lactate axis modulates cardiac hypertrophy and heart failure Article The pyruvate-lactate axis modulates cardiac hypertrophy and heart failure. Cell Metab. 2021, 1–20. https://doi.org/10.1016/j.cmet.2020.12.003.
- Aissaoui, N.; Jouan, J.; Gourjault, M.; Diebold, B.; Ortuno, S.; Hamdan, A.; Latremouille, C.; Pirracchio, R.; Morshuis, M. Understanding left ventricular assist devices. Blood Purif. 2018, 46, 292–300.Badolia, R.; Ramadurai, D.K.A.; Abel, E.D.; Ferrin, P.; Taleb, I.; Shankar, T.S.; Krokidi, A.T.; Navankasattusas, S.; McKellar,
- Zimpfer, D.; Strueber, M.; Aigner, P.; Schmitto, J.D.; Fiane, A.E.; Larbalestier, R.; Tsui, S.; Jansz, P.; Simon, A.; Schueler, S.; et al. Evaluation of the HeartWare ventricular assist device Lavare cycle in a particle image velocimetry model and in clinical practice. Eur. J. Cardio-Thoracic Surg. Off. J. Eur. Assoc. Cardio-Thoracic Surg. 2016, 50, 839–848.S.H.; Yin, M.; et al. The Role of Nonglycolytic Glucose Metabolism in Myocardial Recovery Upon Mechanical Unloading and
- Mariani, S.; Hanke, J.S.; Dogan, G.; Schmitto, J.D. Out of hospital management of LVAD patients during COVID-19 outbreak. Artif. Organs 2020, 44, 873–876.Circulatory Support in Chronic Heart Failure. Circulation 2020, 142, 259–274
- Maybaum, S.; Mancini, D.; Xydas, S.; Starling, R.C.; Aaronson, K.; Pagani, F.D.; Miller, L.W.; Margulies, K.; McRee, S.; Frazier, O.H.; et al. Cardiac improvement during mechanical circulatory support: A prospective multicenter study of the LVAD working group. Circulation 2007, 115, 2497–2505. Aissaoui, N.; Jouan, J.; Gourjault, M.; Diebold, B.; Ortuno, S.; Hamdan, A.; Latremouille, C.; Pirracchio, R.; Morshuis, M. Understanding left ventricular assist devices. Blood Purif. 2018, 46, 292–300.
- Antonides, C.F.J.; Schoenrath, F.; De By, T.M.M.H.; Muslem, R.; Yalcin, Y.C.; Netuka, I.; Gummert, J.; Potapov, E.V.; Meyns, B.; Özbaran, M.; et al. Outcomes of patients after successful left ventricular assist device explantation: A EUROMACS study. ESC Heart Fail. 2020.Zimpfer, D.; Strueber, M.; Aigner, P.; Schmitto, J.D.; Fiane, A.E.; Larbalestier, R.; Tsui, S.; Jansz, P.; Simon, A.; Schueler, S.; et al. Evaluation of the HeartWare ventricular assist device Lavare cycle in a particle image velocimetry model and in clinical practice. Eur. J. Cardio-Thoracic Surg. Off. J. Eur. Assoc. Cardio-Thoracic Surg. 2016, 50, 839–848.
- Yacoub, M.H. A novel strategy to maximize the efficacy of left ventricular assist devices as a bridge to recovery. Eur. Heart J. 2001, 22, 534–540.Mariani, S.; Hanke, J.S.; Dogan, G.; Schmitto, J.D. Out of hospital management of LVAD patients during COVID-19 outbreak. Artif. Organs 2020, 44, 873–876.
- Hon, J.K.F.; Yacoub, M.H. Bridge to recovery with the use of left ventricular assist device and clenbuterol. Ann. Thorac. Surg. 2003, 75, S36–S41.Maybaum, S.; Mancini, D.; Xydas, S.; Starling, R.C.; Aaronson, K.; Pagani, F.D.; Miller, L.W.; Margulies, K.; McRee, S.; Frazier, O.H.; et al. Cardiac improvement during mechanical circulatory support: A prospective multicenter study of the LVAD working group. Circulation 2007, 115, 2497–2505.
- Bowles, C.T.; Ph, D.; Burke, M.; Path, F.R.C.; Banner, N.R.; Khaghani, A. Left Ventricular Assist Device and Drug Therapy for the Reversal of Heart Failure. N. Engl. J. Med. 2006, 1873–1884.Antonides, C.F.J.; Schoenrath, F.; De By, T.M.M.H.; Muslem, R.; Yalcin, Y.C.; Netuka, I.; Gummert, J.; Potapov, E.V.; Meyns, B.; Özbaran, M.; et al. Outcomes of patients after successful left ventricular assist device explantation: A EUROMACS study. ESC Heart Fail. 2020.
- Groenning, B.A.; Nilsson, J.C.; Sondergaard, L.; Fritz-hansen, T.; Larsson, H.B.W.; Dms, C.; Hildebrandt, P.R.; Dms, C. Antiremodeling Effects on the Left Ventricle During Beta-BlockadeWith Metoprolol in the Treatment of Chronic Heart Failure. Clin. Trial 2000, 36, 2072–2080.Yacoub, M.H. A novel strategy to maximize the efficacy of left ventricular assist devices as a bridge to recovery. Eur. Heart J. 2001, 22, 534–540.
- Greenberg, B.; Quinones, M.A.; Koilpillai, C.; Limacher, M.; Shindler, D.; Benedict, C.; Shelton, B. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation 1995, 91, 2573–2581.Hon, J.K.F.; Yacoub, M.H. Bridge to recovery with the use of left ventricular assist device and clenbuterol. Ann. Thorac. Surg. 2003, 75, S36–S41.
- Wong, M.; Staszewsky, L.; Latini, R.; Barlera, S.; Volpi, A.; Chiang, Y.; Benza, R.L.; Gottlieb, S.O.; Kleemann, T.D.; Rosconi, F.; et al. Valsartan Benefits Left Ventricular Structure and Function in Heart Failure: Val-HeFT Echocardiographic Study. Clin. Trial 2002, 40, 970–975.Bowles, C.T.; Ph, D.; Burke, M.; Path, F.R.C.; Banner, N.R.; Khaghani, A. Left Ventricular Assist Device and Drug Therapy for the Reversal of Heart Failure. N. Engl. J. Med. 2006, 1873–1884.
- Mancini, D.M.; Beniaminovitz, A.; Levin, H.; Catanese, K.; Flannery, M.; DiTullio, M.; Savin, S.; Cordisco, M.E.; Rose, E.; Oz, M. Low incidence of myocardial recovery after left ventricular assist device implantation in patients with chronic heart failure. Circulation 1998, 98, 2383–2389.Groenning, B.A.; Nilsson, J.C.; Sondergaard, L.; Fritz-hansen, T.; Larsson, H.B.W.; Dms, C.; Hildebrandt, P.R.; Dms, C. Antiremodeling Effects on the Left Ventricle During Beta-Blockade With Metoprolol in the Treatment of Chronic Heart Failure. Clin. Trial 2000, 36, 2072–2080.
- Farrar, D.J.; Holman, W.R.; McBride, L.R.; Kormos, R.L.; Icenogle, T.B.; Hendry, P.J.; Moore, C.H.; Loisance, D.Y.; El-Banayosy, A.; Frazier, H. Long-term follow-up of Thoratec ventricular assist device bridge-to-recovery patients successfully removed from support after recovery of ventricular function. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2002, 21, 516–521.Greenberg, B.; Quinones, M.A.; Koilpillai, C.; Limacher, M.; Shindler, D.; Benedict, C.; Shelton, B. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation 1995, 91, 2573–2581.
- Birks, E.J.; George, R.S.; Hedger, M.; Bahrami, T.; Wilton, P.; Bowles, C.T.; Webb, C.; Bougard, R.; Amrani, M.; Yacoub, M.H.; et al. Reversal of severe heart failure with a continuous-flow left ventricular assist device and pharmacological therapy: A prospective study. Circulation 2011, 123, 381–390.Wong, M.; Staszewsky, L.; Latini, R.; Barlera, S.; Volpi, A.; Chiang, Y.; Benza, R.L.; Gottlieb, S.O.; Kleemann, T.D.; Rosconi, F.; et al. Valsartan Benefits Left Ventricular Structure and Function in Heart Failure: Val-HeFT Echocardiographic Study. Clin. Trial 2002, 40, 970–975.
- Grupper, A.; Zhao, Y.M.; Sajgalik, P.; Joyce, L.D.; Park, S.J.; Pereira, N.L.; Stulak, J.M.; Burnett, J.C.; Edwards, B.S.; Daly, R.C.; et al. Effect of Neurohormonal Blockade Drug Therapy on Outcomes and Left Ventricular Function and Structure After Left Ventricular Assist Device Implantation. Am. J. Cardiol. 2016, 117, 1765–1770.Mancini, D.M.; Beniaminovitz, A.; Levin, H.; Catanese, K.; Flannery, M.; DiTullio, M.; Savin, S.; Cordisco, M.E.; Rose, E.; Oz, M. Low incidence of myocardial recovery after left ventricular assist device implantation in patients with chronic heart failure. Circulation 1998, 98, 2383–2389.
- Haider, L.; Hugon-Vallet, E.; Constantin, J.P.; Riad, Z.; Sebbag, L.; Mewton, N. ARNI Pre-Operative Use and Vasoplegic Syndrome in Patients Undergoing Heart Transplantation or Left Ventricular Assist Device Surgery. Med. Sci. 2021, 10, 2.Farrar, D.J.; Holman, W.R.; McBride, L.R.; Kormos, R.L.; Icenogle, T.B.; Hendry, P.J.; Moore, C.H.; Loisance, D.Y.; El-Banayosy, A.; Frazier, H. Long-term follow-up of Thoratec ventricular assist device bridge-to-recovery patients successfully removed from support after recovery of ventricular function. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2002, 21, 516–521.
- Velazquez, E.J.; Morrow, D.A.; DeVore, A.D.; Duffy, C.I.; Ambrosy, A.P.; McCague, K.; Rocha, R.; Braunwald, E. Angiotensin- Neprilysin Inhibition in Acute Decompensated Heart Failure. N. Engl. J. Med. 2019, 380, 539–548.Birks, E.J.; George, R.S.; Hedger, M.; Bahrami, T.; Wilton, P.; Bowles, C.T.; Webb, C.; Bougard, R.; Amrani, M.; Yacoub, M.H.; et al. Reversal of severe heart failure with a continuous-flow left ventricular assist device and pharmacological therapy: A prospective study. Circulation 2011, 123, 381–390.
- Navaratnarajah, M.; Ibrahim, M.; Siedlecka, U.; van Doorn, C.; Shah, A.; Gandhi, A.; Dias, P.; Sarathchandra, P.; Yacoub, M.H.; Terracciano, C.M. Influence of ivabradine on reverse remodelling during mechanical unloading. Cardiovasc. Res. 2013, 97, 230–239.Grupper, A.; Zhao, Y.M.; Sajgalik, P.; Joyce, L.D.; Park, S.J.; Pereira, N.L.; Stulak, J.M.; Burnett, J.C.; Edwards, B.S.; Daly, R.C.; et al. Effect of Neurohormonal Blockade Drug Therapy on Outcomes and Left Ventricular Function and Structure After Left Ventricular Assist Device Implantation. Am. J. Cardiol. 2016, 117, 1765–1770. https://doi.org/10.1016/j.amjcard.2016.03.011.
- Fang, Y.; Debunne, M.; Vercauteren, M.; Brakenhielm, E.; Richard, V.; Lallemand, F.; Henry, J.P.; Mulder, P.; Thuillez, C. Heart rate reduction induced by the if current inhibitor ivabradine improves diastolic function and attenuates cardiac tissue hypoxia. J. Cardiovasc. Pharmacol. 2012, 59, 260–267Haider, L.; Hugon-Vallet, E.; Constantin, J.P.; Riad, Z.; Sebbag, L.; Mewton, N. ARNI Pre-Operative Use and Vasoplegic Syndrome in Patients Undergoing Heart Transplantation or Left Ventricular Assist Device Surgery. Med. Sci. 2021, 10, 2.
- Maczewski, M.; Mackiewicz, U. Effect of metoprolol and ivabradine on left ventricular remodelling and Ca2+ handling in the post-infarction rat heart. Cardiovasc. Res. 2008, 79, 42–51. Velazquez, E.J.; Morrow, D.A.; DeVore, A.D.; Duffy, C.I.; Ambrosy, A.P.; McCague, K.; Rocha, R.; Braunwald, E. Angiotensin-Neprilysin Inhibition in Acute Decompensated Heart Failure. N. Engl. J. Med. 2019, 380, 539–548.
- Margulies, K.B.; Matiwala, S.; Cornejo, C.; Olsen, H.; Craven, W.A.; Bednarik, D. Mixed messages: Transcription patterns in failing and recovering human myocardium. Circ. Res. 2005, 96, 592–599.Navaratnarajah, M.; Ibrahim, M.; Siedlecka, U.; van Doorn, C.; Shah, A.; Gandhi, A.; Dias, P.; Sarathchandra, P.; Yacoub, M.H.; Terracciano, C.M. Influence of ivabradine on reverse remodelling during mechanical unloading. Cardiovasc. Res. 2013, 97, 230–239.
- Ambardekar, A.V.; Dorosz, J.L.; Cleveland, J.C.; Lindenfeld, J.; Buttrick, P.M. Longitudinal left ventricular structural and functional imaging during full support with continuous-flow ventricular assist devices: A retrospective, preliminary analysis. J. Heart Lung Transplant. 2012, 31, 1311–1313Fang, Y.; Debunne, M.; Vercauteren, M.; Brakenhielm, E.; Richard, V.; Lallemand, F.; Henry, J.P.; Mulder, P.; Thuillez, C. Heart rate reduction induced by the if current inhibitor ivabradine improves diastolic function and attenuates cardiac tissue hypoxia. J. Cardiovasc. Pharmacol. 2012, 59, 260–267.
- Drakos, S.G.; Kfoury, A.G.; Hammond, E.H.; Reid, B.B.; Revelo, M.P.; Rasmusson, B.Y.; Whitehead, K.J.; Salama, M.E.; Selzman, C.H.; Stehlik, J.; et al. Impact of mechanical unloading on microvasculature and associated central remodeling features of the failing human heart. J. Am. Coll. Cardiol. 2010, 56, 382–391.Ma̧czewski, M.; Mackiewicz, U. Effect of metoprolol and ivabradine on left ventricular remodelling and Ca2+ handling in the post-infarction rat heart. Cardiovasc. Res. 2008, 79, 42–51.
- Tran, H.A.; Silva Enciso, J.; Adler, E.D. Often talked about, seldom seen: Promoting myocardial recovery with ventricular assist device. J. Am. Coll. Cardiol. 2014, 64, 1613–1614.Margulies, K.B.; Matiwala, S.; Cornejo, C.; Olsen, H.; Craven, W.A.; Bednarik, D. Mixed messages: Transcription patterns in failing and recovering human myocardium. Circ. Res. 2005, 96, 592–599.
- Michler, R.E. The current status of stem cell therapy in ischemic heart disease. J. Card. Surg. 2018, 33, 520–531.Ambardekar, A.V.; Dorosz, J.L.; Cleveland, J.C.; Lindenfeld, J.; Buttrick, P.M. Longitudinal left ventricular structural and functional imaging during full support with continuous-flow ventricular assist devices: A retrospective, preliminary analysis. J. Heart Lung Transplant. 2012, 31, 1311–1313.
- Liu, C.-B.; Huang, H.; Sun, P.; Ma, S.-Z.; Liu, A.-H.; Xue, J.; Fu, J.-H.; Liang, Y.-Q.; Liu, B.; Wu, D.-Y.; et al. Human UmbilicalCord-Derived Mesenchymal Stromal Cells Improve Left Ventricular Function, Perfusion, and Remodeling in a Porcine Model of Chronic Myocardial Ischemia. Stem Cells Transl. Med. 2016, 5, 1004–1013.Drakos, S.G.; Kfoury, A.G.; Hammond, E.H.; Reid, B.B.; Revelo, M.P.; Rasmusson, B.Y.; Whitehead, K.J.; Salama, M.E.; Selzman, C.H.; Stehlik, J.; et al. Impact of mechanical unloading on microvasculature and associated central remodeling features of the failing human heart. J. Am. Coll. Cardiol. 2010, 56, 382–391.
- Evers, K.S.; Dawoud, F.; George, R.T.; Lima, J.A.C.; Lardo, A.C. CT for Evaluation of Myocardial Cell Therapy in Heart Failure. JCMG 2011, 4, 1284–1293.Tran, H.A.; Silva Enciso, J.; Adler, E.D. Often talked about, seldom seen: Promoting myocardial recovery with ventricular assist device. J. Am. Coll. Cardiol. 2014, 64, 1613–1614.
- Schuleri, K.H.; Amado, L.C.; Boyle, A.J.; Centola, M.; Saliaris, A.P.; Gutman, M.R.; Hatzistergos, K.E.; Oskouei, B.N.; Zimmet, J.M.; Young, R.G.; et al. Early improvement in cardiac tissue perfusion due to mesenchymal stem cells. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, H2002-11.Michler, R.E. The current status of stem cell therapy in ischemic heart disease. J. Card. Surg. 2018, 33, 520–531.
- Bartolucci, J.; Verdugo, F.J.; González, P.L.; Larrea, R.E.; Abarzua, E.; Goset, C.; Rojo, P.; Palma, I.; Lamich, R.; Pedreros, P.A.; et al. Safety and Efficacy of the Intravenous Infusion of Umbilical Cord Mesenchymal Stem Cells in PatientsWith Heart Failure: A Phase 1/2 Randomized Controlled Trial (RIMECARD Trial [Randomized Clinical Trial of Intravenous Infusion Umbilical Cord Mesenchymal. Circ. Res. 2017, 121, 1192–1204.Martens, T.P.; See, F.; Schuster, M.D.; Sondermeijer, H.P.; Hefti, M.M.; Zannettino, A.; Gronthos, S.; Seki, T.; Itescu, S. Mesenchymal lineage precursor cells induce vascular network formation in ischemic myocardium. Nat. Clin. Pract. Cardiovasc. Med. 2006, 3 (Suppl. 1), S18-22.
- Lunde, K.; Solheim, S.; Aakhus, S.; Arnesen, H.; Abdelnoor, M.; Egeland, T.; Endresen, K.; Ilebekk, A.; Mangschau, A.; Fjeld, J.G.; et al. Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N. Engl. J. Med. 2006, 355, 1199–1209.Dooley, L.M.; Abdalmula, A.; Washington, E.A.; Kaufman, C.; Tudor, E.M.; Ghosh, P.; Itescu, S.; Kimpton, W.G.; Bailey, S.R. Effect of mesenchymal precursor cells on the systemic inflammatory response and endothelial dysfunction in an ovine model of collagen-induced arthritis. PLoS ONE 2015, 10, e0124144.
- Stempien-Otero, A.; Helterline, D.; Plummer, T.; Farris, S.; Prouse, A.; Polissar, N.; Stanford, D.; Mokadam, N.A. Mechanisms of bone marrow-derived cell therapy in ischemic cardiomyopathy with left ventricular assist device bridge to transplant. J. Am. Coll. Cardiol. 2015, 65, 1424–1434. Borow, K.M.; Yaroshinsky, A.; Greenberg, B.; Perin, E.C. Phase 3 DREAM-HF Trial of Mesenchymal Precursor Cells in Chronic Heart Failure. Circ. Res. 2019, 125, 265–281.
- Yau, T.M.; Pagani, F.D.; Mancini, D.M.; Chang, H.L.; Lala, A.; Woo, Y.J.; Acker, M.A.; Selzman, C.H.; Soltesz, E.G.; Kern, J.A.; et al. Intramyocardial Injection of Mesenchymal Precursor Cells and Successful Temporary Weaning From Left Ventricular Assist Device Support in PatientsWith Advanced Heart Failure: A Randomized Clinical Trial. JAMA 2019, 321, 1176–1186.Bartolucci, J.; Verdugo, F.J.; González, P.L.; Larrea, R.E.; Abarzua, E.; Goset, C.; Rojo, P.; Palma, I.; Lamich, R.; Pedreros, P.A.; et al. Safety and Efficacy of the Intravenous Infusion of Umbilical Cord Mesenchymal Stem Cells in Patients With Heart Failure: A Phase 1/2 Randomized Controlled Trial (RIMECARD Trial
- Ascheim, D.D.; Gelijns, A.C.; Goldstein, D.;Moye, L.A.; Smedira, N.; Lee, S.; Klodell, C.T.; Szady, A.; Parides,M.K.; Jeffries, N.O.; et al. Mesenchymal precursor cells as adjunctive therapy in recipients of contemporary left ventricular assist devices. Circulation 2014, 129, 2287–2296.Lunde, K.; Solheim, S.; Aakhus, S.; Arnesen, H.; Abdelnoor, M.; Egeland, T.; Endresen, K.; Ilebekk, A.; Mangschau, A.; Fjeld, J.G.; et al. Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N. Engl. J. Med. 2006, 355, 1199–1209.
- Doenst, T.; Nguyen, T.D.; Abel, E.D. Cardiac metabolism in heart failure: Implications beyond ATP production. Circ. Res. 2013, 113, 709–724.Stempien-Otero, A.; Helterline, D.; Plummer, T.; Farris, S.; Prouse, A.; Polissar, N.; Stanford, D.; Mokadam, N.A. Mechanisms of bone marrow-derived cell therapy in ischemic cardiomyopathy with left ventricular assist device bridge to transplant. J. Am. Coll. Cardiol. 2015, 65, 1424–1434.
- Bertero, E.; Maack, C. Metabolic remodelling in heart failure. Nat. Rev. Cardiol. 2018, 15, 457–470.Yau, T.M.; Pagani, F.D.; Mancini, D.M.; Chang, H.L.; Lala, A.; Woo, Y.J.; Acker, M.A.; Selzman, C.H.; Soltesz, E.G.; Kern, J.A.; et al. Intramyocardial Injection of Mesenchymal Precursor Cells and Successful Temporary Weaning From Left Ventricular Assist Device Support in Patients With Advanced Heart Failure: A Randomized Clinical Trial. JAMA 2019, 321, 1176–1186.
- Zhou, B.; Tian, R. Mitochondrial dysfunction in pathophysiology of heart failure. J. Clin. Investig. 2018, 128, 3716–3726.Ascheim, D.D.; Gelijns, A.C.; Goldstein, D.; Moye, L.A.; Smedira, N.; Lee, S.; Klodell, C.T.; Szady, A.; Parides, M.K.; Jeffries, N.O.; et al. Mesenchymal precursor cells as adjunctive therapy in recipients of contemporary left ventricular assist devices. Circulation 2014, 129, 2287–2296.
- Huss, J.M.; Kelly, D.P. Mitochondrial energy metabolism in heart failure: A question of balance. J. Clin. Investig. 2005, 115, 547–555.Doenst, T.; Nguyen, T.D.; Abel, E.D. Cardiac metabolism in heart failure: Implications beyond ATP production. Circ. Res. 2013, 113, 709–724.
- Grynberg, A.; Demaison, L. Fatty acid oxidation in the heart. J. Cardiovasc. Pharmacol. 1996, 28 (Suppl. 1), S11-7.Bertero, E.; Maack, C. Metabolic remodelling in heart failure. Nat. Rev. Cardiol. 2018, 15, 457–470.
- Dodd, M.S.; Ball, D.R.; Schroeder, M.A.; Le Page, L.M.; Atherton, H.J.; Heather, L.C.; Seymour, A.-M.; Ashrafian, H.; Watkins, H.; Clarke, K.; et al. In vivo alterations in cardiac metabolism and function in the spontaneously hypertensive rat heart. Cardiovasc. Res. 2012, 95, 69–76.Zhou, B.; Tian, R. Mitochondrial dysfunction in pathophysiology of heart failure. J. Clin. Investig. 2018, 128, 3716–3726.
- Osorio, J.C.; Stanley, W.C.; Linke, A.; Castellari, M.; Diep, Q.N.; Panchal, A.R.; Hintze, T.H.; Lopaschuk, G.D.; Recchia, F.A. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. Circulation 2002, 106, 606–612.Huss, J.M.; Kelly, D.P. Mitochondrial energy metabolism in heart failure: A question of balance. J. Clin. Investig. 2005, 115, 547–555.
- Neubauer, S. The Failing Heart—An Engine Out of Fuel. N. Engl. J. Med. 2007, 356, 1140–1151.Grynberg, A.; Demaison, L. Fatty acid oxidation in the heart. J. Cardiovasc. Pharmacol. 1996, 28 (Suppl. 1), S11-7.
- Lenneman, A.J.; Birks, E.J. Treatment strategies for myocardial recovery in heart failure. Curr. Treat. Options Cardiovasc. Med. 2014, 16, 287.Dodd, M.S.; Ball, D.R.; Schroeder, M.A.; Le Page, L.M.; Atherton, H.J.; Heather, L.C.; Seymour, A.-M.; Ashrafian, H.; Watkins, H.; Clarke, K.; et al. In vivo alterations in cardiac metabolism and function in the spontaneously hypertensive rat heart. Cardiovasc. Res. 2012, 95, 69–76.
- Ashrafian, H.; Horowitz, J.D.; Frenneaux, M.P. Perhexiline. Cardiovasc. Drug Rev. 2007, 25, 76–97.Osorio, J.C.; Stanley, W.C.; Linke, A.; Castellari, M.; Diep, Q.N.; Panchal, A.R.; Hintze, T.H.; Lopaschuk, G.D.; Recchia, F.A. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. Circulation 2002, 106, 606–612.
- Cho, Y.W.; Belej, M.; Aviado, D.M. Pharmacology of a new antianginal drug: Perhexiline. I. Coronary circulation and myocardial metabolism. Chest 1970, 58, 577–581. Neubauer, S. The Failing Heart—An Engine Out of Fuel. N. Engl. J. Med. 2007, 356, 1140–1151.
- Hudak,W.J.; Lewis, R.E.; Kuhn,W.L. Cardiovascular pharmacology of perhexiline. J. Pharmacol. Exp. Ther. 1970, 173, 371–382.Lenneman, A.J.; Birks, E.J. Treatment strategies for myocardial recovery in heart failure. Curr. Treat. Options Cardiovasc. Med. 2014, 16, 287.
- Cappola, T.P. Perhexiline: Lessons for heart failure therapeutics. JACC Heart Fail. 2015, 3, 212–213. Ashrafian, H.; Horowitz, J.D.; Frenneaux, M.P. Perhexiline. Cardiovasc. Drug Rev. 2007, 25, 76–97.
- Beadle, R.M.;Williams, L.K.; Kuehl, M.; Bowater, S.; Abozguia, K.; Leyva, F.; Yousef, Z.;Wagenmakers, A.J.M.; Thies, F.; Horowitz, J.; et al. Improvement in cardiac energetics by perhexiline in heart failure due to dilated cardiomyopathy. JACC Heart Fail. 2015, 3, 202–211.Cho, Y.W.; Belej, M.; Aviado, D.M. Pharmacology of a new antianginal drug: Perhexiline. I. Coronary circulation and myocardial metabolism. Chest 1970, 58, 577–581.
- Shu, H.; Peng, Y.; Hang, W.; Zhou, N.; Wang, D.W. Trimetazidine in Heart Failure. Front. Pharmacol. 2020, 11, 569132.Hudak, W.J.; Lewis, R.E.; Kuhn, W.L. Cardiovascular pharmacology of perhexiline. J. Pharmacol. Exp. Ther. 1970, 173, 371–382.
- Ruixing, Y.; Wenwu, L.; Al-Ghazali, R. Trimetazidine inhibits cardiomyocyte apoptosis in a rabbit model of ischemia-reperfusion. Transl. Res. 2007, 149, 152–160.Cappola, T.P. Perhexiline: Lessons for heart failure therapeutics. JACC Heart Fail. 2015, 3, 212–213.
- Zhang, J.; He, X.; Bai, X.; Sun, Y.; Jiang, P.; Wang, X.; Li, W.; Zhang, Y. Protective effect of trimetazidine in radiation-induced cardiac fibrosis in mice. J. Radiat. Res. 2020, 61, 657–665.Beadle, R.M.; Williams, L.K.; Kuehl, M.; Bowater, S.; Abozguia, K.; Leyva, F.; Yousef, Z.; Wagenmakers, A.J.M.; Thies, F.; Horowitz, J.; et al. Improvement in cardiac energetics by perhexiline in heart failure due to dilated cardiomyopathy. JACC Heart Fail. 2015, 3, 202–211.
- Liu, Y.-C.; Li, L.; Su, Q.; Liu, T.; Tang, Z. Trimetazidine pretreatment inhibits myocardial apoptosis and improves cardiac function in a Swine model of coronary microembolization. Cardiology 2015, 130, 130–136.Shu, H.; Peng, Y.; Hang, W.; Zhou, N.; Wang, D.W. Trimetazidine in Heart Failure. Front. Pharmacol. 2020, 11, 569132.
- Tuunanen, H.; Engblom, E.; Naum, A.; Någren, K.; Scheinin, M.; Hesse, B.; Juhani Airaksinen, K.E.; Nuutila, P.; Iozzo, P.; Ukkonen, H.; et al. Trimetazidine, a metabolic modulator, has cardiac and extracardiac benefits in idiopathic dilated cardiomyopathy. Circulation 2008, 118, 1250–1258.Ruixing, Y.; Wenwu, L.; Al-Ghazali, R. Trimetazidine inhibits cardiomyocyte apoptosis in a rabbit model of ischemia-reperfusion. Transl. Res. 2007, 149, 152–160.
- Fragasso, G.; Palloshi, A.; Puccetti, P.; Silipigni, C.; Rossodivita, A.; Pala, M.; Calori, G.; Alfieri, O.; Margonato, A. A randomized clinical trial of trimetazidine, a partial free fatty acid oxidation inhibitor, in patients with heart failure. J. Am. Coll. Cardiol. 2006, 48, 992–998. https://doi.org/10.1016/j.jacc.2006.03.060.
- Zannad, F.; Ferreira, J.P.; Pocock, S.J.; Anker, S.D.; Butler, J.; Filippatos, G.; Brueckmann, M.; Ofstad, A.P.; Pfarr, E.; Jamal, W.; et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction : A meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet 2020, 6736, 1–11. https://doi.org/10.1016/S0140-6736(20)31824-9.
- Petrie, M.C.; Verma, S.; Docherty, K.F.; Inzucchi, S.E.; Anand, I.; Belohlávek, J.; Böhm, M.; Chiang, C.-E.; Chopra, V.K.; de Boer, R.A.; et al. Effect of Dapagliflozin on Worsening Heart Failure and Cardiovascular Death in Patients With Heart Failure With and Without Diabetes. JAMA 2020, 323, 1353–1368. https://doi.org/10.1001/jama.2020.1906.
- Trial, E.O.; Inzucchi, S.E.; Zinman, B.; Fitchett, D.; Wanner, C.; Ferrannini, E.; Schumacher, M.; Schmoor, C.; Ohneberg, K.; Johansen, O.E.; et al. How Does Empagliflozin Reduce Cardiovascular Mortality ? Insights From a Mediation Analysis of the EMPA-REG OUTCOME Trial. Randomized Control. Trial 2018, 41, 356–363. https://doi.org/10.2337/dc17-1096.
- Kim, N.H.; Kim, S.G. Fibrates Revisited: Potential Role in Cardiovascular Risk Reduction. Diabetes Metab. J. 2020, 44, 213–221.Tuunanen, H.; Engblom, E.; Naum, A.; Någren, K.; Scheinin, M.; Hesse, B.; Juhani Airaksinen, K.E.; Nuutila, P.; Iozzo, P.; Ukkonen, H.; et al. Trimetazidine, a metabolic modulator, has cardiac and extracardiac benefits in idiopathic dilated cardiomyopathy. Circulation 2008, 118, 1250–1258. https://doi.org/10.1161/CIRCULATIONAHA.108.778019.
- Okopie´ n, B.; Bułdak, Ł.; Bołdys, A. Expert Review of Clinical Pharmacology Benefits and risks of the treatment with fibrates—A comprehensive summary. Expert Rev. Clin. Pharmacol. 2018, 11, 1099–1112.Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128.
- Khuchua, Z.; Glukhov, A.I.; Strauss, A.W.; Javadov, S. Elucidating the beneficial role of ppar agonists in cardiac diseases. Int. J. Mol. Sci. 2018, 19, 1–17. https://doi.org/10.3390/ijms19113464.
- Montaigne, D.; Butruille, L.; Staels, B. PPAR control of metabolism and cardiovascular functions. Nat. Rev. Cardiol. 2021, 18, 809–823. https://doi.org/10.1038/s41569-021-00569-6.
- Javadov, S.; Kuznetsov, A.V. Mitochondria: The cell powerhouse and nexus of stress. Front. Physiol. 2013, 4, 207.Han, L.; Shen, W.J.; Bittner, S.; Kraemer, F.B.; Azhar, S. PPARs: Regulators of metabolism and as therapeutic targets in cardiovascular disease. Part II: PPAR-β/δ and PPAR-γ. Future Cardiol. 2017, 13, 279–296.
- Mortensen, S.A.; Rosenfeldt, F.; Kumar, A.; Dolliner, P.; Filipiak, K.J.; Pella, D.; Alehagen, U.; Steurer, G.; Littarru, G.P. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: Results from Q-SYMBIO: A randomized double-blind trial. JACC. Heart Fail. 2014, 2, 641–649.Koh, J.-H.; Hancock, C.R.; Terada, S.; Higashida, K.; Holloszy, J.O.; Han, D.-H. PPARβ Is Essential for Maintaining Normal Levels of PGC-1α and Mitochondria and for the Increase in Muscle Mitochondria Induced by Exercise. Cell Metab. 2017, 25, 1176–1185.e5.
- Lei, L.; Liu, Y. Efficacy of coenzyme Q10 in patients with cardiac failure: A meta-analysis of clinical trials. BMC Cardiovasc. Disord. 2017, 17, 196.Chandra, M.; Miriyala, S.; Panchatcharam, M. PPAR γ and Its Role in Cardiovascular Diseases. PPAR Res. 2017, 2017, 6404638.
- Ribeiro Junior, R.F.; Dabkowski, E.R.; Shekar, K.C.O.; Connell, K.A.; Hecker, P.A.; Murphy, M.P. MitoQ improves mitochondrial dysfunction in heart failure induced by pressure overload. Free Radic. Biol. Med. 2018, 117, 18–29.Javadov, S.; Kuznetsov, A.V. Mitochondria: The cell powerhouse and nexus of stress. Front. Physiol. 2013, 4, 207.
- Kalén, A.; Appelkvist, E.L.; Dallner, G. Age-related changes in the lipid compositions of rat and human tissues. Lipids 1989, 24, 579–584.Mortensen, S.A.; Rosenfeldt, F.; Kumar, A.; Dolliner, P.; Filipiak, K.J.; Pella, D.; Alehagen, U.; Steurer, G.; Littarru, G.P. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: Results from Q-SYMBIO: A randomized double-blind trial. JACC. Heart Fail. 2014, 2, 641–649.
- Alehagen, U.; Johansson, P.; Björnstedt, M.; Rosén, A.; Dahlström, U. Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: A 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. Int. J. Cardiol. 2013, 167, 1860–1866.Lei, L.; Liu, Y. Efficacy of coenzyme Q10 in patients with cardiac failure: A meta-analysis of clinical trials. BMC Cardiovasc. Disord. 2017, 17, 196.
- Szeto, H.H. First-in-class cardiolipin-protective compound as a therapeutic agent to restore mitochondrial bioenergetics. Br. J. Pharmacol. 2014, 171, 2029–2050. Ribeiro Junior, R.F.; Dabkowski, E.R.; Shekar, K.C.O.; Connell, K.A.; Hecker, P.A.; Murphy, M.P. MitoQ improves mitochondrial dysfunction in heart failure induced by pressure overload. Free Radic. Biol. Med. 2018, 117, 18–29.
- Daubert, M.A.; Yow, E.; Dunn, G.; Marchev, S.; Barnhart, H.; Douglas, P.S.; O’Connor, C.; Goldstein, S.; Udelson, J.E.; Sabbah, H.N. Novel Mitochondria-Targeting Peptide in Heart Failure Treatment: A Randomized, Placebo-Controlled Trial of Elamipretide. Circ. Heart Fail. 2017, 10. Kalén, A.; Appelkvist, E.L.; Dallner, G. Age-related changes in the lipid compositions of rat and human tissues. Lipids 1989, 24, 579–584.
- Gibson, C.M.; Giugliano, R.P.; Kloner, R.A.; Bode, C.; Tendera, M.; Jánosi, A.; Merkely, B.; Godlewski, J.; Halaby, R.; Korjian, S.; et al. EMBRACE STEMI study: A Phase 2a trial to evaluate the safety, tolerability, and efficacy of intravenous MTP-131 on reperfusion injury in patients undergoing primary percutaneous coronary intervention. Eur. Heart J. 2016, 37, 1296–1303.Alehagen, U.; Johansson, P.; Björnstedt, M.; Rosén, A.; Dahlström, U. Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: A 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. Int. J. Cardiol. 2013, 167, 1860–1866.
- Heerdt, P.M.; Schlame, M.; Jehle, R.; Barbone, A.; Burkhoff, D.; Blanck, T.J.J. Disease-specific remodeling of cardiac mitochondria after a left ventricular assist device. Ann. Thorac. Surg. 2002, 73, 1216–1221.Szeto, H.H. First-in-class cardiolipin-protective compound as a therapeutic agent to restore mitochondrial bioenergetics. Br. J. Pharmacol. 2014, 171, 2029–2050.
- Lee, C.F.; Chavez, J.D.; Garcia-Menendez, L.; Choi, Y.; Roe, N.D.; Chiao, Y.A.; Edgar, J.S.; Goo, Y.A.; Goodlett, D.R.; Bruce, J.E.; et al. Normalization of NAD+ Redox Balance as a Therapy for Heart Failure. Circulation 2016, 134, 883–894. https://doi.org/10.1161/CIRCULATIONAHA.116.022495.
- Airhart, S.E.; Shireman, L.M.; Risler, L.J.; Anderson, G.D.; Nagana Gowda, G.A.; Raftery, D.; Tian, R.; Shen, D.D.; O’Brien, K.D. An open-label, non-randomized study of the pharmacokinetics of the nutritional supplement nicotinamide riboside (NR) and its effects on blood NAD+ levels in healthy volunteers. PLoS ONE 2017, 12, e0186459. https://doi.org/10.1371/journal.pone.0186459.
- Zhou, B.; Wang, D.D.-H.; Qiu, Y.; Airhart, S.; Liu, Y.; Stempien-Otero, A.; O’Brien, K.D.; Tian, R. Boosting NAD level suppresses inflammatory activation of PBMCs in heart failure. J. Clin. Investig. 2020, 130, 6054–6063. https://doi.org/10.1172/JCI138538.
- Dick, S.A.; Epelman, S. Chronic heart failure and inflammation. Circ. Res. 2016, 119, 159–176. Daubert, M.A.; Yow, E.; Dunn, G.; Marchev, S.; Barnhart, H.; Douglas, P.S.; O’Connor, C.; Goldstein, S.; Udelson, J.E.; Sabbah, H.N. Novel Mitochondria-Targeting Peptide in Heart Failure Treatment: A Randomized, Placebo-Controlled Trial of Elamipretide. Circ. Heart Fail. 2017, 10.
- Torre-Amione, G.; Kapadia, S.; Benedict, C.; Oral, H.; Young, J.B.; Mann, D.L. Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: A report from the Studies of Left Ventricular Dysfunction (SOLVD). J. Am. Coll. Cardiol. 1996, 27, 1201–1206.Gibson, C.M.; Giugliano, R.P.; Kloner, R.A.; Bode, C.; Tendera, M.; Jánosi, A.; Merkely, B.; Godlewski, J.; Halaby, R.; Korjian, S.; et al. EMBRACE STEMI study: A Phase 2a trial to evaluate the safety, tolerability, and efficacy of intravenous MTP-131 on reperfusion injury in patients undergoing primary percutaneous coronary intervention. Eur. Heart J. 2016, 37, 1296–1303.
- Testa, M.; Yeh, M.; Lee, P.; Fanelli, R.; Loperfido, F.; Berman, J.W.; LeJemtel, T.H. Circulating levels of cytokines and their endogenous modulators in patients with mild to severe congestive heart failure due to coronary artery disease or hypertension. J. Am. Coll. Cardiol. 1996, 28, 964–971.Heerdt, P.M.; Schlame, M.; Jehle, R.; Barbone, A.; Burkhoff, D.; Blanck, T.J.J. Disease-specific remodeling of cardiac mitochondria after a left ventricular assist device. Ann. Thorac. Surg. 2002, 73, 1216–1221.
- Mann, D.L. Past, Present, and the Foreseeable Future Scientific Rationale for Studying. Circ. Res. 2002, 91, 988–999.Dick, S.A.; Epelman, S. Chronic heart failure and inflammation. Circ. Res. 2016, 119, 159–176.
- Tabit, C.E.; Coplan, M.J.; Chen, P.; Jeevanandam, V.; Uriel, N.; Liao, J.K. Tumor necrosis factor- levels and non-surgical bleeding in continuous-flow left ventricular assist devices. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2018, 37, 107–115.Torre-Amione, G.; Kapadia, S.; Benedict, C.; Oral, H.; Young, J.B.; Mann, D.L. Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: A report from the Studies of Left Ventricular Dysfunction (SOLVD). J. Am. Coll. Cardiol. 1996, 27, 1201–1206.
- Chung, E.S.; Packer, M.; Lo, K.H.; Fasanmade, A.A.;Willerson, J.T. Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: Results of the anti-TNF Therapy Against Congestive Heart Failure. Circulation 2003, 107, 3133–3140.Testa, M.; Yeh, M.; Lee, P.; Fanelli, R.; Loperfido, F.; Berman, J.W.; LeJemtel, T.H. Circulating levels of cytokines and their endogenous modulators in patients with mild to severe congestive heart failure due to coronary artery disease or hypertension. J. Am. Coll. Cardiol. 1996, 28, 964–971.
- Sliwa, K.; Woodiwiss, A.; Kone, V.N.; Candy, G.; Badenhorst, D.; Norton, G.; Zambakides, C.; Peters, F.; Essop, R. Therapy of ischemic cardiomyopathy with the immunomodulating agent pentoxifylline: Results of a randomized study. Circulation 2004, 109, 750–755.Mann, D.L. Past, Present, and the Foreseeable Future Scientific Rationale for Studying. Circ. Res. 2002, 91, 988–999.
- Lecour, S.; Smith, R.M.;Woodward, B.; Opie, L.H.; Rochette, L.; Sack, M.N. Identification of a novel role for sphingolipid signaling in TNF and ischemic preconditioning mediated cardioprotection. J. Mol. Cell. Cardiol. 2002, 34, 509–518.Tabit, C.E.; Coplan, M.J.; Chen, P.; Jeevanandam, V.; Uriel, N.; Liao, J.K. Tumor necrosis factor-α levels and non-surgical bleeding in continuous-flow left ventricular assist devices. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2018, 37, 107–115.
- Abbate, A.; Van Tassell, B.W.; Biondi-Zoccai, G.; Kontos, M.C.; Grizzard, J.D.; Spillman, D.W.; Oddi, C.; Roberts, C.S.; Melchior, R.D.; Mueller, G.H.; et al. Effects of interleukin-1 blockade with anakinra on adverse cardiac remodeling and heart failure after acute myocardial infarction [from the Virginia Commonwealth University-Anakinra Remodeling Trial (2) (VCU-ART2) pilot study]. Am. J. Cardiol. 2013, 111, 1394–1400. https://doi.org/10.1016/j.amjcard.2013.01.287.
- Van Tassell, B.W.; Abouzaki, N.A.; Oddi Erdle, C.; Carbone, S.; Trankle, C.R.; Melchior, R.D.; Turlington, J.S.; Thurber, C.J.; Christopher, S.; Dixon, D.L.; et al. Interleukin-1 Blockade in Acute Decompensated Heart Failure: A Randomized, Double-Blinded, Placebo-Controlled Pilot Study. J. Cardiovasc. Pharmacol. 2016, 67, 544–551. https://doi.org/10.1097/FJC.0000000000000378.
- Buckley, L.F.; Abbate, A. Interleukin-1 Blockade in Cardiovascular Diseases: From Bench to Bedside. BioDrugs 2018, 32, 111–118. https://doi.org/10.1007/s40259-018-0274-5.
- Elzman, C.R.H.S.; Al, H.E.T. Interleukin-1 Receptor Antagonism as Adjunct Therapy for Heart Failure Patients with Left Ventricular Assist Devices. Clin. Trial 2021, 67, 145–147. https://doi.org/10.1097/MAT.0000000000001347.
- Samuel, T.J.; Rosenberry, R.P.; Lee, S.; Pan, Z. Correcting Calcium Dysregulation in Chronic Heart Failure Using SERCA2a Gene Therapy. Int. J. Mol. Sci. 2018, 19, 1086.Chung, E.S.; Packer, M.; Lo, K.H.; Fasanmade, A.A.; Willerson, J.T. Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: Results of the anti-TNF Therapy Against Congestive Heart Failure. Circulation 2003, 107, 3133–3140.
- del Monte, F.; Harding, S.E.; Schmidt, U.; Matsui, T.; Kang, Z.B.; Dec, G.W.; Gwathmey, J.K.; Rosenzweig, A.; Hajjar, R.J. Restoration of contractile function in isolated cardiomyocytes from failing human hearts by gene transfer of SERCA2a. Circulation 1999, 100, 2308–2311.Sliwa, K.; Woodiwiss, A.; Kone, V.N.; Candy, G.; Badenhorst, D.; Norton, G.; Zambakides, C.; Peters, F.; Essop, R. Therapy of ischemic cardiomyopathy with the immunomodulating agent pentoxifylline: Results of a randomized study. Circulation 2004, 109, 750–755.
- Zsebo, K.; Yaroshinsky, A.; Rudy, J.J.;Wagner, K.; Greenberg, B.; Jessup, M.; Hajjar, R.J. Long-term effects of AAV1/SERCA2a gene transfer in patients with severe heart failure: Analysis of recurrent cardiovascular events and mortality. Circ. Res. 2014, 114, 101–108. Lecour, S.; Smith, R.M.; Woodward, B.; Opie, L.H.; Rochette, L.; Sack, M.N. Identification of a novel role for sphingolipid signaling in TNFα and ischemic preconditioning mediated cardioprotection. J. Mol. Cell. Cardiol. 2002, 34, 509–518.
- Lyon, A.R.; Babalis, D.; Morley-Smith, A.C.; Hedger, M.; Suarez Barrientos, A.; Foldes, G.; Couch, L.S.; Chowdhury, R.A.; Tzortzis, K.N.; Peters, N.S.; et al. Investigation of the safety and feasibility of AAV1/SERCA2a gene transfer in patients with chronic heart failure supported with a left ventricular assist device-the SERCA-LVAD TRIAL. Gene Ther. 2020, 27, 579–590.Samuel, T.J.; Rosenberry, R.P.; Lee, S.; Pan, Z. Correcting Calcium Dysregulation in Chronic Heart Failure Using SERCA2a Gene Therapy. Int. J. Mol. Sci. 2018, 19, 1086.
- Chioncel, O.; Collins, S.P.; Butler, J. Istaroxime in acute heart failure: The holy grail is at HORIZON? Eur. J. Heart Fail. 2020, 22, 1694–1697.del Monte, F.; Harding, S.E.; Schmidt, U.; Matsui, T.; Kang, Z.B.; Dec, G.W.; Gwathmey, J.K.; Rosenzweig, A.; Hajjar, R.J. Restoration of contractile function in isolated cardiomyocytes from failing human hearts by gene transfer of SERCA2a. Circulation 1999, 100, 2308–2311.
- Carubelli, V.; Zhang, Y.; Metra, M.; Lombardi, C.; Felker, G.M.; Filippatos, G.; O’Connor, C.M.; Teerlink, J.R.; Simmons, P.; Segal, R.; et al. Treatment with 24 hour istaroxime infusion in patients hospitalised for acute heart failure: A randomised, placebo-controlled trial. Eur. J. Heart Fail. 2020, 22, 1684–1693.Zsebo, K.; Yaroshinsky, A.; Rudy, J.J.; Wagner, K.; Greenberg, B.; Jessup, M.; Hajjar, R.J. Long-term effects of AAV1/SERCA2a gene transfer in patients with severe heart failure: Analysis of recurrent cardiovascular events and mortality. Circ. Res. 2014, 114, 101–108.
- Metra, M.; Chioncel, O.; Cotter, G.; Davison, B.; Filippatos, G.; Mebazaa, A.; Novosadova, M.; Ponikowski, P.; Simmons, P.; Soffer, J.; et al. Safety and Efficacy of Istaroxime for Patients with Acute-Heart-Failure-Related Pre-cardiogenic Shock—A Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel Group Study (SEISMiC). Eur. J. Heart Fail. 2022, doi:10.1002/ejhf.2629.
- Aryan, L.; Younessi, D.; Zargari, M.; Banerjee, S.; Agopian, J.; Rahman, S.; Borna, R.; Ruffenach, G.; Umar, S.; Eghbali, M. The Role of Estrogen Receptors in Cardiovascular Disease. Int. J. Mol. Sci. 2020, 21. https://doi.org/10.3390/ijms21124314.
- Iorga, A.; Cunningham, C.M.; Moazeni, S.; Ruffenach, G.; Umar, S.; Eghbali, M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex Differ. 2017, 8, 33. https://doi.org/10.1186/s13293-017-0152-8.
- Iorga, A.; Li, J.; Sharma, S.; Umar, S.; Bopassa, J.C.; Nadadur, R.D.; Centala, A.; Ren, S.; Saito, T.; Toro, L.; et al. Rescue of Pressure Overload-Induced Heart Failure by Estrogen Therapy. J. Am. Heart Assoc. 2016, 5. https://doi.org/10.1161/JAHA.115.002482.
- Lagranha, C.J.; Deschamps, A.; Aponte, A.; Steenbergen, C.; Murphy, E. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ. Res. 2010, 106, 1681–1691. https://doi.org/10.1161/CIRCRESAHA.109.213645.
- Gardner, J.D.; Murray, D.B.; Voloshenyuk, T.G.; Brower, G.L.; Bradley, J.M.; Janicki, J.S. Estrogen attenuates chronic volume overload induced structural and functional remodeling in male rat hearts. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H497-504. https://doi.org/10.1152/ajpheart.00336.2009.
- Frump, A.L.; Albrecht, M.; Yakubov, B.; Breuils-Bonnet, S.; Nadeau, V.; Tremblay, E.; Potus, F.; Omura, J.; Cook, T.; Fisher, A.; et al. 17β-Estradiol and estrogen receptor α protect right ventricular function in pulmonary hypertension via BMPR2 and apelin. J. Clin. Investig. 2021, 131. https://doi.org/10.1172/JCI129433.
- Metra, M.; Chioncel, O.; Cotter, G.; Davison, B.; Filippatos, G.; Mebazaa, A.; Novosadova, M.; Ponikowski, P.; Simmons, P.; Soffer, J.; et al. Safety and Efficacy of Istaroxime for Patients with Acute-Heart-Failure-Related Pre-cardiogenic Shock—A Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel Group Study (SEISMiC). Eur. J. Heart Fail. 2022, doi:10.1002/ejhf.2629.
- Aryan, L.; Younessi, D.; Zargari, M.; Banerjee, S.; Agopian, J.; Rahman, S.; Borna, R.; Ruffenach, G.; Umar, S.; Eghbali, M. The Role of Estrogen Receptors in Cardiovascular Disease. Int. J. Mol. Sci. 2020, 21. https://doi.org/10.3390/ijms21124314.
- Iorga, A.; Cunningham, C.M.; Moazeni, S.; Ruffenach, G.; Umar, S.; Eghbali, M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex Differ. 2017, 8, 33. https://doi.org/10.1186/s13293-017-0152-8.
- Iorga, A.; Li, J.; Sharma, S.; Umar, S.; Bopassa, J.C.; Nadadur, R.D.; Centala, A.; Ren, S.; Saito, T.; Toro, L.; et al. Rescue of Pressure Overload-Induced Heart Failure by Estrogen Therapy. J. Am. Heart Assoc. 2016, 5. https://doi.org/10.1161/JAHA.115.002482.
- Lagranha, C.J.; Deschamps, A.; Aponte, A.; Steenbergen, C.; Murphy, E. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ. Res. 2010, 106, 1681–1691. https://doi.org/10.1161/CIRCRESAHA.109.213645.
- Gardner, J.D.; Murray, D.B.; Voloshenyuk, T.G.; Brower, G.L.; Bradley, J.M.; Janicki, J.S. Estrogen attenuates chronic volume overload induced structural and functional remodeling in male rat hearts. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H497-504. https://doi.org/10.1152/ajpheart.00336.2009.
- Frump, A.L.; Albrecht, M.; Yakubov, B.; Breuils-Bonnet, S.; Nadeau, V.; Tremblay, E.; Potus, F.; Omura, J.; Cook, T.; Fisher, A.; et al. 17β-Estradiol and estrogen receptor α protect right ventricular function in pulmonary hypertension via BMPR2 and apelin. J. Clin. Investig. 2021, 131. https://doi.org/10.1172/JCI129433.
- Metra, M.; Chioncel, O.; Cotter, G.; Davison, B.; Filippatos, G.; Mebazaa, A.; Novosadova, M.; Ponikowski, P.; Simmons, P.; Soffer, J.; et al. Safety and Efficacy of Istaroxime for Patients with Acute-Heart-Failure-Related Pre-cardiogenic Shock—A Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel Group Study (SEISMiC). Eur. J. Heart Fail. 2022, doi:10.1002/ejhf.2629.
- Aryan, L.; Younessi, D.; Zargari, M.; Banerjee, S.; Agopian, J.; Rahman, S.; Borna, R.; Ruffenach, G.; Umar, S.; Eghbali, M. The Role of Estrogen Receptors in Cardiovascular Disease. Int. J. Mol. Sci. 2020, 21. https://doi.org/10.3390/ijms21124314.
- Iorga, A.; Cunningham, C.M.; Moazeni, S.; Ruffenach, G.; Umar, S.; Eghbali, M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex Differ. 2017, 8, 33. https://doi.org/10.1186/s13293-017-0152-8.
- Iorga, A.; Li, J.; Sharma, S.; Umar, S.; Bopassa, J.C.; Nadadur, R.D.; Centala, A.; Ren, S.; Saito, T.; Toro, L.; et al. Rescue of Pressure Overload-Induced Heart Failure by Estrogen Therapy. J. Am. Heart Assoc. 2016, 5. https://doi.org/10.1161/JAHA.115.002482.
- Lagranha, C.J.; Deschamps, A.; Aponte, A.; Steenbergen, C.; Murphy, E. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ. Res. 2010, 106, 1681–1691. https://doi.org/10.1161/CIRCRESAHA.109.213645.
- Gardner, J.D.; Murray, D.B.; Voloshenyuk, T.G.; Brower, G.L.; Bradley, J.M.; Janicki, J.S. Estrogen attenuates chronic volume overload induced structural and functional remodeling in male rat hearts. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H497-504. https://doi.org/10.1152/ajpheart.00336.2009.
- Frump, A.L.; Albrecht, M.; Yakubov, B.; Breuils-Bonnet, S.; Nadeau, V.; Tremblay, E.; Potus, F.; Omura, J.; Cook, T.; Fisher, A.; et al. 17β-Estradiol and estrogen receptor α protect right ventricular function in pulmonary hypertension via BMPR2 and apelin. J. Clin. Investig. 2021, 131. https://doi.org/10.1172/JCI129433.
- McCarthy, P.M.; Nakatani, S.; Vargo, R.; Kottke-Marchant, K.; Harasaki, H.; James, K.B.; Savage, R.M.; Thomas, J.D. Structural and left ventricular histologic changes after implantable LVAD insertion. Ann. Thorac. Surg. 1995, 59, 609–613. https://doi.org/10.1016/0003-4975(94)00953-8.
- Frazier, O.H. First use of an untethered, vented electric left ventricular assist device for long-term support. Circulation 1994, 89, 2908–2914. https://doi.org/10.1161/01.cir.89.6.2908.
- Frazier, O.H.; Benedict, C.R.; Radovancevic, B.; Bick, R.J.; Capek, P.; Springer, W.E.; Macris, M.P.; Delgado, R.; Buja, L.M. Improved left ventricular function after chronic left ventricular unloading. Ann. Thorac. Surg. 1996, 62, 672–675. https://doi.org/10.1016/s0003-4975(96)00437-7.
- Loebe, M.; Weng, Y.; Müller, J.; Dandel, M.; Halfmann, R.; Spiegelsberger, S.; Hetzer, R. Successful mechanical circulatory support for more than two years with a left ventricular assist device in a patient with dilated cardiomyopathy. J. Heart lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 1997, 16, 1176–1179.
