Therefore, cardioprotective strategies are of paramount importance. They include primary and secondary prevention. It is crucial to risk stratify cancer patients prior to therapy initiation to recognize those at high risk for cardiotoxicity and follow them up throughout and after the therapeutic process in order to treat in a timely manner for cardiovascular therapy effects.
Current therapeutic protocols often include multiple agents resulting in additive or synergistic cardiotoxic effects. Cancer therapeutic agents that are mainly linked to cardiovascular toxicity include anthracyclines, human epidermal growth factor-2 inhibitors (HER2s), vascular endothelial growth factor inhibitors (VEGFs), Bcr-Abl kinase inhibitors (Bcr-Abls), proteasome inhibitors (proteasomes), ICs, and ibrutinib.
2. Preventive Strategies
The appropriate selection of cancer patients who could benefit from cardioprotective strategies still remains a major issue. There is a lack of agreement on the definition of high-risk patients and limited data to support specific preventive strategies in certain patient populations. Most trials focus on systolic dysfunction and biomarkers.
Interestingly, there is no universally accepted definition for cardiac toxicity. The Cardiac Review and Evaluation Committee in an attempt to combine different definitions from various organizations proposed the presence of at least one of the following criteria for the diagnosis of cardiotoxicity: (1) cardiomyopathy characterized by a decrease in cardiac LVEF, either global or more severe in the interventricular septum, (2) symptoms of congestive heart failure (CHF), (3) associated signs of CHF, including but not limited to S3 gallop, tachycardia, or both, and (4) decrease in LVEF of at least 5% to less than 55% with accompanying signs or symptoms of CHF, or a decline in LVEF of at least 10% to below 55% without accompanying signs or symptoms
[1].
Cardiovascular complications encompass variable entities apart from myocardial dysfunction and heart failure (HF), such as valvular disease, pulmonary hypertension, pericardial complications, coronary artery disease (CAD), arrhythmias, arterial hypertension, thromboembolic disease, peripheral vascular disease, and stroke. Cardiotoxic effects can occur either in the short or in the long-term following treatment and they may be transient or irreversible
[2].
3. Primary Prevention of Cardiotoxicity
3.1. Identification and Management of Cardiotoxicity Risk Factors
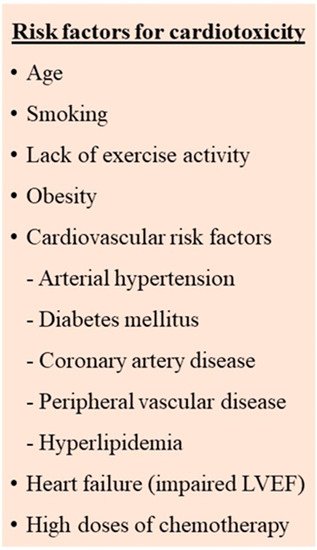
The early identification and management of the risk factors for cardiovascular side effects seems to contribute to the prevention or minimization of cardiotoxicity. Numerous risk factors, both patient-related as well as therapy-related, have been described (
Figure 1)
[2][3][4][5][2,3,4,5]. However, there are still differences in the definition of the high-risk patient as well as the type and the timing of the recommended investigations.
Figure 1.
Risk factors for cardiotoxicity in cancer patients receiving chemotherapy.
The main patient-related risk factors appear to be the pre-existence of cardiac risk factors such as diabetes mellitus, hypertension, dyslipidemia, smoking, increased body weight as well as previous history of cardiovascular disease, left ventricular dysfunction, heart failure, and coronary artery disease. Other factors such as chronic kidney disease, increasing age, female gender, and postmenopausal status have also been proposed. Active management of the modifiable risk factors according to current guidelines is needed. Additionally, tobacco cessation, regular exercise, and a healthy diet are recommended as primary preventive measures to improve outcomes
[2][3][5][6][2,3,5,6].
At the moment, there are no specific cardiovascular risk scores for cancer patients that can accurately calculate their risk. Therefore, the assessment of these patients using the risk scores for the general population is recommended at the time of diagnosis
[7].
A retrospective cohort study in 36,232 adult cancer patients ≥2-year survivors, showed that survivors with two or more cardiovascular risk factors had the highest percentage of ischemic heart disease, stroke, and cardiomyopathy, heart failure when compared to noncancer matched controls. Overall survival in cancer patients who developed cardiovascular disease (CVD) was poor, accounting for 60% at 8 years compared to 81% in cancer survivors without CVD, underlying the need for cardioprevention in individuals at highest risk for cardiovascular disease
[8].
The principal therapy-related factors include the combination of multiple agents, (particularly if they are administered simultaneously or in bolus doses), the addition of mediastinal radiotherapy, and higher doses of chemotherapeutic agents.
Certain agents, such as anthracycline, trastuzumab, and cyclophosphamide give a higher cardiotoxicity risk while others such as etoposide, bevacizumab, and lapatinib seem to carry a lower risk
[9]. Of note, previous anthracycline treatment increases the risk in patients presenting with recurrent disease or even a new malignancy requiring further anthracycline therapy
[10]. Genetic polymorphisms have also been described as possible predisposing factors at lower anthracycline doses, suggesting that the genetic substrate could modify the risk of cardiotoxicity after cancer treatment
[2][11][2,11].
3.2. Cardiovascular Assessment
A thorough cardiovascular assessment and active surveillance are needed before, during, and following the therapeutic process in order to prevent and/or detect cardiovascular toxicity. A combination of imaging evaluation and serum biomarkers has been suggested by several Cardiology and Oncology societies
[12][13][14][15][12,13,14,15].
The French Working Group of Cardio-Oncology proposes the combination of the following cardiotoxicity risk factors, taking into account the patient’s previous history, the biomarkers, the dose and type of the therapeutic agents, and imaging findings: previous heart disease, elevated cardiac biomarkers before initiation of anticancer therapy (N-terminal pro-B-type natriuretic peptide or B-type natriuretic peptide and/or troponin), high-dose anthracycline therapy (e.g., doxorubicin ≥ 250 mg/m
2, epirubicin ≥ 600 mg/m
2), high radiotherapy dose (≥30 Gy) with the heart in the treatment field or lower-dose of anthracycline or HERs or VEGFs or proteasomes or Bcr-Abls but with the presence of any of the following risk factors: older age ≥ 60 years, lower radiotherapy dose (<30 Gy) where the heart is in the treatment field, ≥2 risk factors which include diabetes mellitus, hypertension, dyslipidemia, smoking, chronic kidney disease, and obesity
[3].
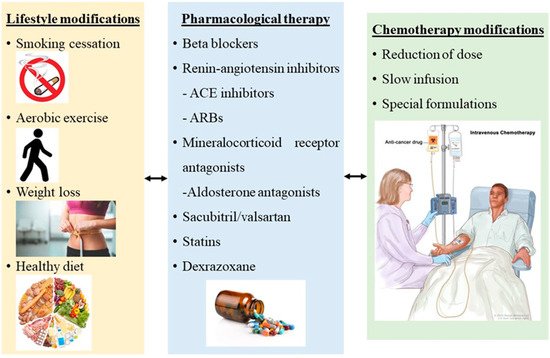
3.3. Cardioprotective Medical Therapy
During the last two decades, the established and most approved strategic management of prevention and treatment of chemotherapy-induced cardiotoxicity in HF with LV dysfunction and LVEF < 40% is the use of b-blockers, renin–angiotensin inhibitors including angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), statins, the use of dexrazoxane and a non-pharmaceutical approach, physical exercise (
Figure 23)
[16][19].
Figure 23.
Cardioprotective strategies against chemotherapy cardiotoxicity in cancer patients.
Beta-blockers have the ability to increase prosurvival signaling through the EGFR pathway and mitigate free radicals. Several b-blockers have been used in several studies within the last years
[17][18][19][20][21][22][23][24][25][20,21,22,23,24,25,26,27,28], but carvedilol and nebivolol seem to be the most efficient so far. Specifically, carvedilol is a third-generation nonselective BB that reduces free radicals, prevents mitochondrial dysfunction, and inhibits lipid peroxidation
[26][27][29,30]. Daily use of carvedilol twice a day has been shown to contribute to lower troponin I levels and lower incidence of diastolic dysfunction in patients with cancer under chemotherapeutic agents compared to controls
[17][20][23][25][20,23,26,28], as well as unchanged dimensions in LV basal septal, lateral peak systolic strain and strain-rate parameters after chemotherapy compared to controls
[18][19][21,22]. Another b-blocker, nebivolol is another third-generation BB with vasodilatory and antioxidant properties that increases nitrous oxide and decrease reactive oxygen species
[28][31]. It has been shown to have similar beneficial effects in myocardium as 5 mg on a daily basis protects from impairment in LVEF compared to controls
[22][25].
Another category of cardioprotective medication for cardiotoxicity is renin–angiotensin inhibitors including ACE inhibitors and ARBs. ACE inhibitors and ARBs are neurohormonal blocking agents, used to treat hypertension and facilitate cardiac remodeling
[29][32]. Their action is through the attenuation of oxidative stress and myocardial fibrosis
[30][31][18,33]. They also improve intracellular calcium handling, cardiomyocyte metabolism, and mitochondrial function
[30][31][18,33]. Lisinopril has been shown to protect LVEF and present lower long-term cardiovascular events compared to the placebo group, in a study of 114 patients receiving anthracyclines
[30][18]. Enalapril is another ACE inhibitor that has been used daily as a protective strategy in patients receiving chemotherapeutic agents. In a study by Cardinale et al.
[32][34], daily use of enalapril at the start of chemotherapy showed significantly lower elevation of troponin and fewer cardiotoxicity incidents compared to the troponin-triggered enalapril therapy group. Another study by Janbabai et al.
[33][35], showed that daily use of enalapril results in lower incidences of LV diastolic dysfunction from baseline at 6 months, and significantly unchanged tissue Doppler, E/e’ ratio, mean LVEF, and cTnI and CK-MB levels compared to the control group where measurements were worse after chemotherapy. An ARB agent, valsartan was also shown to have cardioprotective properties. Specifically, a low dose of 80 mg daily was observed to significantly inhibit the dilatation of LVDd, the elevation of BNP, and the prolongation of the QTc interval and QTc dispersion in 40 patients undergoing chemotherapy
[34][36].
The combination of a b-blockers and a renin–angiotensin inhibitor, however, seems controversial as if it could be suggested as the most appropriate and efficient method of cardioprotection in patients with malignancies undergoing chemotherapy. Two big studies, the OVERCOME and the PRADA trial, combined a b-blocker and a renin–angiotensin inhibitor in the intervention group and compared it to a control group of either placebo treatment or treatment with a b-blocker or a renin–angiotensin inhibitor separately. In the first trial
[35][37], investigators administered carvedilol and lisinopril together at the start of chemotherapy to their patients and compared it to a control group of placebo treatment. The combination was shown to be effective at preventing the decline in LVEF compared to the placebo. In the other trial, the PRADA trial
[36][38], investigators examined the combination of 32 mg of candesartan and 100 mg of metoprolol versus candesartan alone, or metoprolol alone or placebo therapy. They observed that breast cancer patients receiving canderstartan during anthracycline chemotherapy had less LVEF decline but metoprolol did not have the same effect. They also observed that there was no additional benefit when metoprolol was used in conjunction with candesartan
[36][38]. Finally, another big trial, the MANTICORE 101–Breast trial
[37][39], investigated the early treatment with perindopril, bisoprolol, or placebo (1:1:1) in patients with HER2-positive early breast cancer for the duration of trastuzumab adjuvant therapy. It was shown that perindopril and bisoprolol protected against cancer-therapy-related declines in LVEF while LV remodeling could not be prevented. There were no other studies demonstrating the beneficial effects of the combination of b-blockers and renin–angiotensin inhibitors.
The use of another medication, sacubitril/valsartan, is still under investigation regarding the cardioprotective effect in cancer patients. Sacubitril/valsartan belongs to the angiotensin receptor-neprilysin inhibitors (ARNIs) and has been approved as a first-line treatment in HFrEF patients. Unfortunately, data are still limited regarding this category. There is a randomized prospective study
[38][40] comparing valsartan/sacubitril to candesartan in 112 breast cancer patients with reduced LVEF prior to getting anthracyclines. Th
eis study showed that valsartan/sacubitril group presented less rise in BNP, increased 6-min walk test, better suppression of ventricular arrhythmias, and improved indicators of LV function compared to the candesartan group
[38][40]. However, more randomized clinical trials are required in order to support the use of ARNIs in chemotherapy-related cardiomyopathies.
Mineralocorticoid receptor antagonist blockades, such as aldosterone antagonists, are widely used in patients with HFrEF and suppress fibrosis, leading to improvement of their symptoms
[39][41]. There is a single randomized, double-blind, placebo-controlled study
[40][42] including 43 breast cancer women who received 25 mg of spironolactone daily and were compared to 40 women under placebo treatment. Both groups were receiving doxorubicin or epirubicin. The study showed that spironolactone provided significant short-term cardioprotection by significantly less decrease in LVEF, preserved LV diastolic functional grade, and unchanged serum cardiac biomarker concentrations including creatine kinase-MB, cTnI, and NT-proBNP compared to controls where all indices deteriorated after chemotherapy. Moreover, total oxidative capacity and the oxidative stress index were more pronounced in controls
[40][42].
Anthracyclines increase the reactive oxygen species, oxidative stress and inflammation and cause cardiotoxicity
[41][43]. Statins reduce cholesterol synthesis by inhibiting the enzyme HMG CoA reductase and they are known to exhibit pleiotropic properties and decrease oxidative stress and inflammation
[42][44]. They can also improve endothelial function and nitric oxide delivery
[43][45]. Thus, they may potentially protect against anthracycline-induced cardiac damage
[42][44]. Statins have been used as a cardioprotective strategy against cardiotoxicity in patients with cancer. Specifically, 67 women with newly diagnosed breast cancer were treated with statins during chemotherapy with anthracyclines and had a lower risk of HF (HR, 0.3; 95% CI, 0.1 to 0.9;
p = 0.03) compared to 134 women not treated with statins
[44][46]. Statins are also shown to prevent a drop in LVEF after chemotherapy with anthracyclines compared to placebo
[45][47]. Indeed, higher statin doses (40–80 mg) could actually have an increase in LVEF
[45][47]. The cardioprotective effects of statins have been also shown in other studies
[46][47][48,49], not only in anthracyclines but also in trastuzumab therapy
[48][50].
Dexrazoxane is the only approved drug by FDA for preventing anthracycline-induced cardiotoxicity
[49][51]. It has been approved to be given to children and adolescents that are likely to be treated with high cumulative doses of anthracyclines (>300 mg/m
2 of doxorubicin)
[50][52]. Its action mechanism is to reduce ROS formation via the prevention of anthracycline–iron complex formation
[16][19]. Specifically, dexrazoxane has the ability to bind iron before it enters cardiomyocytes, preventing thus, the formation of the iron–anthracycline complex, free radical formation, and cardiac damage
[51][52][53,54]. In addition, it prevents anthracyclines from binding to topoisomerase 2β which would lead to cardiomyocyte death and mitochondrial dysfunction
[53][55]. It has been used as a cardioprotective agent against anthracycline-induced cardiotoxicity for over 30 years in many types of solid and hematological malignancies, not only in adults but also in children receiving doxorubicin and other anthracycline drugs. Dexrazoxane has been shown to have fewer rates of asymptomatic LV dysfunction, lower rates of HF progression, better LV performance, and fewer cardiac events in patients treated with doxorubicin and dexrazoxane
[54][55][56][57][56,57,58,59]. Moreover, no changes in cardiac troponin I or brain natriuretic peptide concentrations are observed with dexrazoxane
[58][60]. In summary, dexrazoxane’s effectiveness in reducing anthracycline-related cardiotoxicity in patients with cancer is already proven throughout the years.
Finally, a non-pharmaceutical cardioprotective strategy in patients with cancer under chemotherapy, exercise, has been also studied in the last years. Exercise decreases ROS formation, improves endothelial function, and decreases intracellular anthracycline levels
[16][59][60][61][19,61,62,63]. It also increases heart tolerance against many cardiotoxic agents and therefore improves several functional, subclinical, and clinical parameters
[62][64]. Cancer patients usually decrease their physical activity from pre- to post-diagnosis and gain approximately 3 kg during chemotherapy
[63][64][65,66]. As a result, their functional capacity is being deteriorated as shown in peak VO2 during cardiopulmonary exercise testing
[65][67]. The American College of Sports Medicine published a consensus regarding exercise safety for specific patient groups with malignancies and cancer survivors, confirming exercise’s overall safety and efficacy
[66][68].