Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Camila Xu and Version 1 by Wojciech Konarski.
Medial epicondylalgia (ME), commonly known as “the golfer’s elbow”, typically develops in individuals who perform repetitive forearm movements and weight-bearing activities. It accounts for up to 20% of all epicondylitis cases and is most prevalent in particular sports and occupations.
- elbow
- ultrasound
- differential diagnosis
1. Introduction
Epicondylalgia remains one of the most common elbow disorders. It occurs mainly when specific movements, namely flexion and extension, followed by pronation and supination of the elbow, are repeated over a long period [1]. Excessive joint strain over time results in micro-trauma accumulation at the tendon attachment. This, in turn, leads to local tenderness, swelling, and ulnar nerve irritation, which results in pain and discomfort with activity, but it may also be present at rest [2].
The first literature report on epicondylalgia was published in 1882. The condition was then described as ‘lawn-tennis arm’ because the disorder was first observed in tennis players [3]. Since that time, knowledge about this entity has increased, and currently, it is known that epicondylalgia may involve either medial or lateral epicondyle. Lateral epicondylalgia (LE), also known as ‘the tennis elbow’, results from injury to the attachment of extensor carpi radialis brevis but may extend to other tendons. In turn, medial epicondylalgia (ME), called ‘the golfer’s elbow’, involves the muscles originating on the medial epicondyle of the humerus [4]. Although their common names suggest a close relationship with particular types of sport, they are also observed in many people who perform other activities involving repetitive hand movements [3,4][3][4].
Though ME is mainly diagnosed during routine clinical examination, it should be confirmed using imaging modalities. New imaging techniques, especially magnetic resonance (MRI), were propagated to diagnose elbow pathologies in recent decades. For chronic elbow pain, MRI became the first-choice imaging modality [5]. Typically, MRI allows for establishing a proper diagnosis [5]. However, it does not enable real-time dynamic examination of the joint [4]. Ultrasound (US) offers such a possibility, which is gaining popularity in osteoarticular diagnostic and therapeutic purposes [6].
Contrary to the MRI, US examination is more accessible and less expensive. In the case of a well-trained orthopedic surgery specialist with a solid knowledge of normal anatomy, this imaging tool might be non-inferior to MRI and other currently available imaging modalities [6,7,8][6][7][8]. Notwithstanding, modern technical solutions, including harmonic and spatial compound imaging, have brought significant noise and artifact reduction improvements, contributing to an increase in image quality. Recently introduced phase-inversion techniques also improve the field’s depth and signal-to-noise ratio. That together with technological advances in ultrasound probes allows for image quality comparable to that of an MRI [7,9][7][9].
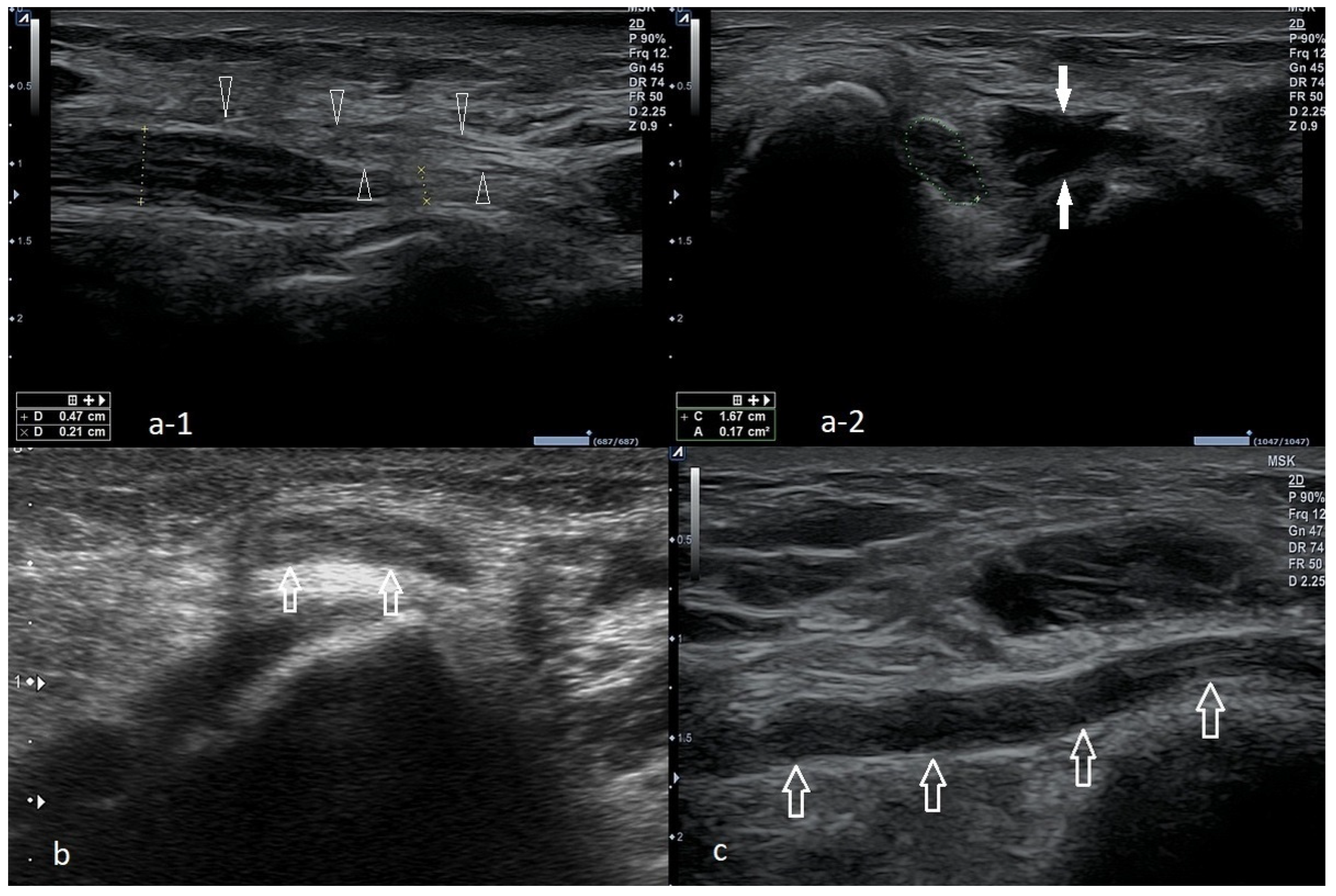
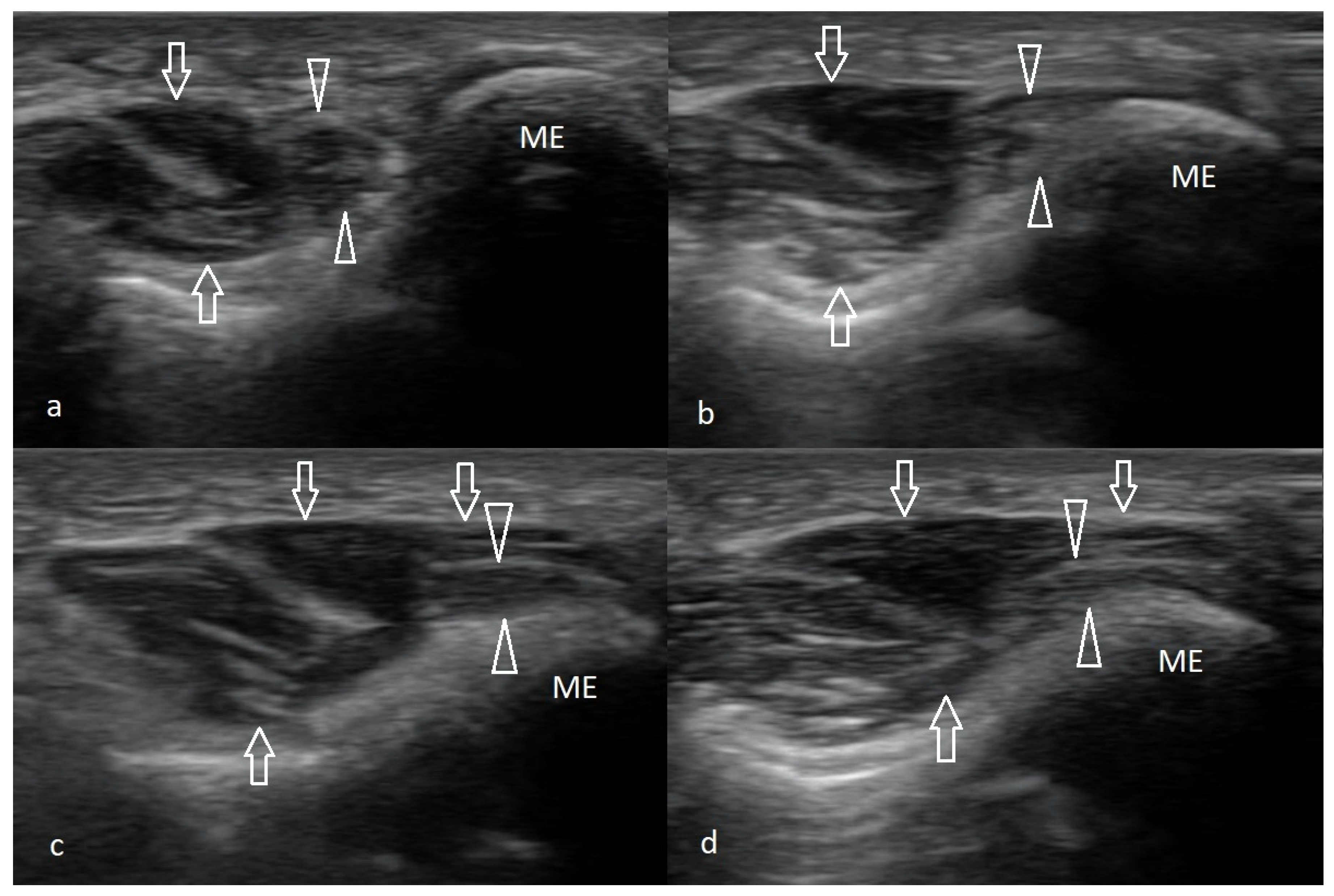
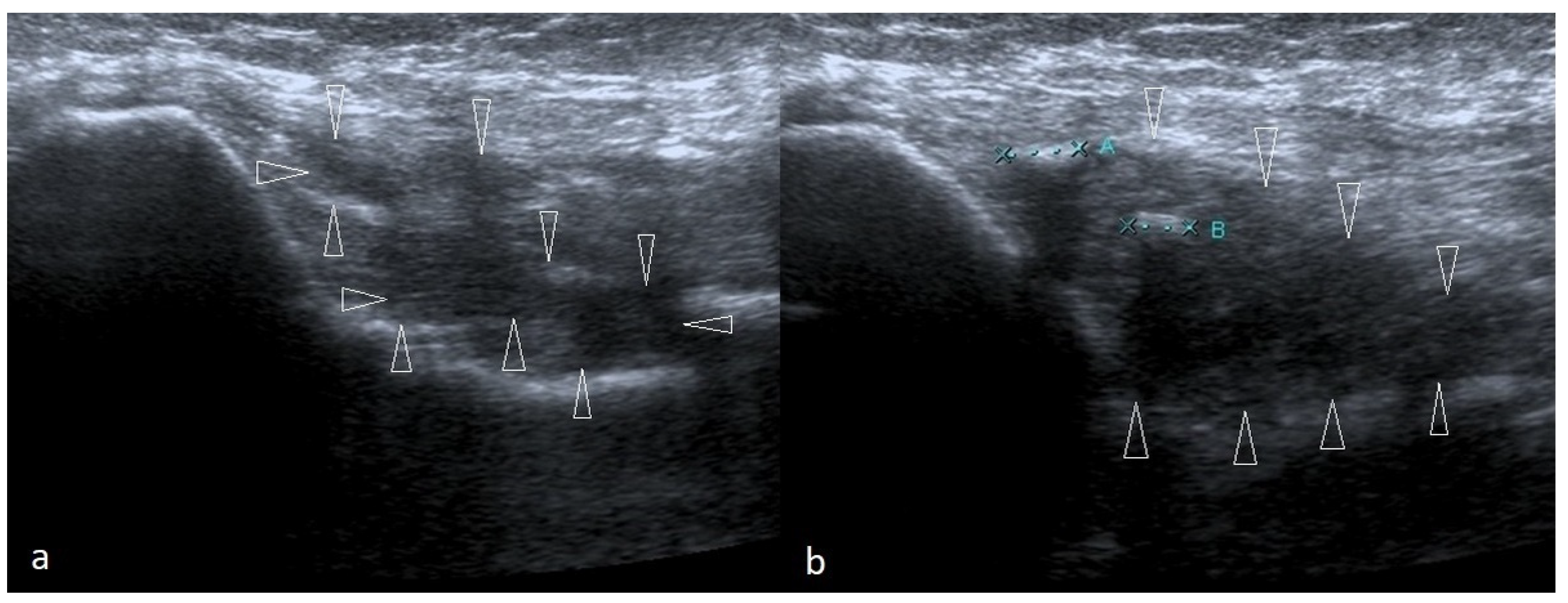 Figure 3. Two cases of post-traumatic changes within the medial collateral ligament and profound part of the common flexor tendon. In both pictures (a,b), the areas of hypoechoic scarring are marked with arrowheads; post-traumatic calcifications are also visible.
Figure 3. Two cases of post-traumatic changes within the medial collateral ligament and profound part of the common flexor tendon. In both pictures (a,b), the areas of hypoechoic scarring are marked with arrowheads; post-traumatic calcifications are also visible.
2. Ultrasound in Medial Epicondylalgia and Medial Elbow Pain
ME diagnosis may be based on the physical examination and the patient’s medical history. Nonetheless, ME is a relatively uncommon disease with unspecific symptoms, so the entity can easily be confused with other sources of elbow pain—features differentiating ME from other conditions [34,51][10][11].2.1. Cubital Tunnel Syndrome and Ulnar Neuritis
Cubital tunnel syndrome is the second most common compression neuropathy. The ulnar nerve courses behind the medial epicondyle, so the pressure or stretching in this area may affect the shape of the cubital tunnel, which causes pain [34][10]. However, contrary to ME, where pain with activity is the leading symptom, most patients report sensory loss first. Numbness, tingling sensation, and weakness of the forearm muscles can also occur [34,52][10][12]. Diagnosis of cubital tunnel syndrome may be facilitated with the Tinel test, which involves direct gentle compression over the nerve course at the elbow level. The test is positive when a sensation of tingling and paresthesia occurs [5,10,34,37][5][10][13][14]. The diagnosis can be excluded by performing electromyography (EMG). It might also elucidate the site of nerve compression and the degree of nerve damage. Some reseauthorchers recommend screening patients for systemic and metabolic disorders that might predispose them to this condition [53,54][15][16]. At times, the neuropathy might result from nerve instability or subluxation. Nerve displacement occurs mainly during forearm flexion to more than 90 degrees [55][17]. When the ulnar nerve dislocates from its groove, it becomes irritated, which might be captured on the US as nerve swelling. The dislocation might be observed when examining the nerve with a supinated forearm. A patient is asked to flex the forearm until the full flexion is reached gradually [55][17]. Nonetheless, ulnar nerve edema might be secondary to forceful work or after long periods of forearm flexion. In such circumstances, the patient might also experience symptoms indicative of neuropathy [55][17]. The US image of ulnar nerve pathologies is depicted in Figure 91.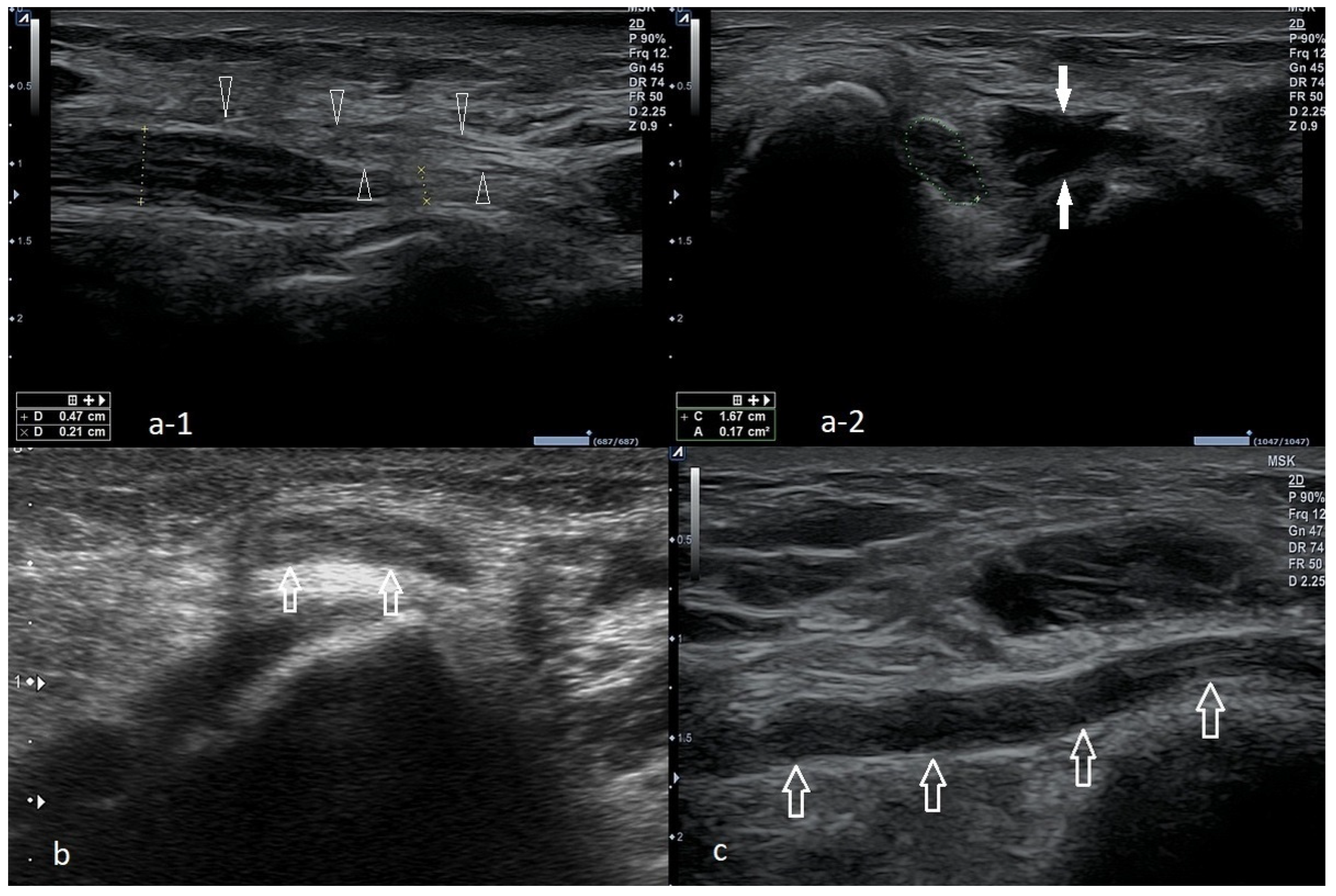
Figure 91. Three cases of the ulnar nerve neuropathy of different etiologies. (a-1)—Long-axis view of the ulnar nerve, visible compression of the nerve at the level of the arcuate ligament (the narrowing of the nerve is accompanied by increased echogenicity); proximal to the stenosis site, nerve swelling is visible, expressed as a thickening, decreased echogenicity without the typical echo structure. Arrowheads—Osborn’s ligament transforming into an arcuate ligament in the distal direction. (a-2)—The same case, cross-section at the level of the sulcus, significantly increased cross-sectional area (0.17 cm2, with the norm defined by most reseauthorchers at 0.09 cm2), although in the longitudinal section, a nerve compression is visible at the level of the arcuate ligament; in this case, at the level of the sulcus there is also a visible muscular structure that may correspond to the anconeus epitrochlearis (marked with white arrows). (b)—A case of instability of the ulnar nerve, during flexion above 90 degrees: the ulnar nerve (arrows) was dislocated above the surface of the medial epicondyle. (c)—Significant nerve swelling, mainly at the level of the sulcus; no stenosis was visualized at any of the levels.
2.2. Snapping Triceps with Ulnar Neuritis
Snapping triceps as a cause of ulnar neuritis Although it is rarely diagnosed, snapping triceps can also cause ulnar neuritis [56][18]. It affects men primarily in the fourth decade of life. Dynamic US examination is a method of choice because it allows differentiation between the snapping of the muscle and the ulnar nerve (Figure 102) [57][19]. The muscle may dislocate both medially and laterally. The treatment for the snapping triceps syndrome is primarily conservative and involves avoiding activities that provoke symptoms.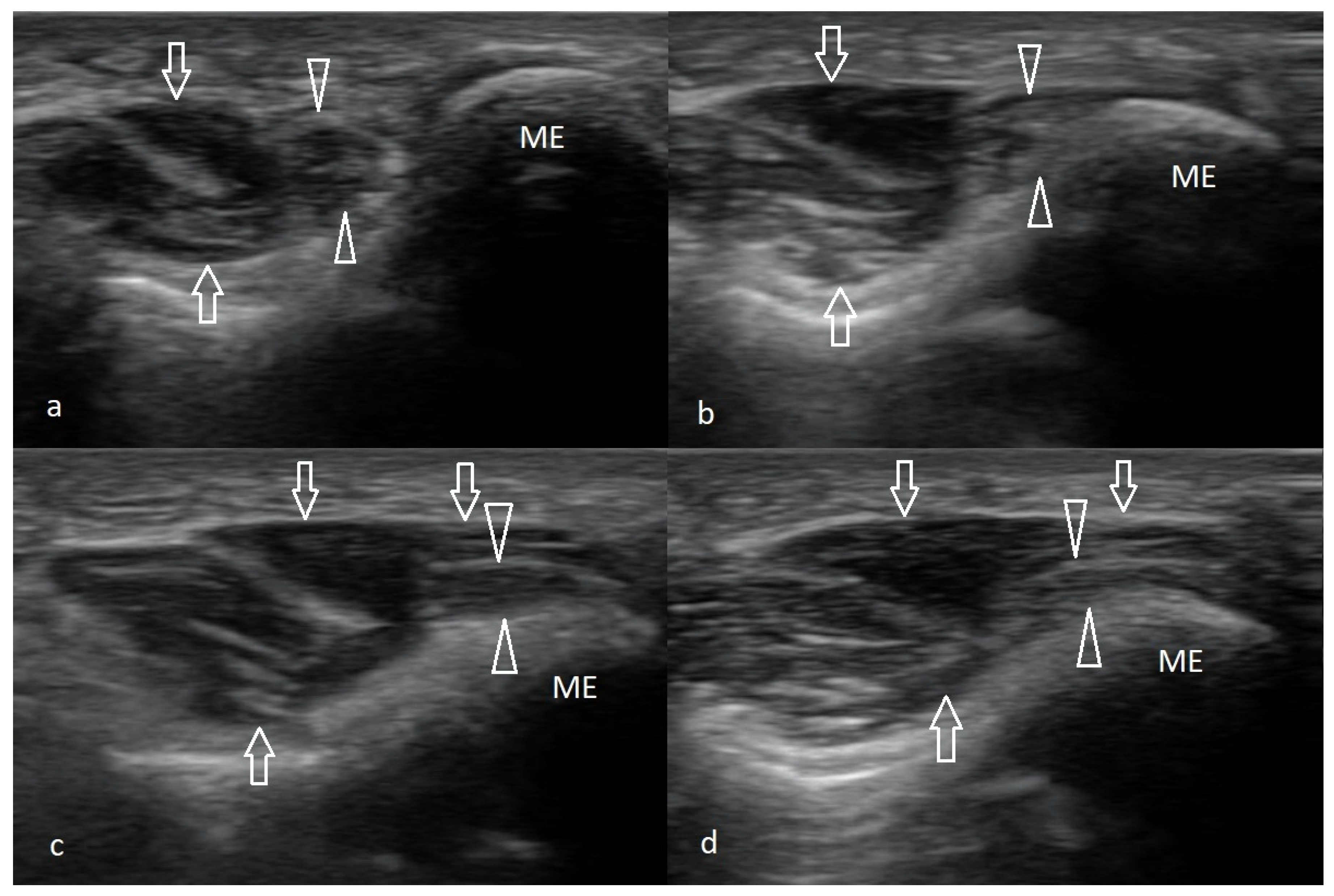
Figure 102. Snapping triceps syndrome. A series demonstrating the anterior dislocation of the medial head of triceps muscle over the surface of the medial epicondyle, which is accompanied by shifting the ulnar nerve beyond the sulcus and its compression; compression increases as the degree of flexion increases. (a)—Examination in full extension, (b)—90, (c)—100, and (d)—120 degrees of flexion; arrows—medial head of triceps muscle; arrowheads—ulnar nerve.
2.3. Ulnar Nerve Compression Caused by Anconeus Epitrochlearis
Another rare cause of ulnar neuritis is the presence of an anomalous muscle, anconeus epitrochlearis (AE). Cadavers and imaging studies found it in 3–34% of subjects [58,59,60][20][21][22]. Nonetheless, this accessory muscle in patients undergoing surgery for cubital tunnel syndrome might be as high as 20% [61][23]. Typically, patients with AE muscle and ulnar neuritis develop symptoms more rapidly and early in life; forearm movements might sometimes provoke the symptoms.2.4. Ulnar Collateral Ligament Injury
Injury to the medial collateral ligament (MCL) occurs mainly in athletes who throw overhead because the anterior part of the MCL is the primary restraint to valgus stress during overhead throwing. The disorder leads to valgus elbow instability and pop sensation over the medial elbow [5,62,63][5][24][25]. The most crucial test for MCL injury is ‘the valgus stress test’, also known as ‘the elbow abduction stress test’, which involves palpation of the medial joint line of both the symptomatic elbow and the contralateral side and comparing them for signs of laxity or instability against valgus forces. Valgus stress should be applied against an elbow flexed 20–30°, and then, the amount of opening and the subjective quality of the endpoint is assessed. The test is positive when a firm endpoint is absent, joint space opens more than 3 mm, or the patient feels pain [21,51][11][26]. MCL injury may also be confirmed with a positive result on the moving valgus stress test or milking maneuver [5,36][5][27]. An US picture of MCL is presented in Figure 83.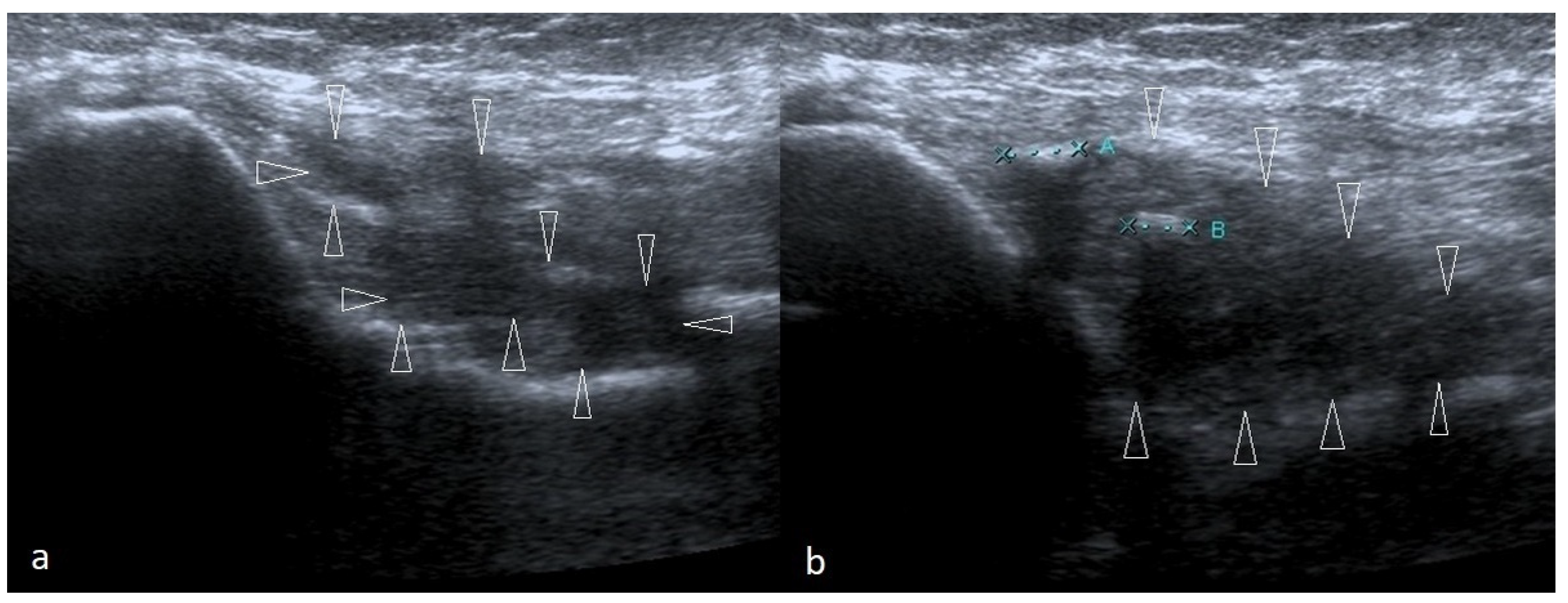 Figure 3. Two cases of post-traumatic changes within the medial collateral ligament and profound part of the common flexor tendon. In both pictures (a,b), the areas of hypoechoic scarring are marked with arrowheads; post-traumatic calcifications are also visible.
Figure 3. Two cases of post-traumatic changes within the medial collateral ligament and profound part of the common flexor tendon. In both pictures (a,b), the areas of hypoechoic scarring are marked with arrowheads; post-traumatic calcifications are also visible.
2.5. Cervical Radiculopathy
Patients with neurologic disorders should also be examined for cervical radiculopathy and dysfunction of a nerve root of the cervical spine. The C7 and C6 cervical nerve roots are the most affected. The typical symptoms of cervical radiculopathy are neck and arm discomfort of insidious onset and sensory changes along the involved nerve root dermatome, including tingling, numbness, or sensorineural loss [64][28]. Confirming cervical radiculopathy may be possible with the foraminal compression test (or Spurling test). It is performed by applying downward pressure on a patient’s head, with the neck extended and the head rotated. The test is positive if the pain radiates into the ipsilateral limb. As C6 and C7 radiculopathy lead to muscle weakness, it may predispose to ME development [64,65][28][29]. An imaging modality of choice for confirmation of cervical radiculopathy is MRI.2.6. Ganglion Cyst
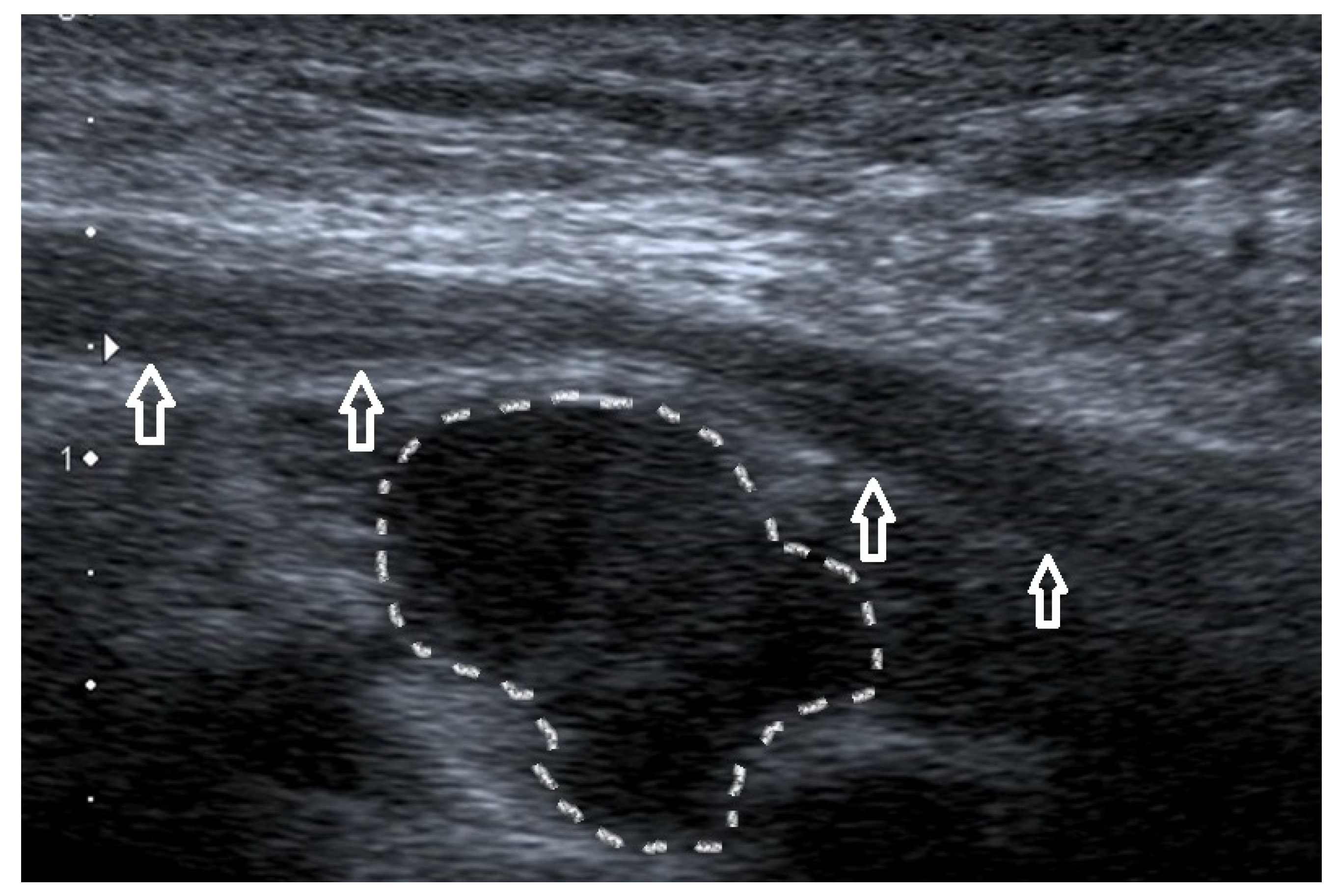
Another cause of elbow pain may be a ganglion cyst, a benign form of soft tissue swelling. It typically arises from the ulnohumeral joint capsule. The etiology of ganglia remains unclear, but degenerative changes at the collective and repeated minor trauma seem to contribute to its development [66][30]. An improper diagnosis is likely because the ganglion may mimic epicondylalgia or cubital tunnel syndrome. US evaluation (Figure 114) or magnetic resonance imaging (MRI) may be particularly helpful in the proper assessment of pain sources [67,68,69][31][32][33].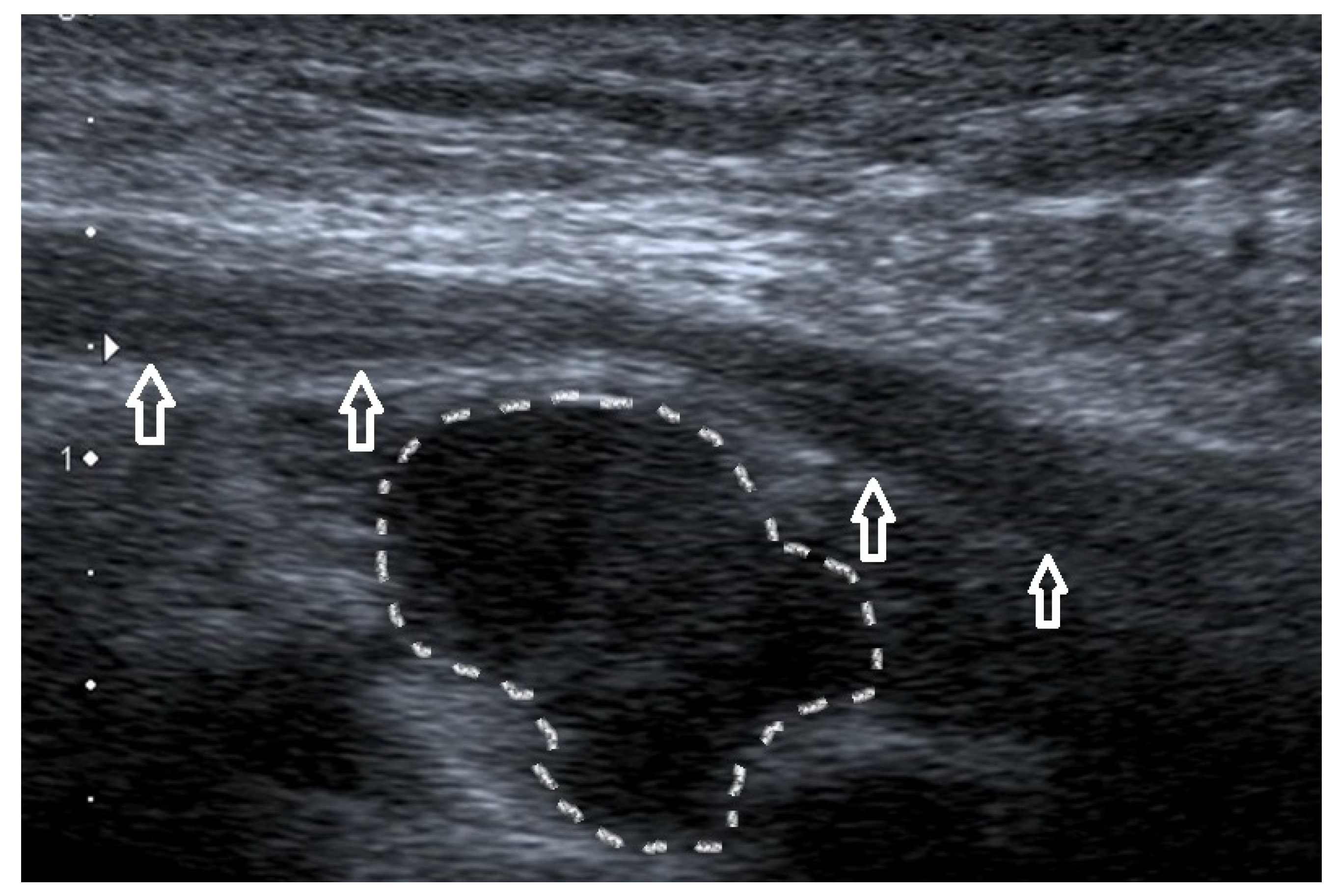
Figure 114.
Ganglion cysts (dotted line) compressing the ulnar nerve (arrows).
2.7. Degenerative Changes in the Elbow Joint
Osteoarthritis and degenerative changes in the elbow joint might cause elbow pain and stiffness, especially in elderly subjects [70][34]. The most common cause of elbow arthritis is rheumatoid arthritis, followed by trauma-related arthritis and primary osteoarthritis [71][35]. Nonetheless, it seems unlikely that such changes will be highly localized to affect only the medial side of the elbow without changes in other joints. US dynamic examination might help determine if osteophytes and loose bodies are a source of irritation and pain and exclude inflammatory activity that might suggest a rheumatic background of the patient’s ailments.2.8. Epitrochlear Lymphadenopathies
Lymphadenopathy of the elbow region is likely to signify a systemic illness. Usually, they accompany the disorders that cause general lymphadenopathy (including lymphomas, leukemias), infections (Epstein–Barr virus, human immunodeficiency virus, cat-scratch disease, syphilis), and malignancies [72,73,74][36][37][38]. Patients with enlarged lymph nodes in the epitrochlear region should be carefully evaluated in the light of clinical data, such as the presence of fever and other systemic symptoms, mobility of enlarged nodes concerning skin and deeper layers, and changes in the overlying skin [73][37]. It is advisable to screen such patients for red flags indicative of malignant disease and refer them for further testing to exclude such pathology [73][37].References
- Morrey, B.F. (Ed.) The Elbow and Its Disorders, 3rd ed.; WB Saunders: Philadelphia, PA, USA, 2000.
- Matthews, J.; Boyle, K. Tennis and Golfer’s Elbow: Epicondylitis. In Orthopedic Surgery Clerkship; Eltorai, A.E.M., Eberson, C.P., Daniels, A.H., Eds.; Springer International Publishing: Cham, Germany, 2017; pp. 87–90.
- Morris, H. The rider’s sprain. Lancet 1882, 120, 133–134.
- Hultman, K.L.; Goldman, B.H.; Nazarian, L.N.; Ciccotti, M.G. Ultrasound Examination Techniques for Elbow Injuries in Overhead Athletes. J. Am. Acad. Orthop. Surg. 2021, 29, 227–234.
- Kane, S.F.; Lynch, J.H.; Taylor, J.C. Evaluation of elbow pain in adults. Am. Fam. Physician 2014, 89, 649–657.
- Barret, H.; Gastaud, O.; Laumonerie, P.; Faruch, M.; Bonnevialle, N.; Mansat, P.; Langlais, T. Feasibility and technique of ultrasound traumatic elbow lesion assessment. Orthop. Traumatol. Surg. Res. 2021, 107, 102836.
- Jeong, J.S. Dual-element transducer with phase-inversion for wide depth of field in high-frequency ultrasound imaging. Sensors 2014, 14, 14278–14288.
- Jäschke, M.; Weber, M.A. Sonographie des Ellenbogens—Standardschnitte und Normalanatomie . Radiologe 2018, 58, 985–990.
- Entrekin, R.R.; Porter, B.A.; Sillesen, H.H.; Wong, A.D.; Cooperberg, P.L.; Fix, C.H. Real-time spatial compound imaging: Application to breast, vascular, and musculoskeletal ultrasound. Semin. Ultrasound. CT MR 2001, 22, 50–64.
- Barco, R.; Antuña, S.A. Medial elbow pain. EFORT Open Rev. 2017, 2, 362–371.
- Taylor, S.A.; Hannafin, J.A. Evaluation and management of elbow tendinopathy. Sports Health 2012, 4, 384–393.
- Cutts, S. Cubital tunnel syndrome. Postgrad. Med. J. 2007, 83, 28–31.
- Amin, N.H.; Kumar, N.S.; Schickendantz, M.S. Medial epicondylitis: Evaluation and management. J. Am. Acad. Orthop. Surg. 2015, 23, 348–355.
- Ciccotti, M.G.; Ramani, M.N. Medial epicondylitis. Tech. Hand Up Extrem. Surg. 2003, 7, 190–196.
- Andrews, K.; Rowland, A.; Pranjal, A.; Ebraheim, N. Cubital tunnel syndrome: Anatomy, clinical presentation, and management. J. Orthop. 2018, 15, 832–836, Correction in J. Orthop. 2020, 23, 275.
- Bordes, S.J.; Jenkins, S., Jr.; Bang, K.; Turgut, M.; Iwanaga, J.; Loukas, M.; Spinner, R.J.; Dumont, A.S.; Tubbs, R.S. Ulnar nerve subluxation and dislocation: A review of the literature. Neurosurg. Rev. 2021, 44, 793–798.
- Tsukada, K.; Yasui, Y.; Sasahara, J.; Okawa, Y.; Nakagawa, T.; Kawano, H.; Miyamoto, W. Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes. J. Clin. Med. 2021, 10, 3131.
- Rioux-Forker, D.; Bridgeman, J.; Brogan, D.M. Snapping Triceps Syndrome. J. Hand Surg. Am. 2018, 43, 90.e1–90.e5.
- Shuttlewood, K.; Beazley, J.; Smith, C.D. Distal triceps injuries (including snapping triceps): A systematic review of the literature. World J. Orthop. 2017, 8, 507–513.
- Chalmers, J. Unusual causes of peripheral nerve compression. Hand 1978, 10, 168–175.
- Husarik, D.B.; Saupe, N.; Pfirrmann, C.W.; Jost, B.; Hodler, J.; Zanetti, M. Elbow nerves: MR findings in 60 asymptomatic subjects—normal anatomy, variants, and pitfalls. Radiology 2009, 252, 148–156.
- Masear, V.R.; Hill, J.J., Jr.; Cohen, S.M. Ulnar compression neuropathy secondary to the anconeus epitrochlearis muscle. J. Hand Surg. Am. 1988, 13, 720–724.
- Maslow, J.I.; Johnson, D.J.; Block, J.J.; Lee, D.H.; Desai, M.J. Prevalence and Clinical Manifestations of the Anconeus Epitrochlearis and Cubital Tunnel Syndrome. Hand 2020, 15, 69–74.
- Freehill, M.T.; Safran, M.R. Diagnosis and management of ulnar collateral ligament injuries in throwers. Curr. Sports Med. Rep. 2011, 10, 271–278.
- Zaremski, J.L.; Vincent, K.R.; Vincent, H.K. Elbow Ulnar Collateral Ligament: Injury, Treatment Options, and Recovery in Overhead Throwing Athletes. Curr. Sports Med. Rep. 2019, 18, 338–345.
- Erdem, Y.; Neyisci, C. Lateral and Medial Epicondylitis: Definition, Diagnosis, Screening and Treatment Algorithms, Work-Related Musculoskeletal Disorders; IntechOpen: Ankara, Turkey, 2019.
- Zwerus, E.L.; Somford, M.P.; Maissan, F.; Heisen, J.; Eygendaal, D.; van den Bekerom, M.P. Physical examination of the elbow, what is the evidence? A systematic literature review. Br. J. Sports Med. 2018, 52, 1253–1260.
- Lee, A.T.; Lee-Robinson, A.L. The prevalence of medial epicondylitis among patients with c6 and c7 radiculopathy. Sports Health 2010, 2, 334–336.
- Polston, D.W. Cervical radiculopathy. Neurol. Clin. 2007, 25, 373–385.
- Vaishya, R.; Kapoor, C.; Agarwal, A.K.; Vijay, V. A Rare Presentation of Ganglion Cyst of the Elbow. Cureus 2016, 8, e665.
- Chim, H.; Yam, A.K.; Teoh, L.C. Elbow ganglion arising from medial epicondyle pseudarthrosis. Hand Surg. 2007, 12, 155–158.
- Kuboi, T.; Tajika, T.; Endo, F.; Hatori, Y.; Saida, R.; Chikuda, H. Cubital tunnel syndrome with small occult ganglion: A case report of bike rider. SAGE Open Med. Case Rep. 2020, 8, 2050313X20972850.
- Lee, S.W.; Kim, S.G.; Oh-Park, M. Ganglion cyst of radiocapitellar joint mimicking lateral epicondylitis: Role of ultrasonography. Am. J. Phys. Med. Rehabil. 2013, 92, 459–460.
- Kokkalis, Z.T.; Schmidt, C.C.; Sotereanos, D.G. Elbow arthritis: Current concepts. J Hand Surg. Am. 2009, 34, 761–768.
- Soojian, M.G.; Kwon, Y.W. Elbow arthritis. Bull NYU Hosp. Jt. Dis. 2007, 65, 61–71.
- Catalano, O.; Nunziata, A.; Saturnino, P.P.; Siani, A. Epitrochlear lymph nodes: Anatomy, clinical aspects, and sonography features. Pictorial essay. J. Ultrasound 2010, 13, 168–174.
- Pannu, A.K.; Prakash, G.; Jandial, A.; Kopp, C.R.; Kumari, S. Epitrochlear lymphadenopathy. Korean J. Intern. Med. 2019, 34, 1396.
- Selby, C.D.; Marcus, H.S.; Toghill, P.J. Enlarged epitrochlear lymph nodes: An old physical sign revisited. J. R. Coll. Physicians Lond. 1992, 26, 159–161.
More
