Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 1 by Bárbara Costa.
Dostarlimab (JEMPERLI) is a PD-1 monoclonal antibody for the treatment of adult patients, with mismatch repair deficient (dMMR), recurrent or advanced endometrial cancer that has progressed on or following prior therapy with a platinum-containing regimen. As determined by an FDA-approved test this indication was granted rapid approval based on the rate of tumor response and the duration of the response. Continued approval for this indication is conditioned on further confirmatory trials demonstrating and documenting clinical benefit.
- anti-PD-1 antibody
- dostarlimab
- immunotherapy
1. Introduction
In 1986, the first immunotherapy agent, an antitumor cytokine designated interferon-alpha 2 was approved by the US Food and Drug Administration (FDA). IFN-a2 was first approved for the treatment of hairy cell leukemia (HCL) after studies showed that it had a high response rate in patients with advanced HCL. In 1995, the FDA approved IFN-a2 for use as adjuvant therapy for stage IIB/III melanoma. When it was licensed for the treatment of metastatic melanoma and renal cell carcinoma in 1998, interleukin-2 (IL-2), a T-cell growth factor that aids in immunological modulation and T-cell proliferation, became the second anticancer cytokine approved by the FDA. Since the development of immunotherapies a promise of revolutionizing the standard care in cancer treatment has existed and, in recent years, a novel class of immunotherapeutics known as checkpoint inhibitors has emerged as a cornerstone in cancer treatment [1]. To this day, different types of immunotherapies are used to treat cancer: immune checkpoint inhibitors, T-cell transfer therapy, monoclonal antibodies, vaccines, and immune system modulators.
Notably, a record number of antibody therapeutics have been granted approval in either the European Union (EU) or the United States (US). In diseases such as cancer, immunotherapies have drastically changed the game for patients, since immunotherapies get the immune system properly engaged to eradicate cancer cells. For example, the use of programmed cell death protein-1 (PD-1) and the cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) has been demonstrating increased median overall survival and durable responses in patients across multiple tumors. Thousands of people have benefited from immune checkpoint inhibitors (ICPIs); however, despite long-lasting responses in a variety of tumor types, most patients either do not respond at all or develop resistance to the ICPI. Additionally, ICPI treatment has the potential to cause major side effects, and therefore identification of patient populations that will benefit from ICPI as single medicines and in combination is urgently needed [2].
Regarding activated T cells, PD-1 is an inhibitory immunological checkpoint receptor. PD-1 reduces activated effector T-cell capabilities such as proliferation, cytokine generation, and cytotoxic activity by interacting with its ligands, programmed cell death ligands 1 and 2 (PD-L1 and PD-L2). One of the strategies through which tumor cells elude the immune system and interfere with cancer-specific immune responses is the upregulation of PD-L1. Preclinical and clinical investigations have shown that treatments that bind to either the PD-1 receptor or ligand and effectively disrupt the receptor–ligand interaction can boost antitumor immunity and improve patient survival in a range of malignancies [3]. So far, the FDA has approved six PD-1 and PD-L1 inhibitors for clinical usage, collectively known as PD-L1. Patients with cancer can choose from a variety of dose regimens, disease-specific treatments, tolerance profiles, and pricing alternatives due to the competitive environment of anti-PD-1 antibodies.
On 17 August 2021, the FDA granted accelerated approval to Dostarlimab, a monoclonal antibody, for adults with dMMR recurrent or advanced endometrial cancer that has progressed despite ongoing or prior treatment with the platinum-containing chemotherapy regimen, Figure 1.
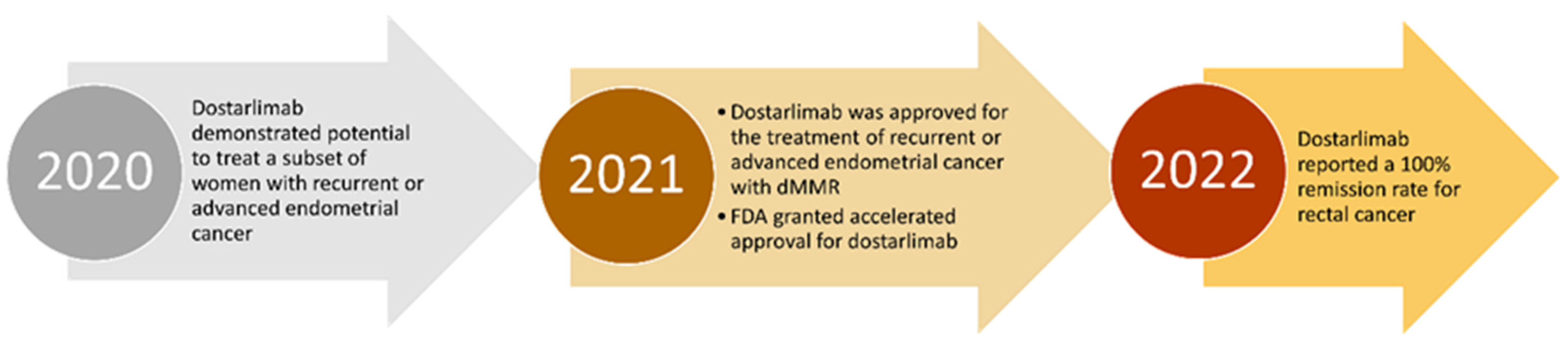
Figure 1. Timeline of the drug Dostarlimab since the demonstrated potential to treat a subset of women with EC to the reported 100% remission rate in rectal cancer.
1.1. About the Drug
Dostarlimab (also referred to as TSR-042 or Jemperli, commercial name) is a humanized mAb of the IgG4 isotype, produced by recombinant DNA technology in mammalian Chinese hamster ovary (CHO) cells that binds PD-1 on T cells and blocks interactions with its ligands PD-L1 and PD-L2, activating immune responses. Dostarlimab is an immunotherapy that aids the body’s natural anti-tumor immune response during cancer treatment. It is given via intravenous infusion for over 30 min every three to six weeks, depending on the cycle.
To prevent the formation of half-antibodies, each heavy chain of the antibody has a serine to proline substitution (S228P) to promote the stabilization of disulfide bonds between the two heavy chains. Dostarlimab was humanized by grafting the heavy- and light-chain complementarity-determining regions on the germline variable region frameworks of their nearest CONTACT human species orthologs, followed by affinity maturation via mammalian cell display and somatic hypermutation, using the AnaptysBio SHM-XEL system. The company Anaptysbio developed the drug Dostarlimab, also in collaboration with Tesaro, and was bought by GlaxoSmithKline in 2019 [5,6][4][5]. The JemperliTM final product is a concentrate for infusion solution containing 500 mg of dostarlimab as the active ingredient. Trisodium citrate dihydrate, citric acid monohydrate, L-arginine hydrochloride, sodium chloride, polysorbate 80, and water for injection are among the other constituents.
Although the heavy chain of Dostarlimab is involved in the interaction between PD-1 and Dostarlimab, the light chain is predominantly responsible for steric blockage of PD-L1 binding. To attain high affinity, Dostarlimab causes conformational rearrangements in the BC, C’D, and FG loops of PD-1. By occupying the concave surface on the heavy chain via numerous interactions, the residue R86 within the C’D loop of PD-1 plays a vital role in Dostarlimab binding. This high-resolution structure could be useful in developing better anti-PD-1 biologics or effective cancer immunotherapy combination methods [7][6]. Dostarlimab has a KD value of 0.3 nM for human PD-1, with an association rate of 5.7105 (M−1s−1) and a dissociation rate of 1.7 104 (s−1), indicating fast target association and delayed dissociation [5][4]. Since IgG4 isotypes elicit modest Fc-mediated effector functions such as antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC), Dostarlimab was designed to avoid tumor-reactive T cell depletion. Fc binding has been used to illustrate the lack of Dostarlimab ADCC activity (in a Biacore analysis).
The structural basis is still unrevealed, but it is known that an epitope within a target molecule might be a critical component of a therapeutic antibody since antibodies that recognize different epitopes have varying therapeutic efficacy. Even though that antibodies against PD-1 and PD-L1 have a similar blocking function, they identify different antigenic epitopes. Because of their high specificity and affinity for their targets, monoclonal antibodies have been a key therapeutic method for decades. The high-resolution structure revealed that Dostarlimab binds to the flexible loops of PD-1, including the BC, C’D, and FG loops, differently than Pembrolizumab or Nivolumab [7][6].
Dostarlimab has an anti-drug antibodies (ADA) rate of 2.5%, which, again, is comparable to other anti-PD-L1 medicines, and it only induces a modest immune response in a limited fraction of cancer patients after one or more treatment cycles. Dostarlimab’s high product purity and mode of administration reduces the danger of inducing immunological reactions. Furthermore, there is currently no evidence that pre-existing ADAs or the generation of ADAs has any effect on any safety or efficacy measurements. These findings suggest that Dostarlimab is a novel and effective anti-PD-1 monoclonal antibody with a low risk of eliciting immunogenic reactions [9][7]. Data from the GARNET trial support reports that dMMR/MSI-H is a predictive biomarker of response to anti-PD-L1 agents; however, Dostarlimab has shown clinical activity in endometrial cancer (EC) and nonsmall cell lung cancer (NSCLC) regardless of MMR status, with a tolerability profile similar to other anti-PD-1 mAbs across tumor types.
1.2. Effect on T-Cell Activation
Dostarlimab was found to improve T-cell activation in a variety of in vitro functional test methods using primary human T cells. While Dostarlimab improved T-cell activation in antigen-dependent systems, it had no direct (nonspecific) effects on T-cell responses, as seen by the lack of cytokine production in the absence of antigen. Dostarlimab was found to have effective anticancer action in humanized mice tumor models, as well as a consistent pharmacokinetic and pharmacodynamic profile with negligible off-target effects. Its anticancer effectiveness was linked to a decrease in tumor-associated regulatory T cells and an increase in tumor-infiltrating CD8+ T cells [10][8]. For example, dostarlimab treatment in vitro decreased tumor growth in the MDA-MB-436 breast cancer model (TGI of 53%) when compared to isotype control [5][4]. Dostarlimab’s anti-PD-1 antibody profile was shown to be good in preclinical testing, with effective binding to PD-1 and antagonizing interactions with PD-L1 and PD-L2. Dostarlimab binds to the human PD-1 receptor with a high affinity, with a binding affinity (KD) of 300 pM. Preclinical findings for the previous approved PD-1 treatments such as Nivolumab, Pembrolizumab, and Cemiplimab have a similar binding profile. Dostarlimab was chosen for its IgG4 isotype to generate the most dependable and efficacious therapy. Other anti-PD-1 antibodies (Pembrolizumab, Nivolumab, and Cemiplimab) are all IgG4 modalities, but anti-PD-L1 antibodies (Atezolizumab, Avelumab, and Durvalumab) are all IgG1 modalities (added risk is a possibility in the chronic administration of IgG1 Fc for immunological enhancement). According to surface plasmon resonance, flow cytometry employing cell lines overexpressing recombinant PD-1, or binding to the native protein on peripheral blood mononuclear cells, Dostarlimab bound to both human and cynomolgus monkey PD-1 with great affinity [11][9]. The antibody also prevented PD-L1 and PD-L2 from interacting with the receptor. In a human CD4+ mixed lymphocyte response assay, Dostarlimab, acted as a powerful functional antagonist, resulting in enhanced IL-2 production. In this test, the addition of anti-TIM3 or anti-LAG3 antibodies increased the activity of Dostarlimab. Dostarlimab incubation of human peripheral blood mononuclear cells (PBMCs) as a single agent did not result in significant cytokine release stimulation. Interfering with the PD-1/PD-L1 pathway removes an essential immune system inhibitory response, which can lead to severe or fatal immune-mediated adverse effects. These reactions can occur in any organ system and at any time after starting therapy; while they are most common during therapy, they can also occur after the causative substance is stopped. Patients on Dostarlimab should be closely monitored for signs of an underlying immune-mediated reaction, and if one is suspected, they should be assessed and treated immediately. It is important to remember that anti-PD-L1 therapies are associated with a multitude of side effects, including pneumonitis, hypothyroidism, colitis, and infusion-site responses. Although enhancing the immune system’s activation state is an effective anticancer strategy these events are most likely connected to the target’s binding and associated pharmacodynamic consequences, such as anti-PD-L1 treatments’ immune-related side events. The cytotoxicity caused by the antibody’s binding to complement, or FC receptors is another important factor in predicting the safety profile of a new anti-PD-(L)1 treatment. Dostarlimab demonstrated little to no binding to Fc or a complement protein C1q, receptors that induce ADCC, and CDC, respectively, and so is unlikely to result in the depletion of antitumor effector T cells, which is consistent with its IgG4 framework. The preclinical data supported Dostarlimab first-in-human dose selection and showed that the drug had a sufficient safety margin to be examined further in the Phase 1 GARNET trial’s human dose-finding sections 1 and 2A. Dostarlimab has shown significant and sustained responses in ongoing clinical studies, as well as a manageable safety profile with side effects like those seen with other anti-PD-1 treatments. No dose-limiting toxicity was observed. Dostarlimab has shown potential as an anti-PD-1 therapy in different clinical studies, including RUBY (NCT03981796), FIRST (NCT03602859), IOLite (NCT03307785), and MOONSTONE (NCT03307785), and several more, where it is being tested either as a monotherapy and in combination for a variety of tumor types (NCT03955471) [12][10].1.3. Pharmacodynamics and Pharmacokinetics
A population PK (PopPk) profile of Dostarlimab was well described by a 2-compartment model with time-dependent linear elimination. At clinically relevant doses, the PopPK model revealed that Dostarlimab exposure is approximately dose-proportional. The PK profile of Dostarlimab is generally consistent with that of other approved PD-1 inhibitors, Pembrolizumab, Nivolumab, and Cemiplimab because PK parameters were similar, and both time-varying CL and a linear elimination pattern were previously observed for these agents within their therapeutic dose range. While Dostarlimab’s time-varying CL is similar to other PD-1 inhibitor observations, the typical maximum drop in CL over time was calculated at 14.9%, which is lower than that reported for Pembrolizumab (20–30%), Nivolumab (25%), or Cemiplimab (35.9%). Interestingly, in stepwise covariate modeling, tumor type (EC (dMMR/MSI-H), NSCLC or MSI-H, etc.) was not determined to be a statistically significant covariate and did not affect Dostarlimab PK characteristics. Body weight and time-varying albumin were observed to influence Dostarlimab PK, as previously reported for other PD-1 inhibitors. The impact of body weight on exposure was considered not clinically relevant. For short, patient covariates/disease characteristics had limited clinically relevant effects on exposure. Dostarlimab has a pharmacokinetics (PK) profile that permits the dosing interval to be increased from three to six weeks. The pharmacodynamic activity of Dostarlimab was conducted in both in vitro and in vivo experimental systems. Throughout the first cycle 500 mg was administered intravenously every 3 weeks, and the absorption was described by: the mean Cmax and AUC0-tau of dostarlimab as 171 mcg/mL and 35,730 mcg.h/mL, respectively. When administered at 1000 mg every 6 weeks, the mean Cmax and AUC0-tau are 309 mcg/mL and 95,820 mcg.h/mL, respectively. At steady state, the mean volume of distribution of Dostarlimab is 5.3 L. The metabolism of Dostarlimab has yet to be characterized, but for now it is estimated to be degraded via catabolic pathways into smaller peptides and amino acids [13][11]. The mean terminal elimination half-life of Dostarlimab is 25.4 days, and the mean clearance of Dostarlimab is 0.007 L/h. There are no data regarding overdose with Dostarlimab. Symptoms of overdosage are likely to be consistent with the adverse effect profile of Dostarlimab and may therefore involve significant immune-mediated reactions [14,15][12][13].2. Immune Microenvironment and Emerging Treatments
T cells, B cells, natural killer cells, and other tumor-infiltrating lymphocytes express PD-1, a transmembrane receptor. Antigen-presenting cells (APCs) and certain nonimmune cells, particularly tumor cells, express PD-L1 and PD-L2. The immunological inhibitory checkpoint PD-1 and its ligands are involved in T-cell activation and tolerance [19][14]. The binding of PD-L1 or PD-L2 to PD-1 prevents lymphocyte activation and improves immunological tolerance to self-antigens to prevent tissue injury, but it also prevents immune cells from responding to tumors. Tumors have been demonstrated to use the PD-1 signaling pathway to elude immune regulation and enhance tumor growth by upregulating PD-L1 expression. Even though mAbs have proven to be highly effective immuno-oncology therapy agents in clinical trials, there are still obstacles to their general usage in all patients, such as the rise of immunogenicity. ADAs often have no overall clinically relevant effects, although they can affect pharmacokinetics and have an impact on safety or efficacy. Patient-related factors (e.g., human leukocyte antigen type, disease, concomitant drugs, and immunological competence), dosing regimen, method of administration, and essential product factors all have a role in the development of ADAs [20][15]. Moreover, infusion reactions, hypersensitivity reactions, anaphylaxis, and ADA-mediated diseases are all examples of how ADAs can reduce efficacy by altering drug clearance. They can also have an impact on drug safety through infusion reactions, hypersensitivity reactions, anaphylaxis, and ADA-mediated diseases. Neutralizing antibodies (NAbs), another form of ADA, diminish efficacy by disrupting target binding. Even though the humanization of antibodies reduces the risk of antidrug immunological reactions, immunogenic responses are nevertheless seen in both partially and fully humanized antibodies [21][16]. Pembrolizumab, Nivolumab, Cemiplimab, Atezolizumab, Avelumab, and Durvalumab are mAbs that disrupt the interaction of PD-1/PD-L1 and thereby eliminate cancers’ ability to evade the immune system [9][7]. Nivolumab (OPDIVO®) and Pembrolizumab (KEYTRUDA®) were approved by the US FDA in 2014 for the treatment of melanoma and nonsmall cell lung cancer. Since then, the antibodies’ indications have been expanded to include renal cell carcinoma, classical Hodgkin lymphoma, squamous cell carcinoma of the head and neck, urothelial carcinoma, esophageal carcinoma, endometrial cancer, squamous cell carcinoma, hepatocellular carcinoma, and breast cancer, either as monotherapy or in combination with other drugs. These drugs are also indicated for dMMR/MSI-H testing. Dostarlimab, the fourth PD-1 monoclonal antibody, was approved in 2021 [7][6]. Scientific advancements have facilitated the development of mAb therapeutics that entered clinical trials and were granted marketing approvals. In 2019, GSK anticipated potential regulatory submissions for Dostarlimab, after the results of Phase I dose-escalation and cohort expansion study (GARNET; NCT02715284). This study evaluated the safety and efficacy of Dostarlimab monotherapy for patients with advanced solid tumors, including women with recurrent or advanced endometrial cancer who progressed on or after a platinum-based regimen. Patients were administered 500 mg every 3 weeks for the first 4 cycles, and 1000 mg every 6 weeks. Of the 25 patients with microsatellite instability in endometrial cancer, one had a complete response and 12 had partial responses. The objective response rate was 43.5% in this group of 108 patients, according to RECIST v1.1 (47/108; 95% confidence interval: 34.0–53.4), with 10.2% complete responses (CRs) (11/108) and 33% partial responses (36/108). Furthermore, 89.4% of respondents had an active answer at the time of data cut-off [22][17]. Early-stage clinical studies, as well as two Phase 3 studies, RUBY and FIRST, are evaluating Dostarlimab as a treatment for several forms of cancer. The Phase 3 RUBY study (NCT03981796) is a 2-part study. Part 1 is to evaluate the efficacy and safety of Dostarlimab plus carboplatin-paclitaxel followed by Dostarlimab versus placebo plus Carboplatin-Paclitaxel followed by placebo. Part 2 is to evaluate the efficacy and safety of Dostarlimab plus Carboplatin-Paclitaxel followed by Dostarlimab plus Niraparib versus placebo plus Carboplatin-Paclitaxel followed by placebo in participants with recurrent or primary advanced (Stage III or IV) endometrial cancer. TSR-042 is also being tested in a Phase 3 FIRST trial (NCT03602859), which compares platinum-based therapy with TSR-042 and Niraparib to the standard of care platinum-based therapy as first-line treatment of Stage III or IV non-mucinous epithelial ovarian cancer [8][18]. The EMA approved the conditional marketing authorization since Jemperli answers an unmet medical need and the benefit of immediate availability outweighed the risk of less comprehensive data than is generally necessary. In 2021, either the US or the EU granted accelerated approvals to 11 antibody therapeutics. The FDA granted accelerated approval to five of the seven products, Dostarlimab, Loncastuximab Tesirine, Amivantamab, Aducanumab, and Tisotumab vedotin. Jemperli received an additional accelerated approval from the FDA on 17 August 2021, for the treatment of adult patients with dMMR recurrent or advanced solid tumors, as determined by an FDA-approved test, that have progressed on or following prior treatment and who have no satisfactory alternative treatment options. This approval was based on the tumor response rate and the response’s duration. The increased number and variety of antibody therapies that may be approved soon will almost certainly have a significant impact on patient care. This is particularly true for cancer patients, who may soon have access to a significantly higher number of antibody immune checkpoint modulators and antibody–drug conjugates.2.1. Inhibitors of PD-1/PD-L1 and dMMR
Inhibitors of PD-1/PD-L1 and dMMR
Cancer immuno-therapy has seen significant clinical success driven by ICBs that restore T-cell activation. ICBs act in multiple ways to alter T-cell function, including the downregulation of inhibitory signaling [14][12]. One target of ICBs is programmed cell death protein 1 (PD-1). Multiple malignancies have high levels of PD-L1 and PD-L2, which suppress T cells. Monoclonal antibodies that target PD-1 or PD-L1 (PD-(L)1) disrupt the interaction between PD-1 on T cells and PD-L1 on cancer cells, restoring T-cell activity. The PD-L1 inhibitor has been licensed as an immunotherapeutic for a variety of malignancies [23][19]. Anti–PD-(L)1 pathway-targeted treatments have been demonstrated to be well tolerated and have consistent safety profiles as a pharmacological class, and when used to treat dMMR-MSI-H, PD-1/PD-L1 inhibitors showed favorable clinical results, including a higher response rate. However, not all drugs entitled of PD-1/PD-L1 inhibitors have the same success rate in treating tumors with dMMR. In Sclafani’s papereview, it is highlighted that the administration of Pembrolizumab to patients with dMMR metastatic colorectal cancer was correlated with a poor prognosis. Numerous studies have demonstrated the wide range of immunotherapy, prognosis, and chemotherapy sensitivity in individuals with dMMR/MSI malignancies, and the detection limitation contributes to the difficulty of treatment. Moreover, it is necessary to quantify the frequency of missmatch repairs. A lower or higher frequency will require a different treatment. However, it remains unclear how the same PD-1/PD-L1 inhibitors (or even different ones) cause variable therapeutic responses in patients with a different frequency of mismatch repairs [24][20]. At last, it appears Dostarlimab that shows durable antitumor activity in patients with dMMR/MSI-H.3. Conclusions
In MMR-deficient instances, Dostarlimab has demonstrated promising benefits, and the combination of Pembrolizumab and Lenvatinib is quickly becoming the standard of therapy for pre-treated recurrent MMR-proficient EC. However, further research is needed to understand the primary and secondary mechanisms of immunotherapy resistance, as well as to use ICI in the first-line metastatic context and early-stage malignancies. The same applies to rectal cancer. Future clinical trials should go through safety studies to identify higher-risk categories. Treatments such as Dostarlimab should become widely available, as well as access to a medical team who will help monitor patients like in the trial NCT04165772 and intervene if the tumor comes back. The future of cancer treatment is an approach based on cancer type and subtype, and such a dramatic response as seen with Dostarlimab in patients with rectal cancer gives hope that we are on the right track to find a dramatic match for the remaining cancers.References
- Eno, J. Immunotherapy Through the Years. J. Adv. Pract. Oncol. 2017, 8, 747.
- Gjoerup, O.; Brown, C.A.; Ross, J.S.; Huang, R.S.P.; Schrock, A.; Creeden, J.; Fabrizio, D.; Tolba, K. Identification and Utilization of Biomarkers to Predict Response to Immune Checkpoint Inhibitors. AAPS J. 2020, 22, 132.
- Yu, X.; Gao, R.; Li, Y.; Zeng, C. Regulation of PD-1 in T Cells for Cancer Immunotherapy. Eur. J. Pharmacol. 2020, 881, 173240.
- Kumar, S.; Ghosh, S.; Sharma, G.; Wang, Z.; Kehry, M.R.; Marino, M.H.; Neben, T.Y.; Lu, S.; Luo, S.; Roberts, S.; et al. Preclinical Characterization of Dostarlimab, a Therapeutic Anti-PD-1 Antibody with Potent Activity to Enhance Immune Function in in Vitro Cellular Assays and in Vivo Animal Models. MAbs 2021, 13, 1954136.
- Bowers, P.M.; Neben, T.Y.; Tomlinson, G.L.; Dalton, J.L.; Altobell, L.; Zhang, X.; MacOmber, J.L.; Wu, B.F.; Toobian, R.M.; McConnell, A.D.; et al. Humanization of Antibodies Using Heavy Chain Complementarity-Determining Region 3 Grafting Coupled with in Vitro Somatic Hypermutation. J. Biol. Chem. 2013, 288, 7688–7696.
- Park, U.B.; Jeong, T.J.; Gu, N.; Lee, H.T.; Heo, Y.S. Molecular Basis of PD-1 Blockade by Dostarlimab, the FDA-Approved Antibody for Cancer Immunotherapy. Biochem. Biophys. Res. Commun. 2022, 599, 31–37.
- Lu, S.; Bowsher, R.R.; Clancy, A.; Rosen, A.; Zhang, M.; Yang, Y.; Koeck, K.; Gao, M.; Potocka, E.; Guo, W.; et al. An Integrated Analysis of Dostarlimab Immunogenicity. AAPS J. 2021, 23, 96.
- Sullivan, M.R.; Ugolini, G.S.; Sarkar, S.; Kang, W.; Smith, E.C.; Mckenney, S.; Konry, T. Quantifying the Efficacy of Checkpoint Inhibitors on CD8+ Cytotoxic T Cells for Immunotherapeutic Applications via Single-Cell Interaction. Cell Death Dis. 2020, 11, 979.
- Markham, A. Dostarlimab: First Approval. Drugs 2021, 81, 1213–1219.
- Yi, M.; Zheng, X.; Niu, M.; Zhu, S.; Ge, H.; Wu, K. Combination Strategies with PD-1/PD-L1 Blockade: Current Advances and Future Directions. Mol. Cancer 2022, 21, 28.
- CHMP. Committee for Medicinal Products for Human Use (CHMP) Assessment Report. 2021. Available online: https://www.ema.europa.eu/en/news/meeting-highlights-committee-medicinal-products-human-use-chmp-13-16-december-2021 (accessed on 20 June 2022).
- Yap, T.A.; Bessudo, A.; Hamilton, E.; Sachdev, J.; Patel, M.R.; Rodon, J.; Evilevitch, L.; Duncan, M.; Guo, W.; Kumar, S.; et al. IOLite: Phase 1b Trial of Doublet/Triplet Combinations of Dostarlimab with Niraparib, Carboplatin-Paclitaxel, with or without Bevacizumab in Patients with Advanced Cancer. J. Immunother. Cancer 2022, 10, e003924.
- Melhem, M.; Hanze, E.; Lu, S.; Alskär, O.; Visser, S.; Gandhi, Y. Population Pharmacokinetics and Exposure–Response of Anti-Programmed Cell Death Protein-1 Monoclonal Antibody Dostarlimab in Advanced Solid Tumours. Br. J. Clin. Pharmacol. 2022, 87, 4421–4431.
- Dong, Y.; Sun, Q.; Zhang, X. PD-1 and Its Ligands Are Important Immune Checkpoints in Cancer. Oncotarget 2017, 8, 2171.
- Davda, J.; Declerck, P.; Hu-Lieskovan, S.; Hickling, T.P.; Jacobs, I.A.; Chou, J.; Salek-Ardakani, S.; Kraynov, E. Immunogenicity of Immunomodulatory, Antibody-Based, Oncology Therapeutics. J. Immunother. Cancer 2019, 7, 1–9.
- Sasson, S.C.; Wilkins, L.E.; Watson, R.A.; Jolly, C.; Brain, O.; Klenerman, P.; Olsson-Brown, A.; Fairfax, B.P. Identification of Neutralising Pembrolizumab Anti-Drug Antibodies in Patients with Melanoma. Sci. Rep. 2021, 11, 1–6.
- Oaknin, A.; Gilbert, L.; Tinker, A.V.; Brown, J.; Mathews, C.; Press, J.; Sabatier, R.; O’Malley, D.M.; Samouelian, V.; Boni, V. Safety and antitumor activity of dostarlimab in patients with advanced or recurrent DNA mismatch repair deficient/microsatellite instability-high (dMMR/MSI-H) or proficient/stable (MMRp/MSS) endometrial cancer: Interim results from GARNET—A phase I, single-arm study. J. Immunother. Cancer 2002, 10, e003777.
- Patnaik, A.; Weiss, G.J.; Rasco, D.W.; Blaydorn, L.; Mirabella, A.; Beeram, M.; Guo, W.; Lu, S.; Danaee, H.; McEachern, K.; et al. Safety, Antitumor Activity, and Pharmacokinetics of Dostarlimab, an Anti-PD-1, in Patients with Advanced Solid Tumors: A Dose–Escalation Phase 1 Trial. Cancer Chemother. Pharmacol. 2022, 89, 93–103.
- Han, Y.; Liu, D.; Li, L. PD-1/PD-L1 Pathway: Current Researches in Cancer. Am. J. Cancer Res. 2020, 10, 727.
- Sclafani, F. PD-1 inhibition in metastatic dMMR/MSI-H colorectal cancer. Lancet Oncol. 2017, 18, 1141–1142.
More
