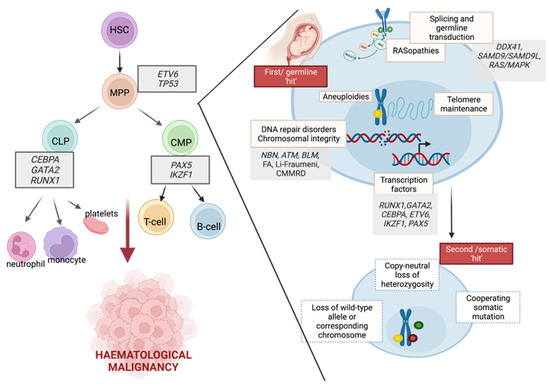
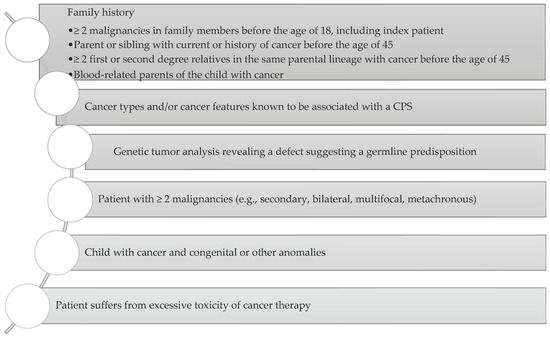
Neoplasms develop as the after effect of an increase of acquired and physical genetic variations in proto-oncogenes, tumour-suppressor genes, and DNA-repair genes (deoxyribonucleic acid). Alfred Knudson, the father of modern cancer genetics and heritable predisposition, hypothesized that “retinoblastoma is a form of cancer caused by two mutational events. In the dominantly inherited form, one mutation is inherited via the germinal cells and the second occurs in somatic cells. In the nonhereditary form, both mutations occur in somatic cells”. The past decade, with large-scale genomic analyses, gave a possibility for better understanding of genetic disorders with predisposition to paediatric cancer. However, the prevalence of cancer predisposition mutations among children is still incompletely known and is reported in 7–10% of paediatric cancer patients. Germline mInteractions between germline and somatic mutations are genetic variants that occur in gametes and are present in every cell of an offspring. a key determinant of cancer development. Cancer predisposition syndrome (CPS) is inherited when a germline mutation is present in the cancer predisposition gene. Somatic mutations can occur in all other cell types and their accumulation can lead to tumourigenesis. Paediatric The early recognition of genetic predispositions for childhood cancers typically have a higher prevalence of germline mutations in cancer predisposition genes when compared with smay provide an opportunity of early detection of neoplasms, followed by presymptomatic mutations. Including the unique combination of somatic alterations on the background of inherited and de novo germline variants during diagnosis is crucial for the understanding of the development of paediatric cancer. Mutations in 60 genes have been associated with clinically relevant autosomal dominant CPSs. The early recognition of genetic predispositions for childhood cancers may provide an opportunity of early detection of neoplasms, followed by presymptomatic genetic testing of relatives, implementation of appropriate clinical procedures (e.g., avoiding radiotherapy), prophylactic surgical resection of organs at risk, or searching for donors of hematopoietic stem cells. Therefore,genetic testing of relatives, implementation of appropriate clinical procedures (e.g., avoiding radiotherapy), prophylactic surgical there is a need for multidisciplinary cooperation between a paediatrician, an oncologist, a geneticist, and a psychologist during the surveillance of families with increased cancer risksection of organs at risk, or searching for donors of hematopoietic stem cells.
- germline mutations
- paediatric cancer
- genetic counselling
1. Syndromes Predisposing to Haematological Malignancies
1.1. DNA Repair Disorders
1.1.1. Ataxia Teleangiectasia (A-T)
1.1.2. Nijmegen Breakage Syndrome (NBS)
1.1.3. Bloom’s Syndrome (BS)
1.1.4. Constitutional Mismatch Repair Deficiency (CMMRD)
1.1.5. Xeroderma Pigmentosum (XP)
1.2. Bone Marrow Failure
1.2.1. Fanconi Anaemia (FA)
1.2.2. Dyskeratosis Congenita (DC)
1.2.3. Shwachman Diamond Syndrome (SDS)
1.2.4. Diamond Blackfan Anemia (DBA)
1.2.5. GATA2 Deficiency
1.3. Immunodeficiencies with Associated or Syndrome Features
1.3.1. Cartilage–Hair Hypoplasia (CHH)
1.3.2. Wiskott-Aldrich Syndrome (WAS)
1.3.3. SAMD9 and SAMD9L Syndromes
1.4. RASopathies
1.4.1. Noonan Syndrome
1.4.2. Neurofibromatosis Type 1 (NF1)
1.4.3. Casitas B-Lineage Lymphoma (CBL-Syndrome)
1.5. Aneuploidies
2. Non-Syndromic Germline Variants Predisposing to Malignancies
2.1. Germline Predisposition without a Pre-Existing Haematological Disorder or Organ Dysfunction
2.1.1. Familial AML with CEBPA Mutation
2.1.2. Familial MDS/AML with Mutated DDX41
2.1.3. PAX-5-Associated Leukaemia Predisposition
2.1.4. IKZF1 Susceptibility to ALL
2.1.5. DICER1 Syndrome
2.1.6. Li-Fraumeni Syndrome (LFS)
2.2. Germ Line Predisposition with a Pre-Existing Haematological Disorder
2.2.1. ETV6-Related Familial Neutropenia (Thrombocytopenia, Type 5)
2.2.2. Familial Platelet Disorder with Predisposition for AML
2.2.3. ANKRD26-Related Thrombocytopenia
3. The Importance of Identifying Genetic Predispositions to Paediatric Cancers
4. Incorporating Molecular Findings into Clinic
4.1. Multidisciplinary Cooperation
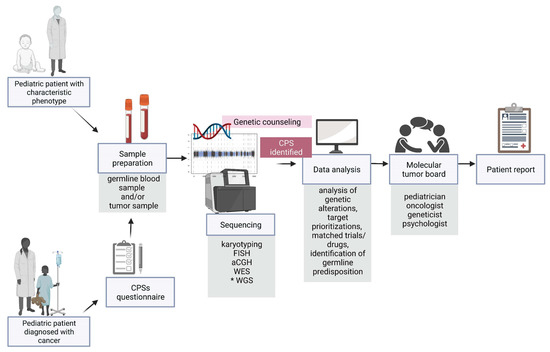
4.2. The Impact of Diagnosis of Germline Variants Predisposing to Malignancies on Clinical Management
References
- Seemanova, E.; Varon, R.; Vejvalka, J.; Jarolim, P.; Seeman, P.; Chrzanowska, K.H.; Digweed, M.; Resnick, I.; Kremensky, I.; Saar, K.; et al. The Slavic NBN Founder Mutation: A Role for Reproductive Fitness? PLoS ONE 2016, 11, e0167984.
- Wolska-Kusnierz, B.; Pastorczak, A.; Fendler, W.; Wakulinska, A.; Dembowska-Baginska, B.; Heropolitanska-Pliszka, E.; Piątosa, B.; Pietrucha, B.; Kałwak, K.; Ussowicz, M.; et al. Hematopoietic Stem Cell Transplantation Positively Affects the Natural History of Cancer in Nijmegen Breakage Syndrome. Clin. Cancer Res. 2020, 27, 575–584.
- Arber, D.A.; Orazi, A.; Hasserjian, R.; Thiele, J.; Borowitz, M.J.; Le Beau, M.M.; Bloomfield, C.D.; Cazzola, M.; Vardiman, J.W. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016, 127, 2391–2405.
- Godley, L.; Shimamura, A. Genetic predisposition to hematologic malignancies: Management and surveillance. Blood 2017, 130, 424–432.
- Mangaonkar, A.A.; Patnaik, M.M. Hereditary Predisposition to Hematopoietic Neoplasms: When Bloodline Matters for Blood Cancers. Mayo Clin. Proc. 2020, 95, 1482–1498.
- Bomken, S.; van der Werff Ten Bosch, J.; Attarbaschi, A.; Bacon, C.; Borkhardt, A.; Boztug, K.; Fischer, U.; Hauck, F.; Kuiper, R.; Lammens, T.; et al. Current Understanding and Future Research Priorities in Malignancy Associated With Inborn Errors of Immunity and DNA Repair Disorders: The Perspective of an Interdisciplinary Working Group. Front. Immunol. 2018, 9, 2912.
- Szmyd, B.; Mlynarski, W.; Pastorczak, A. Genetic predisposition to lymphomas: Overview of rare syndromes and inherited familial variants. Mutat. Res./Rev. Mutat. Res. 2021, 788, 108386.
- Suarez, F.; Mahlaoui, N.; Canioni, D.; Andriamanga, C.; Dubois d’Enghien, C.; Brousse, N.; Jais, J.; Fischer, A.; Hermine, O.; Stoppa-Lyonnet, D. Incidence, Presentation, and Prognosis of Malignancies in Ataxia-Telangiectasia: A Report From the French National Registry of Primary Immune Deficiencies. J. Clin. Oncol. 2015, 33, 202–208.
- Rothblum-Oviatt, C.; Wright, J.; Lefton-Greif, M.; McGrath-Morrow, S.; Crawford, T.; Lederman, H. Ataxia telangiectasia: A review. Orphanet J. Rare Dis. 2016, 11, 159.
- van Os, N.; Jansen, A.; van Deuren, M.; Haraldsson, A.; van Driel, N.; Etzioni, A.; van der Flier, M.; Haaxma, C.; Morio, T.; Rawat, A.; et al. Ataxia-telangiectasia: Immunodeficiency and survival. Clin. Immunol. 2017, 178, 45–55.
- Gathmann, B.; Mahlaoui, N.; Gérard, L.; Oksenhendler, E.; Warnatz, K.; Schulze, I.; Kindle, G.; Kuijpers, T.; van Beem, R.; Guzman, D.; et al. Clinical picture and treatment of 2212 patients with common variable immunodeficiency. J. Allergy Clin. Immunol. 2014, 134, 116–126.e11.
- Chrzanowska, K.; Gregorek, H.; Dembowska-Bagińska, B.; Kalina, M.; Digweed, M. Nijmegen breakage syndrome (NBS). Orphanet J. Rare Dis. 2012, 7, 13.
- Deripapa, E.; Balashov, D.; Rodina, Y.; Laberko, A.; Myakova, N.; Davydova, N.; Gordukova, M.; Abramov, D.; Pay, G.; Shelikhova, L.; et al. Prospective Study of a Cohort of Russian Nijmegen Breakage Syndrome Patients Demonstrating Predictive Value of Low Kappa-Deleting Recombination Excision Circle (KREC) Numbers and Beneficial Effect of Hematopoietic Stem Cell Transplantation (HSCT). Front. Immunol. 2017, 8, 807.
- Piatosa, B.; Wolska-Kuśnierz, B.; Tkaczyk, K.; Heropolitanska-Pliszka, E.; Grycuk, U.; Wakulinska, A.; Gregorek, H. T Lymphocytes in Patients With Nijmegen Breakage Syndrome Demonstrate Features of Exhaustion and Senescence in Flow Cytometric Evaluation of Maturation Pathway. Front. Immunol. 2020, 11, 1319.
- Maciejczyk, M.; Heropolitanska-Pliszka, E.; Pietrucha, B.; Sawicka-Powierza, J.; Bernatowska, E.; Wolska-Kusnierz, B.; Pac, M.; Car, H.; Zalewska, A.; Mikoluc, B. Antioxidant Defense, Redox Homeostasis, and Oxidative Damage in Children with Ataxia Telangiectasia and Nijmegen Breakage Syndrome. Front. Immunol. 2019, 10, 2322.
- Walsh, M.; Chang, V.; Kohlmann, W.; Scott, H.; Cunniff, C.; Bourdeaut, F.; Molenaar, J.; Porter, C.; Sandlund, J.; Plon, S.; et al. Recommendations for Childhood Cancer Screening and Surveillance in DNA Repair Disorders. Clin. Cancer Res. 2017, 23, e23–e31.
- Cunniff, C.; Bassetti, J.; Ellis, N. Bloom’s Syndrome: Clinical Spectrum, Molecular Pathogenesis, and Cancer Predisposition. Mol. Syndromol. 2016, 8, 4–23.
- Ababou, M. Bloom syndrome and the underlying causes of genetic instability. Mol. Genet. Metab. 2021, 133, 35–48.
- Flanagan, M.; Cunniff, C.M. Bloom Syndrome. In GeneReviews®; Adam, M.P., Ed.; University of Washington: Seattle, WA, USA, 2006.
- Bakry, D.; Aronson, M.; Durno, C.; Rimawi, H.; Farah, R.; Alharbi, Q.; Alharbi, M.; Shamvil, A.; Ben-Shachar, S.; Mistry, M.; et al. Genetic and clinical determinants of constitutional mismatch repair deficiency syndrome: Report from the constitutional mismatch repair deficiency consortium. Eur. J. Cancer 2014, 50, 987–996.
- Tabori, U.; Hansford, J.; Achatz, M.; Kratz, C.; Plon, S.; Frebourg, T.; Brugières, L. Clinical Management and Tumor Surveillance Recommendations of Inherited Mismatch Repair Deficiency in Childhood. Clin. Cancer Res. 2017, 23, e32–e37.
- Wimmer, K.; Rosenbaum, T.; Messiaen, L. Connections between constitutional mismatch repair deficiency syndrome and neurofibromatosis type. Clin. Genet. 2017, 91, 507–519.
- Ripperger, T.; Schlegelberger, B. Acute lymphoblastic leukemia and lymphoma in the context of constitutional mismatch repair deficiency syndrome. Eur. J. Med Genet. 2016, 59, 133–142.
- Durno, C.; Sherman, P.; Aronson, M.; Malkin, D.; Hawkins, C.; Bakry, D.; Bouffet, E.; Gallinger, S.; Pollett, A.; Campbell, B.; et al. Phenotypic and genotypic characterisation of biallelic mismatch repair deficiency (BMMR-D) syndrome. Eur. J. Cancer 2015, 51, 977–983.
- Guerrini-Rousseau, L.; Varlet, P.; Colas, C.; Andreiuolo, F.; Bourdeaut, F.; Dahan, K.; Devalck, C.; Faure-Conter, C.; Genuardi, M.; Goldberg, Y.; et al. Constitutional mismatch repair deficiency–associated brain tumors: Report from the European C4CMMRD consortium. Neuro Oncol. Adv. 2019, 1, 1–13.
- Martens, M.; Emmert, S.; Boeckmann, L. Xeroderma Pigmentosum: Gene Variants and Splice Variants. Genes 2021, 12, 1173.
- Lehmann, J.; Seebode, C.; Martens, M.; Emmert, S. Xeroderma pigmentosum—Facts and Perspectives. Aktuelle Dermatol. 2018, 44, 232–236.
- Martens, M.C.; Emmert, S.; Boeckmann, L. Sunlight, Vitamin D, and Xeroderma Pigmentosum. Adv. Exp. Med. Biol. 2020, 1268, 319–331.
- Kraemer, K.H.; Lee, M.M.; Andrews, A.D.; Lambert, W.C. The role of sunlight and DNA repair in melanoma and nonmelanoma skin cancer. The xeroderma pigmentosum paradigm. Arch. Dermatol. 1994, 130, 1018–1021.
- Seif, A.E. Pediatric leukemia predisposition syndromes: Clues to understanding leukemogenesis. Cancer Genet. 2011, 204, 227–244.
- Taylor, A.; Rothblum-Oviatt, C.; Ellis, N.; Hickson, I.; Meyer, S.; Crawford, T.; Smogorzewska, A.; Pietrucha, B.; Weemaes, C.; Stewart, G. Chromosome instability syndromes. Nat. Rev. Dis. Primers 2019, 5, 64.
- Alter, B. Fanconi anemia and the development of leukemia. Best Pract. Res. Clin. Haematol. 2014, 27, 214–221.
- Vulliamy, T.; Marrone, A.; Szydlo, R.; Walne, A.; Mason, P.; Dokal, I. Disease anticipation is associated with progressive telomere shortening in families with dyskeratosis congenita due to mutations in TERC. Nat. Genet. 2004, 36, 447–449.
- Garofola, C.; Nassereddin, A.; Gross, G.P. Dyskeratosis Congenita. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK507710/ (accessed on 2 July 2022).
- AlSabbagh, M. Dyskeratosis congenita: A literature review. J. Dtsch. Dermatol. Ges. 2020, 18, 943–967.
- Bezzerri, V.; Cipolli, M. Shwachman-Diamond Syndrome: Molecular Mechanisms and Current Perspectives. Mol. Diagn. Ther. 2018, 23, 281–290.
- Nelson, A.; Myers, K. Shwachman-Diamond Syndrome. Available online: https://www.ncbi.nlm.nih.gov/books/NBK1756/ (accessed on 2 April 2022).
- Myers, K.C.; Furutani, E.; Weller, E.; Siegele, B.; Galvin, A.; Arsenault, V.; Alter, B.P.; Boulad, F.; Bueso-Ramos, C.; Burroughs, L.; et al. Clinical features and outcomes of patients with Shwachman-Diamond syndrome and myelodysplastic syndrome or acute myeloid leukaemia: A multicentre, retrospective, cohort study. Lancet Haematol. 2020, 7, e238–e246.
- Shimamura, A.; Alter, B.P. Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev. 2010, 24, 101–122.
- Da Costa, L.; Leblanc, T.; Mohandas, N. Diamond-Blackfan anemia. Blood 2020, 136, 1262–1273.
- Bartels, M.; Bierings, M. How I manage children with Diamond-Blackfan anaemia. Br. J. Haematol. 2018, 184, 123–133.
- Vlachos, A.; Rosenberg, P.; Atsidaftos, E.; Alter, B.; Lipton, J. Incidence of neoplasia in Diamond Blackfan anemia: A report from the Diamond Blackfan Anemia Registry. Blood 2012, 119, 3815–3819.
- Babushok, D.; Bessler, M.; Olson, T. Genetic predisposition to myelodysplastic syndrome and acute myeloid leukemia in children and young adults. Leuk. Lymphoma 2015, 57, 520–536.
- Klco, J.; Mullighan, C. Advances in germline predisposition to acute leukaemias and myeloid neoplasms. Nat. Rev. Cancer 2020, 21, 122–137.
- Porter, C.; Druley, T.; Erez, A.; Kuiper, R.; Onel, K.; Schiffman, J.; Wolfe Schneider, K.; Scollon, S.; Scott, H.; Strong, L.; et al. Recommendations for Surveillance for Children with Leukemia-Predisposing Conditions. Clin. Cancer Res. 2017, 23, e14–e22.
- Vakkilainen, S.; Taskinen, M.; Mäkitie, O. Immunodeficiency in cartilage-hair hypoplasia: Pathogenesis, clinical course and management. Scand. J. Immunol. 2020, 92, e12913.
- Makitie, O. Cartilage-hair hypoplasia in Finland: Epidemiological and genetic aspects of 107 patients. J. Med Genet. 1992, 29, 652–655.
- Taskinen, M.; Ranki, A.; Pukkala, E.; Jeskanen, L.; Kaitila, I.; Mäkitie, O. Extended follow-up of the Finnish cartilage-hair hypoplasia cohort confirms high incidence of non-Hodgkin lymphoma and basal cell carcinoma. Am. J. Med Genet. Part A 2008, 146A, 2370–2375.
- Candotti, F. Clinical Manifestations and Pathophysiological Mechanisms of the Wiskott-Aldrich Syndrome. J. Clin. Immunol. 2017, 38, 13–27.
- Leechawengwongs, E.; Shearer, W. Lymphoma complicating primary immunodeficiency syndromes. Curr. Opin. Hematol. 2012, 19, 305–312.
- Duan, L.; Grunebaum, E. Hematological Malignancies Associated With Primary Immunodeficiency Disorders. Clin. Immunol. 2018, 194, 46–59.
- Sahoo, S.; Kozyra, E.; Wlodarski, M. Germline predisposition in myeloid neoplasms: Unique genetic and clinical features of GATA2 deficiency and SAMD9/SAMD9L syndromes. Best Pract. Res. Clin. Haematol. 2020, 33, 101197.
- Chen, D.; Below, J.; Shimamura, A.; Keel, S.; Matsushita, M.; Wolff, J.; Sul, Y.; Bonkowski, E.; Castella, M.; Taniguchi, T.; et al. Ataxia-Pancytopenia Syndrome Is Caused by Missense Mutations in SAMD9L. Am. J. Hum. Genet. 2016, 98, 1146–1158.
- Narumi, S.; Amano, N.; Ishii, T.; Katsumata, N.; Muroya, K.; Adachi, M.; Toyoshima, K.; Tanaka, Y.; Fukuzawa, R.; Miyako, K.; et al. SAMD9 mutations cause a novel multisystem disorder, MIRAGE syndrome, and are associated with loss of chromosome. Nat. Genet. 2016, 48, 792–797.
- Roberts, A.E.; Allanson, J.E.; Tartaglia, M.; Gelb, B.D. Noonan syndrome. Lancet 2013, 381, 333–342.
- Roberts, A. Noonan Syndrome. Available online: https://www.ncbi.nlm.nih.gov/books/NBK1124/ (accessed on 2 April 2022).
- Villani, A.; Greer, M.; Kalish, J.; Nakagawara, A.; Nathanson, K.; Pajtler, K.; Pfister, S.; Walsh, M.; Wasserman, J.; Zelley, K.; et al. Recommendations for Cancer Surveillance in Individuals with RASopathies and Other Rare Genetic Conditions with Increased Cancer Risk. Clin. Cancer Res. 2017, 23, e83–e90.
- Miller, D.; Freedenberg, D.; Schorry, E.; Ullrich, N.; Viskochil, D.; Korf, B.; Chen, E.; Trotter, T.; Berry, S.; Burke, L.; et al. Health Supervision for Children With Neurofibromatosis Type. Pediatrics 2019, 143, e20190660.
- Sur, M.; Armat, I.; Sur, G.; Pop, D.; Samasca, G.; Lupan, I.; Timis, T.; Florian, I.; Sur, D. Neurofibromatosis in Children: Actually and Perspectives. Children 2022, 9, 40.
- Pinti, E.; Nemeth, K.; Staub, K.; Lengyel, A.; Fekete, G.; Haltrich, I. Diagnostic difficulties and possibilities of NF1-like syndromes in childhood. BMC Pediatr. 2021, 21, 331.
- Legius, E.; Messiaen, L.; Wolkenstein, P.; Pancza, P.; Avery, R.; Berman, Y.; Blakeley, J.; Babovic-Vuksanovic, D.; Cunha, K.; Ferner, R.; et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: An international consensus recommendation. Genet. Med. 2021, 23, 1506–1513.
- Niemeyer, C. JMML genomics and decisions. Hematology 2018, 2018, 307–312.
- Evans, D.; Salvador, H.; Chang, V.; Erez, A.; Voss, S.; Schneider, K.; Scott, H.; Plon, S.; Tabori, U. Cancer and Central Nervous System Tumor Surveillance in Pediatric Neurofibromatosis. Clin. Cancer Res. 2017, 23, e46–e53.
- Bülow, L.; Lissewski, C.; Bressel, R.; Rauch, A.; Stark, Z.; Zenker, M.; Bartsch, O. Hydrops, fetal pleural effusions and chylothorax in three patients with CBL mutations. Am. J. Med Genet. Part A 2015, 167A, 394–399.
- Naramura, M.; Nadeau, S.; Mohapatra, B.; Ahmad, G.; Mukhopadhyay, C.; Sattler, M.; Raja, S.M.; Natarajan, A.; Band, V.; Band, H. Mutant Cbl proteins as oncogenic drivers in myeloproliferative disorders. Oncotarget 2011, 2, 245–250.
- Martinelli, S.; De Luca, A.; Stellacci, E.; Rossi, C.; Checquolo, S.; Lepri, F.; Caputo, V.; Silvano, M.; Buscherini, F.; Consoli, F.; et al. Heterozygous germline mutations in the CBL tumor-suppressor gene cause a Noonan syndrome-like phenotype. Am. J. Hum. Genet. 2010, 87, 250–257.
- Cardoso, L.; Galán-Gómez, V.; Corral-Sánchez, M.; Pérez-Martínez, A.; Riesco, S.; Isidoro-García, M.; Escudero, A. Juvenile myelomonocytic leukemia in CBL syndrome associated with germline splice-site mutations: Two case reports and a literature review. Clin. Case Rep. 2021, 9, e04260.
- Roberts, I.; Izraeli, S. Haematopoietic development and leukaemia in Down syndrome. Br. J. Haematol. 2014, 167, 587–599.
- Zwaan, C.; Reinhardt, D.; Hitzler, J.; Vyas, P. Acute Leukemias in Children with Down Syndrome. Pediatr. Clin. N. Am. 2008, 55, 53–70.
- Davidsson, J.; Veerla, S.; Johansson, B. Constitutional trisomy 8 mosaicism as a model for epigenetic studies of aneuploidy. Epigenet. Chromatin 2013, 6, 18.
- Rojas, A.; Vo, D.; Mwangi, L.; Rehman, S.; Peiris, A. Oncologic manifestations of Klinefelter syndrome. Hormones 2020, 19, 497–504.
- Ji, J.; Zöller, B.; Sundquist, J.; Sundquist, K. Risk of solid tumors and hematological malignancy in persons with Turner and Klinefelter syndromes: A national cohort study. Int. J. Cancer 2016, 139, 754–758.
- Rau, R.; Carroll, A.; Heerema, N.; Arland, L.; Carroll, W.; Winick, N.; Raetz, E.; Loh, M.; Yang, W.; Relling, M.; et al. Klinefelter syndrome and 47,XYY syndrome in children with B cell acute lymphoblastic leukaemia. Br. J. Haematol. 2016, 179, 843–846.
- Pathak, A.; Seipel, K.; Pemov, A.; Dewan, R.; Brown, C.; Ravichandran, S.; Luke, B.; Malasky, M.; Suman, S.; Yeager, M.; et al. Whole exome sequencing reveals a C-terminal germline variant in CEBPA-associated acute myeloid leukemia: 45-year follow up of a large family. Haematologica 2015, 101, 846–852.
- Tawana, K.; Rio-Machin, A.; Preudhomme, C.; Fitzgibbon, J. Familial CEBPA-mutated acute myeloid leukemia. Semin. Hematol. 2017, 54, 87–93.
- Pabst, T.; Eyholzer, M.; Haefliger, S.; Schardt, J.; Mueller, B.U. Somatic CEBPA mutations are a frequent second event in families with germline CEBPA mutations and familial acute myeloid leukemia. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008, 26, 5088–5093.
- Feurstein, S.; Drazer, M.; Godley, L. Genetic predisposition to leukemia and other hematologic malignancies. Semin. Oncol. 2016, 43, 598–608.
- Lewinsohn, M.; Brown, A.; Weinel, L.; Phung, C.; Rafidi, G.; Lee, M.; Schreiber, A.; Feng, J.; Babic, M.; Chong, C.; et al. Novel germ line DDX41 mutations define families with a lower age of MDS/AML onset and lymphoid malignancies. Blood 2016, 127, 1017–1023.
- Polprasert, C.; Schulze, I.; Sekeres, M.; Makishima, H.; Przychodzen, B.; Hosono, N.; Singh, J.; Padgett, R.; Gu, X.; Phillips, J.; et al. Inherited and Somatic Defects in DDX41 in Myeloid Neoplasms. Cancer Cell 2015, 27, 658–670.
- Churchman, M.; Qian, M.; te Kronnie, G.; Zhang, R.; Yang, W.; Zhang, H.; Lana, T.; Tedrick, P.; Baskin, R.; Verbist, K.; et al. Germline Genetic IKZF1 Variation and Predisposition to Childhood Acute Lymphoblastic Leukemia. Cancer Cell 2018, 33, 937–948.e8.
- Foulkes, W.D.; Bahubeshi, A.; Hamel, N.; Pasini, B.; Asioli, S.; Baynam, G.; Choong, C.S.; Charles, A.; Frieder, R.P.; Dishop, M.K.; et al. Extending the phenotypes associated with DICER1 mutations. Hum. Mutat. 2011, 32, 1381–1384.
- Kuhlen, M.; Hönscheid, A.; Schemme, J.; Merz, H.; Mauz-Körholz, C.; Borkhardt, A.; Troeger, A. Hodgkin lymphoma as a novel presentation of familial DICER1 syndrome. Eur. J. Pediatr. 2015, 175, 593–597.
- Schultz, K.; Rednam, S.P.; Kamihara, J.; Doros, L.; Achatz, M.I.; Wasserman, J.D.; Diller, L.R.; Brugières, L.; Druker, H.; Schneider, K.A.; et al. PTEN, DICER1, FH, and Their Associated Tumour Susceptibility Syndromes: Clinical Features, Genetics, and Surveillance Recommendations in Childhood. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, e76–e82.
- Farouk Sait, S.; Walsh, M.; Karajannis, M. Genetic syndromes predisposing to pediatric brain tumors. Neuro-Oncol. Pract. 2021, 8, 375–390.
- Kratz, C.P.; Steinke-Lange, V.; Spier, I.; Aretz, S.; Schröck, E.; Holinski-Feder, E. Overview of the Clinical Features of Li-Fraumeni Syndrome and the Current European ERN GENTURIS Guideline. Geburtshilfe Frauenheilkd. 2021, 82, 42–49.
- Frebourg, T.; Bajalica Lagercrantz, S.; Oliveira, C.; Magenheim, R.; Evans, D.G.; European Reference Network GENTURIS. Guidelines for the Li-Fraumeni and heritable TP53-related cancer syndromes. Eur. J. Hum. Genet. EJHG 2020, 28, 1379–1386.
- Bougeard, G.; Renaux-Petel, M.; Flaman, J.; Charbonnier, C.; Fermey, P.; Belotti, M.; Gauthier-Villars, M.; Stoppa-Lyonnet, D.; Consolino, E.; Brugières, L.; et al. Revisiting Li-Fraumeni Syndrome From TP53 Mutation Carriers. J. Clin. Oncol. 2015, 33, 2345–2352.
- Kratz, C.; Freycon, C.; Maxwell, K.; Nichols, K.; Schiffman, J.; Evans, D.; Achatz, M.; Savage, S.; Weitzel, J.; Garber, J.; et al. Analysis of the Li-Fraumeni Spectrum Based on an International Germline TP53 Variant Data Set. JAMA Oncol. 2021, 7, 1800.
- Ripperger, T.; Bielack, S.; Borkhardt, A.; Brecht, I.; Burkhardt, B.; Calaminus, G.; Debatin, K.; Deubzer, H.; Dirksen, U.; Eckert, C.; et al. Childhood cancer predisposition syndromes-A concise review and recommendations by the Cancer Predisposition Working Group of the Society for Pediatric Oncology and Hematology. Am. J. Med Genet. Part A 2017, 173, 1017–1037.
- Feurstein, S.; Godley, L. Germline ETV6 mutations and predisposition to hematological malignancies. Int. J. Hematol. 2017, 106, 189–195.
- Papaemmanuil, E.; Rapado, I.; Li, Y.; Potter, N.; Wedge, D.; Tubio, J.; Alexandrov, L.; Van Loo, P.; Cooke, S.; Marshall, J.; et al. RAG-mediated recombination is the predominant driver of oncogenic rearrangement in ETV6-RUNX1 acute lymphoblastic leukemia. Nat. Genet. 2014, 46, 116–125.
- Bluteau, D.; Balduini, A.; Balayn, N.; Currao, M.; Nurden, P.; Deswarte, C.; Leverger, G.; Noris, P.; Perrotta, S.; Solary, E.; et al. Thrombocytopenia-associated mutations in the ANKRD26 regulatory region induce MAPK hyperactivation. J. Clin. Investig. 2014, 124, 580–591.
- NSGC. Policy, Research and Publications. Professional Status Survey. Available online: https://www.nsgc.org/Policy-Research-and-Publications/Professional-Status-Survey (accessed on 2 April 2022).
- Jongmans, M.C.; Loeffen, J.L.; Waanders, E.; Hoogerbrugge, P.M.; Ligtenberg, M.J.; Kuiper, R.P.; Hoogerbrugge, N. Recognition of genetic predisposition in pediatric cancer patients: An easy-to-use selection tool. Eur. J. Med. Genet. 2016, 59, 116–125.
- Newman, S.; Nakitandwe, J.; Kesserwan, C.A.; Azzato, E.M.; Wheeler, D.A.; Rusch, M.; Shurtleff, S.; Hedges, D.J.; Hamilton, K.V.; Foy, S.G.; et al. Genomes for Kids: The Scope of Pathogenic Mutations in Pediatric Cancer Revealed by Comprehensive DNA and RNA Sequencing. Cancer Discov. 2021, 11, 3008–3027.
- Surrey, L.; MacFarland, S.; Chang, F.; Cao, K.; Rathi, K.; Akgumus, G.; Gallo, D.; Lin, F.; Gleason, A.; Raman, P.; et al. Clinical utility of custom-designed NGS panel testing in pediatric tumors. Genome Med. 2019, 11, 32.
- Langenberg, K.; Looze, E.J.; Molenaar, J.J. The Landscape of Pediatric Precision Oncology: Program Design, Actionable Alterations, and Clinical Trial Development. Cancers 2021, 13, 4324.
- Marks, L.; Oberg, J.; Pendrick, D.; Sireci, A.; Glasser, C.; Coval, C.; Zylber, R.; Chung, W.; Pang, J.; Turk, A.; et al. Precision Medicine in Children and Young Adults with Hematologic Malignancies and Blood Disorders: The Columbia University Experience. Front. Pediatr. 2017, 5, 265.
- Clarke, R.; Van den Bruel, A.; Bankhead, C.; Mitchell, C.; Phillips, B.; Thompson, M. Clinical presentation of childhood leukaemia: A systematic review and meta-analysis. Arch. Dis. Child. 2016, 101, 894–901.
- Cortelazzo, S.; Ferreri, A.; Hoelzer, D.; Ponzoni, M. Lymphoblastic lymphoma. Crit. Rev. Oncol. Hematol. 2017, 113, 304–317.
- Kratz, C.; Achatz, M.; Brugières, L.; Frebourg, T.; Garber, J.; Greer, M.; Hansford, J.; Janeway, K.; Kohlmann, W.; McGee, R.; et al. Cancer Screening Recommendations for Individuals with Li-Fraumeni Syndrome. Clin. Cancer Res. 2017, 23, e38–e45.
- Villani, A.; Shore, A.; Wasserman, J.; Stephens, D.; Kim, R.; Druker, H.; Gallinger, B.; Naumer, A.; Kohlmann, W.; Novokmet, A.; et al. Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: 11 year follow-up of a prospective observational study. Lancet Oncol. 2016, 17, 1295–1305.
